AUGUST 2013 | Volume 36 • Number 8 619 n trauma update Section Editors: David J. Hak, MD, MBA & Philip F. Stahel, MD A cute compartment syn- drome remains one of the few true emergencies in ortho- pedic traumatology. It is a con- dition in which increased com- partment pressure within a con- fined space compromises the circulation and viability of the tissues within that space. In the orthopedic trauma setting, com- partment syndrome is observed in both acute open and closed fracture settings, most often in the long bones of the forearm and leg. 1 It can also be present in the absence of fracture follow- ing a severe soft tissue injury. Acute compartment syndrome is important for orthopedic sur- geons to recognize because its diagnosis is not always straight- forward, and it has a high risk of associated limb morbidity if left undiagnosed or untreated. Early fasciotomy is of the utmost importance because definitive treatment through early and correct diagnosis is key in preventing morbid- ity. 2 Classic cardinal signs for acute compartment syndrome have demonstrated less than optimal sensitivity but excel- lent specificity; as Ulmer 3 stated: “these findings sug- gest that the clinical features of compartment syndrome of the lower leg are more useful by their absence in excluding the diagnosis than they are when present in confirming the diagnosis.” Despite the ability to inva- sively measure compartment pressures, the diagnosis of acute compartment syndrome, which is an evolving patholog- ic process, is often based on the assessment of all related clinical factors. In this article, the authors review the patho- physiology, anatomy, diagno- sis, and treatment of this po- tentially devastating condition. PATHOPHYSIOLOGY When inflammation devel- ops following trauma, the lim- iting envelope surrounding in- dividual muscle compartments leads to increased pressures that, if untreated, will eventu- ally produce a final common pathway of cellular anoxia and tissue damage. 4 The limiting envelope is most often the fas- cia but can be the epimysium 5 or skin. 1 Fascial compartments are inelastic and do not change in size after development is complete, but the muscle within is not limited in growth. Patients with increased muscle mass have less space for swell- ing after muscle injury. 6 The basic principle of isch- emia stems from inadequate perfusion relative to demand. The ischemia produced by compartment syndrome is a self-perpetuating cycle involv- ing increasing edema, pres- sure, and ischemia. 7 Muscles and nerves tolerate ischemia for up to 4 hours with limited sequelae; however, 8 hours of ischemia results in irreversible damage. 8 Fasciotomy allows for normalization of capillary blood flow and clears the lo- cal accumulation of anaerobic metabolite build-up via res- Abstract: Acute compartment syndrome remains a challeng- ing problem for orthopedic surgeons because its diagnosis is not always straightforward and it has a high risk of associated limb morbidity if left undiagnosed or untreated. Failure to di- agnose and treat acute compartment syndrome is one of the most common causes of successful medical liability claims. The authors review the current literature concerning the diag- nosis of acute compartment syndrome and discuss new non- invasive technologies that may allow for earlier and more ac- curate diagnosis of impending acute compartment syndrome. The authors are from the Department of Orthopaedics and Rehabilitation (NM), University of Vermont College of Medicine, Burlington, Vermont; and the Department of Orthopaedics (HG, CH, JH, DH, CM), Denver Health Medical Center, Denver, Colorado. The authors have no relevant financial relationships to disclose. Correspondence should be addressed to: Cyril Mauffrey, MD, FRCS, Department of Orthopaedics, Denver Health Medical Center, 777 Bannock St, Denver, CO 80204 ([email protected]). doi: 10.3928/01477447-20130724-07 Acute Lower-leg Compartment Syndrome Nathan Mauser, MD; Hannah Gissel, BA; Corey Henderson, MS; Jiandong Hao, MD, PhD; David Hak, MD, MBA; Cyril Mauffrey, MD, FRCS

Acute Lower-leg Compartment Syndrome
Jan 16, 2023
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
AUGUST 2013 | Volume 36 • Number 8 619
n trauma update Section Editors: David J. Hak, MD, MBA & Philip F. Stahel, MD
Acute compartment syn- drome remains one of the
few true emergencies in ortho- pedic traumatology. It is a con- dition in which increased com- partment pressure within a con- fined space compromises the circulation and viability of the tissues within that space. In the orthopedic trauma setting, com- partment syndrome is observed in both acute open and closed
fracture settings, most often in the long bones of the forearm and leg.1 It can also be present in the absence of fracture follow- ing a severe soft tissue injury. Acute compartment syndrome is important for orthopedic sur- geons to recognize because its diagnosis is not always straight- forward, and it has a high risk of associated limb morbidity if left undiagnosed or untreated.
Early fasciotomy is of the utmost importance because definitive treatment through early and correct diagnosis is key in preventing morbid- ity.2 Classic cardinal signs for acute compartment syndrome have demonstrated less than optimal sensitivity but excel- lent specificity; as Ulmer3 stated: “these findings sug- gest that the clinical features of compartment syndrome of the lower leg are more useful by their absence in excluding the diagnosis than they are when present in confirming the diagnosis.”
Despite the ability to inva- sively measure compartment pressures, the diagnosis of acute compartment syndrome, which is an evolving patholog- ic process, is often based on the assessment of all related clinical factors. In this article, the authors review the patho- physiology, anatomy, diagno- sis, and treatment of this po- tentially devastating condition.
PathoPhysiology When inflammation devel-
ops following trauma, the lim-
iting envelope surrounding in- dividual muscle compartments leads to increased pressures that, if untreated, will eventu- ally produce a final common pathway of cellular anoxia and tissue damage.4 The limiting envelope is most often the fas- cia but can be the epimysium5 or skin.1 Fascial compartments are inelastic and do not change in size after development is complete, but the muscle within is not limited in growth. Patients with increased muscle mass have less space for swell- ing after muscle injury.6
The basic principle of isch- emia stems from inadequate perfusion relative to demand. The ischemia produced by compartment syndrome is a self-perpetuating cycle involv- ing increasing edema, pres- sure, and ischemia.7 Muscles and nerves tolerate ischemia for up to 4 hours with limited sequelae; however, 8 hours of ischemia results in irreversible damage.8 Fasciotomy allows for normalization of capillary blood flow and clears the lo- cal accumulation of anaerobic metabolite build-up via res-
Abstract: Acute compartment syndrome remains a challeng- ing problem for orthopedic surgeons because its diagnosis is not always straightforward and it has a high risk of associated limb morbidity if left undiagnosed or untreated. Failure to di- agnose and treat acute compartment syndrome is one of the most common causes of successful medical liability claims. The authors review the current literature concerning the diag- nosis of acute compartment syndrome and discuss new non- invasive technologies that may allow for earlier and more ac- curate diagnosis of impending acute compartment syndrome.
The authors are from the Department of Orthopaedics and Rehabilitation (NM), University of Vermont College of Medicine, Burlington, Vermont; and the Department of Orthopaedics (HG, CH, JH, DH, CM), Denver Health Medical Center, Denver, Colorado.
The authors have no relevant financial relationships to disclose. Correspondence should be addressed to: Cyril Mauffrey, MD, FRCS,
Department of Orthopaedics, Denver Health Medical Center, 777 Bannock St, Denver, CO 80204 ([email protected]).
doi: 10.3928/01477447-20130724-07
Acute Lower-leg Compartment Syndrome Nathan Mauser, MD; Hannah Gissel, BA; Corey Henderson, MS; Jiandong Hao, MD, PhD; David Hak, MD, MBA; Cyril Mauffrey, MD, FRCS
620 ORTHOPEDICS | Healio.com/Orthopedics
n trauma update
toration of physiologic pres- sures within the compartment. Following decompression, if early enough in the cycle, cells may become edematous and histologically will appear to exhibit injury. However, nor- mal morphology is returned after 1 week.9,10
Several hypotheses exist regarding the pathophysiology of compartment syndrome, and it is likely that this syndrome is more complex than the cur- rent state of knowledge. The most widely accepted hypoth- esis is the arteriovenous pres- sure gradient theory, in which reduction of this gradient and decreased microvascular flow through the capillaries perpetu- ates edema and pressure, lead- ing to increased ischemia.1,7 Initially, and most often in the acute setting, an increase in lo- cal pressure and edema stem from the insult. Subsequently, an increase in local intravenous pressure occurs, as well as a reduction in arteriovenous gra- dient, and leads to a local de- crease in perfusion.
Endothelial cells sustain damage via anoxia and in- creased vessel wall permeabil- ity.11 In addition to the decrease in perfusion, the decreased venous return increases tis- sue edema. Lymphatic drain- age can only compensate to a point and will fail under high pressure.12 It is the venous flow and this local stasis that perpetuate the edema and el- evate compartment pressures. The pressures then increase to equal the diastolic blood pres- sure, and local tissue perfusion ceases.13,14 Once muscle necro- sis begins and cytolysis occurs,
the osmotically active contents of the cell spill into the intersti- tium and further increase the edema.15
Whitesides et al16 recom- mended that compartment pressures be compared with systemic diastolic pressures rather than absolute compart- ment pressures when deter- mining the need for fascioto- my. This may account for why hypotension has been reported as a risk factor for developing compartment syndrome and for why hypertension has a protective effect and elevated the threshold pressure for vi- ability of peripheral nerves.17 Conversely, in a study of tib- ial fractures and compartment syndrome by Park et al,18 no association was found be- tween diastolic pressure and acute compartment syndrome.
Increased understanding of the exact pathophysiology processes may guide the de- velopment of medical nonsur- gical interventions that could be applied in the early stages of acute compartment syn- drome development to stop its progression and eliminate the need for surgical intervention.
anatomy of ExtrEmity ComPartmEnts
Knowledge of the anatomy and contents of each compart- ment are of paramount im- portance during the physical examination for compartment syndrome (Table; Figure). In cases of compartment syn- drome of the leg, specifically in the context of a tibia frac- ture, the anterior compartment is almost always involved.19 Clinical judgement is an im-
portant tool for a surgeon to use to determine the need to release deep investing fascia or epimysium of a specific muscle compartment.10
EPidEmiology and Etiology
The mechanism of injury for acute compartment syn- drome ranges from high- and low-energy trauma to nontrau- matic causes.20,21 The reported incidence of high- and low- energy trauma leading to acute compartment syndrome is ap- proximately equal.4 McQueen et al6 reported that routine traffic accidents (involving both vehicle vs vehicle and vehicle vs pedestrian) were the most common causes of acute compartment syndrome, followed by sport-related in- juries. Tissue-crushing inju- ries, falls, direct blows, burns, and penetrating injuries were among other reported trau- matic mechanisms.6,22 Of note, traumatic injury leading to acute compartment syndrome was associated with frac- ture and nonfracture injuries. Circumferential wraps and casts also have the potential to restrict compartment expan- sion, decrease venous flow, and result in acute compart- ment syndrome.4,23
Age and sex distributions indicated that men in their thir- ties have the highest likelihood of developing acute compart- ment syndrome, which may be explained by the relatively larger muscle mass in men within a fixed compartment size after growth is complete. McQueen et al6 reported that the average annual incidence
of compartment syndrome for men was 7.3 per 100,000, with a mean age of 32 years, whereas the average annual incidence for women was 0.7 per 100,000, with a mean age of 44 years.
Fracture is the reason for initial presentation and a ma- jor contributing factor in ap- proximately 75% of cases of acute compartment syn- drome.4,6,13,24 Specifically, in a review of 164 patients with acute compartment syndrome, 113 (70%) patients had an associated fracture, with the most common fracture being tibial diaphyseal fractures in 59 (36%) patients.
Lower-leg acute compart- ment syndrome has been re- ported in 2% to 9% of tibial fractures.6,18,25 Park et al18 found that, depending on the location of tibial fractures, the incidence of acute compart- ment syndrome varied from 1.8% in proximal tibial frac- tures to 8.1% in diaphyseal fractures and 1.4% in distal fractures, with the predomi- nance at the diaphysis because the majority of muscle mass surrounds this area. McQueen et al6 reported 68 tibial frac- tures with acute compartment syndrome, of which 59 were diaphyseal fractures, 5 were tibial plateau fractures, and 4 were tibial pilon fractures.
Hope and McQueen26 re- ported the first series of pa- tients to develop acute com- partment syndrome in the ab- sence of a fracture and exclud- ed crush syndrome as a diag- nosis. They showed that these patients are typically older, have more comorbidities, and
AUGUST 2013 | Volume 36 • Number 8 621
n trauma update
have an increased chance of delay to fasciotomy, leading to increased muscle necrosis at the time of fasciotomy, cit- ing a low awareness for risk of acute compartment syndrome in an isolated soft tissue inju- ry. Posterior compartment in- volvement is more common in acute compartment syndrome without a fracture.26
CliniCal fEaturEs and diagnosis
The “6 Ps” (pain, pallor, paresthesia, paralysis, and pulselessness), which were initially developed to describe the findings seen in vascular injuries, have been used to de- scribe clinical signs associated with compartment syndrome. However, these clinical symp- toms are subject to large vari- ability and inconsistencies.27
Pulselessness and pallor are rarely associated with com- partment syndrome unless an associated vascular injury or systemic hypotension occurs. Practitioners who are unfamil- iar with the pathophysiology of compartment syndrome often place emphasis on the presence of pulses to incorrectly rule out compartment syndrome. The presence of paresthesia and pa- ralysis represent late findings after acute compartment syn- drome has likely been present for 4 hours or more.
Diagnosing compartment syndrome is difficult in clinical practice, even with the avail- ability of intracompartmental pressure measuring, and it has been argued that there is no way to determine the true rate of compartment syndrome.28 In addition, the gold standard for
diagnosis via measurement of compartment pressures has re- cently been questioned. Within a single Level I trauma institu- tion, a significant variation was found in different surgeons’ rates of compartment syndrome diagnosis. Interestingly, when looking at individual surgeons, the “more commonly a surgeon decided to check compartment pressures, the more likely the surgeon was to perform fasci- otomy,”28 which introduces the hypothesis that a high false-pos- itive rate may exist when using compartment checks. In addi- tion, Prayson et al29 prospective- ly looked at compartment pres- sures in lower-extremity frac- tures and showed that 84% of fractured extremities qualified for the diagnosis of compart- ment syndrome based on having a compartment pressure within 30 mm Hg of diastolic pressure. Prayson et al29 argued that “di- rect compartment measurement with existing thresholds and for- mulations to determine the diag-
nosis of compartment syndrome may not accurately reflect a true existence of the syndrome.”
Current methods for direct measuring and monitoring of the compartment pressures
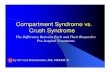
Figure: Axial section of the lower leg. Abbreviations: AIS, anterior intermuscu- lar septum; ATA, anterior tibial artery; ATV, anterior tibial vein; DPN, deep pero- neal nerve; F, fibula; GSaV, great saphenous vein; IM, interosseous membrane; LSuCN, lateral sural cutaneous nerve; MSuCN, medial sural cutaneous nerve; PA, peroneal artery; PIS, posterior intermuscular septum; PTA, posterior tibial artery; PTV, posterior tibial vein; PV, peroneal vein; SaN, saphenous nerve; SPN, superficial peroneal nerve; SSaV, small saphenous vein; T, tibia; TIS, transverse intermuscular septum; TN, tibial nerve.
Table
Anterior Extensor hallicus longus, extensor digitorum communis, tibialis anterior, peroneous tertius
Deep peroneal nerve Anterior tibial artery
Lateral Peroneous brevis and longus
Superficial peroneal nerve, proximal portion of deep peroneal nerve
Peroneal artery
Tibial nerve branches Posterior tibial artery, popliteal artery, peroneal artery, sural arteries
Posterior deep Popliteus; tibilis posterior, flexor hallicus longus, flexor digitorum longus, popliteus
Tibial nerve Posterior tibial artery, peroneal artery
622 ORTHOPEDICS | Healio.com/Orthopedics
n trauma update
include slit catheters, side- port needles, and ultrafiltra- tion catheters. Pressure mea- surement is done either by an arterial line set or another pressure-monitoring device.30 Contrary to previous studies questioning the usefulness of compartment pressure mea- surements, McQueen et al31
estimated the sensitivity and specificity to be high. In a large retrospective review of patients who sustained a tibial diaphyseal fracture and under- went documented continuous anterior compartment pressure monitoring, the sensitivity and specificity were estimated as 94% and 98%, respectively, and the positive and negative predictive values were 93% and 99%, respectively. The study diagnosed acute com- partment syndrome only after 2 hours of continuous anterior compartment measurement with the differential pressure (diastolic-intracompartmental pressure) remaining higher than 30 mm Hg, and the au- thors recommended continu- ous monitoring over 1 single measurement.31
Ulmer3 reviewed prospec- tive studies on compartment syndrome and, despite vari- ability in the clinical history and examination, was able to draw conclusions about the usefulness of the clinical find- ings. He looked specifically at pain, pain with passive stretch, paresthesias, and paresis in the literature and was unable to determine a consensus re- garding which sign was of the greatest value due to a paucity of data. However, regarding use of these clinical findings
in diagnosing compartment syndrome, the sensitivity was low (13% to 19%), the positive predictive value was low (11% to 19%), and both the speci- ficity and negative predictive values were high (both 97% to 98%, respectively).3
Pain out of proportion to the injury is often cited as an early sensitive sign,4 yet pain is often already present at varying levels in trauma pa- tients.13,19 Pain with a passive stretch of the muscle in the area of the injury has been re- ported to be of greatest clinical value but has also been stated to be too subjective.3 Swelling and palpable tenseness may be early signs of compartment syndrome, but at best they are crude indications of acute compartment syndrome.32 It is critical to maintain a high index of suspicion in at-risk patients, and repeated serial examinations are necessary.4,33
Magnetic resonance imag- ing (MRI) has been shown to identify chronic exertional compartment syndrome34; however, the use of MRI in trauma settings is limited due to the time commitment of MRI vs the emergent nature of acute compartment syndrome. Edematous changes on MRI are partially due to the initial injury and, although MRI can show changes in late compart- ment syndrome, it is not effec- tive in diagnosing early acute compartment syndrome.35 Ultrasonography techniques are still in the early stages of development for monitor- ing compartment and perfu- sion pressures. Noninvasive ultrasound devices and pulse
phase-locked loops detect slight movements in the fas- cia corresponding with arte- rial pulsation and distinguish between normal and abnormal intramuscular pressures.36,37 The benefit of this technology is that it is noninvasive and can be performed serially to produce a trend of intramuscu- lar pressures. This may allow clinicians to detect impending acute compartment syndrome in its early stages. Near- infrared spectroscopy technol- ogy is noninvasive, measures local soft tissue oxygenation approximately 2 to 3 cm below the skin, and could provide continuous monitoring for intracompartmental hypoxia. Near-infrared spectroscopy has shown promise to become a sensitive and specific moni- tor of oxygenation of individ- ual muscle compartments and is inversely correlated with increasing compartmental pressures. However, its limita- tions include use for patients with total body hypoperfusion and for obtaining measure- ments over a deoxygenated soft tissue hematoma.35,38,39 Interestingly, a lack of infor- mation exists in the literature on this subject, but measuring somatosensory-evoked poten- tials to detect nerve dysfunc- tion may play a role in future noninvasive monitoring for compartment syndrome.40,41
In a prospective study comparing different compart- mental measuring devices, Collinge and Kuper42 reported that no single measurement should be used for determina- tion for or against performing fasciotomy, recommending
the necessity of clinical corre- lation in the diagnosis of acute compartment syndrome.
trEatmEnt, fasCiotomy, and outComEs
Definitive treatment for acute compartment syndrome is emergent fasciotomy to de- compress the compartments involved and prevent critical ischemia. Soft tissue viability is of immediate concern and has a narrow treatment win- dow. As little as 8 hours of critical ischemia results in ir- reversible damage to compart- mental muscles and nerves.8 Both single- and double- incision fasciotomy tech- niques have been described for releasing the 4 compartments of the lower extremity. In the first analysis of single- vs double-incision fasciotomy techniques for tibial fractures in acute compartment syn- drome, Bible et al43 showed similar infection and nonunion rates between the techniques and left the choice to the sur- geon.
Surgical decompression is not always indicated if the compartment syndrome has been evident for more than 48 hours and no evidence ex- ists of retained function of the components within the compartment.30 Timing of prophylactic fasciotomy is controversial, and outcome data comparing prophylactic vs therapeutic fasciotomy are retrospective and of mediocre quality. In a study of 94 pa- tients (including trauma and vascular patients), Velmahos et al44 found higher complica- tion and nonclosure rates in
AUGUST 2013 | Volume 36 • Number 8 623
n trauma update
prophylactic fasciotomy cases. The authors make a valid point that prophylactic fasciotomy is not without major complica- tions, and the risk-benefit ratio should be weighed heavily.
ConClusion Acute compartment syn-
drome remains a true ortho- pedic emergency. Despite a large amount of research and many articles discussing novel diagnostic tools, clinical ex- amination is paramount, and the documentation of findings, discussion with patients and family, and treatment plan are essential. The authors believe that measurements of com- partment pressures or other nonclinical diagnostic means should have no bearing on the urgent “get out of bed and take the patient to the [operating room].”
Alternative methods for di- agnosing compartment syn- drome have been attempted, but none have replaced high clinical suspicion and clinical examination.34 Review of the literature demonstrates the need for prospective, random- ized trials comparing prophy- lactic and therapeutic fascioto- my, as well as additional in- vestigation into reliable meth- ods of diagnosing acute com- partment syndrome.
rEfErEnCEs 1. Matsen FA III, Krugmire RB
Jr. Compartmental syndromes. Surg Gynecol Obstet. 1978; 147:943-949.
2. Bhattacharyya T, Vrahas MS. The medical-legal aspects of compart- ment syndrome. J Bone Joint Surg Am. 2004; 86:864-868.
3. Ulmer T. The clinical diagno- sis of compartment syndrome
of the lower leg: are clinical findings predictive of the dis- order? J Orthop Trauma. 2002; 16:572-577.
4. Olson SA, Glasgow RR. Acute compartment syndrome in lower extremity musculoskel- etal trauma. J Am Acad Orthop Surg. 2005; 13:436-444.
5. Eaton RG, Green WT. Epimysiotomy and fasciotomy in the treatment of Volkmann’s ischemic contracture. Orthop Clin North Am. 1972; 3:175-186.
6. McQueen MM, Gaston P, Court-Brown CM. Acute com- partment syndrome. Who is at risk? J Bone Joint Surg Br. 2000; 82:200-203.
7. Holden CE. The pathology and prevention of Volkmann’s isch- aemic contracture. J Bone Joint Surg Br. 1979; 61:296-300.
8. Whitesides TE, Heckman MM. Acute compartment syndrome: update on diagnosis and treat- ment. J Am Acad Orthop Surg. 1996; 4:209-218.
9. Heppenstall RB, Sapega AA, Scott R, et al. The compartment syndrome. An experimental and clinical study of muscular ener- gy metabolism using phospho- rus nuclear magnetic resonance spectroscopy. Clin Orthop Relat Res. 1988; (226):138-155.
10. Leversedge FJ, Moore TJ, Peterson BC, Seiler JG III. Compartment syndrome of the upper extremity. J Hand Surg. 2011; 36:544-559.
11.…
n trauma update Section Editors: David J. Hak, MD, MBA & Philip F. Stahel, MD
Acute compartment syn- drome remains one of the
few true emergencies in ortho- pedic traumatology. It is a con- dition in which increased com- partment pressure within a con- fined space compromises the circulation and viability of the tissues within that space. In the orthopedic trauma setting, com- partment syndrome is observed in both acute open and closed
fracture settings, most often in the long bones of the forearm and leg.1 It can also be present in the absence of fracture follow- ing a severe soft tissue injury. Acute compartment syndrome is important for orthopedic sur- geons to recognize because its diagnosis is not always straight- forward, and it has a high risk of associated limb morbidity if left undiagnosed or untreated.
Early fasciotomy is of the utmost importance because definitive treatment through early and correct diagnosis is key in preventing morbid- ity.2 Classic cardinal signs for acute compartment syndrome have demonstrated less than optimal sensitivity but excel- lent specificity; as Ulmer3 stated: “these findings sug- gest that the clinical features of compartment syndrome of the lower leg are more useful by their absence in excluding the diagnosis than they are when present in confirming the diagnosis.”
Despite the ability to inva- sively measure compartment pressures, the diagnosis of acute compartment syndrome, which is an evolving patholog- ic process, is often based on the assessment of all related clinical factors. In this article, the authors review the patho- physiology, anatomy, diagno- sis, and treatment of this po- tentially devastating condition.
PathoPhysiology When inflammation devel-
ops following trauma, the lim-
iting envelope surrounding in- dividual muscle compartments leads to increased pressures that, if untreated, will eventu- ally produce a final common pathway of cellular anoxia and tissue damage.4 The limiting envelope is most often the fas- cia but can be the epimysium5 or skin.1 Fascial compartments are inelastic and do not change in size after development is complete, but the muscle within is not limited in growth. Patients with increased muscle mass have less space for swell- ing after muscle injury.6
The basic principle of isch- emia stems from inadequate perfusion relative to demand. The ischemia produced by compartment syndrome is a self-perpetuating cycle involv- ing increasing edema, pres- sure, and ischemia.7 Muscles and nerves tolerate ischemia for up to 4 hours with limited sequelae; however, 8 hours of ischemia results in irreversible damage.8 Fasciotomy allows for normalization of capillary blood flow and clears the lo- cal accumulation of anaerobic metabolite build-up via res-
Abstract: Acute compartment syndrome remains a challeng- ing problem for orthopedic surgeons because its diagnosis is not always straightforward and it has a high risk of associated limb morbidity if left undiagnosed or untreated. Failure to di- agnose and treat acute compartment syndrome is one of the most common causes of successful medical liability claims. The authors review the current literature concerning the diag- nosis of acute compartment syndrome and discuss new non- invasive technologies that may allow for earlier and more ac- curate diagnosis of impending acute compartment syndrome.
The authors are from the Department of Orthopaedics and Rehabilitation (NM), University of Vermont College of Medicine, Burlington, Vermont; and the Department of Orthopaedics (HG, CH, JH, DH, CM), Denver Health Medical Center, Denver, Colorado.
The authors have no relevant financial relationships to disclose. Correspondence should be addressed to: Cyril Mauffrey, MD, FRCS,
Department of Orthopaedics, Denver Health Medical Center, 777 Bannock St, Denver, CO 80204 ([email protected]).
doi: 10.3928/01477447-20130724-07
Acute Lower-leg Compartment Syndrome Nathan Mauser, MD; Hannah Gissel, BA; Corey Henderson, MS; Jiandong Hao, MD, PhD; David Hak, MD, MBA; Cyril Mauffrey, MD, FRCS
620 ORTHOPEDICS | Healio.com/Orthopedics
n trauma update
toration of physiologic pres- sures within the compartment. Following decompression, if early enough in the cycle, cells may become edematous and histologically will appear to exhibit injury. However, nor- mal morphology is returned after 1 week.9,10
Several hypotheses exist regarding the pathophysiology of compartment syndrome, and it is likely that this syndrome is more complex than the cur- rent state of knowledge. The most widely accepted hypoth- esis is the arteriovenous pres- sure gradient theory, in which reduction of this gradient and decreased microvascular flow through the capillaries perpetu- ates edema and pressure, lead- ing to increased ischemia.1,7 Initially, and most often in the acute setting, an increase in lo- cal pressure and edema stem from the insult. Subsequently, an increase in local intravenous pressure occurs, as well as a reduction in arteriovenous gra- dient, and leads to a local de- crease in perfusion.
Endothelial cells sustain damage via anoxia and in- creased vessel wall permeabil- ity.11 In addition to the decrease in perfusion, the decreased venous return increases tis- sue edema. Lymphatic drain- age can only compensate to a point and will fail under high pressure.12 It is the venous flow and this local stasis that perpetuate the edema and el- evate compartment pressures. The pressures then increase to equal the diastolic blood pres- sure, and local tissue perfusion ceases.13,14 Once muscle necro- sis begins and cytolysis occurs,
the osmotically active contents of the cell spill into the intersti- tium and further increase the edema.15
Whitesides et al16 recom- mended that compartment pressures be compared with systemic diastolic pressures rather than absolute compart- ment pressures when deter- mining the need for fascioto- my. This may account for why hypotension has been reported as a risk factor for developing compartment syndrome and for why hypertension has a protective effect and elevated the threshold pressure for vi- ability of peripheral nerves.17 Conversely, in a study of tib- ial fractures and compartment syndrome by Park et al,18 no association was found be- tween diastolic pressure and acute compartment syndrome.
Increased understanding of the exact pathophysiology processes may guide the de- velopment of medical nonsur- gical interventions that could be applied in the early stages of acute compartment syn- drome development to stop its progression and eliminate the need for surgical intervention.
anatomy of ExtrEmity ComPartmEnts
Knowledge of the anatomy and contents of each compart- ment are of paramount im- portance during the physical examination for compartment syndrome (Table; Figure). In cases of compartment syn- drome of the leg, specifically in the context of a tibia frac- ture, the anterior compartment is almost always involved.19 Clinical judgement is an im-
portant tool for a surgeon to use to determine the need to release deep investing fascia or epimysium of a specific muscle compartment.10
EPidEmiology and Etiology
The mechanism of injury for acute compartment syn- drome ranges from high- and low-energy trauma to nontrau- matic causes.20,21 The reported incidence of high- and low- energy trauma leading to acute compartment syndrome is ap- proximately equal.4 McQueen et al6 reported that routine traffic accidents (involving both vehicle vs vehicle and vehicle vs pedestrian) were the most common causes of acute compartment syndrome, followed by sport-related in- juries. Tissue-crushing inju- ries, falls, direct blows, burns, and penetrating injuries were among other reported trau- matic mechanisms.6,22 Of note, traumatic injury leading to acute compartment syndrome was associated with frac- ture and nonfracture injuries. Circumferential wraps and casts also have the potential to restrict compartment expan- sion, decrease venous flow, and result in acute compart- ment syndrome.4,23
Age and sex distributions indicated that men in their thir- ties have the highest likelihood of developing acute compart- ment syndrome, which may be explained by the relatively larger muscle mass in men within a fixed compartment size after growth is complete. McQueen et al6 reported that the average annual incidence
of compartment syndrome for men was 7.3 per 100,000, with a mean age of 32 years, whereas the average annual incidence for women was 0.7 per 100,000, with a mean age of 44 years.
Fracture is the reason for initial presentation and a ma- jor contributing factor in ap- proximately 75% of cases of acute compartment syn- drome.4,6,13,24 Specifically, in a review of 164 patients with acute compartment syndrome, 113 (70%) patients had an associated fracture, with the most common fracture being tibial diaphyseal fractures in 59 (36%) patients.
Lower-leg acute compart- ment syndrome has been re- ported in 2% to 9% of tibial fractures.6,18,25 Park et al18 found that, depending on the location of tibial fractures, the incidence of acute compart- ment syndrome varied from 1.8% in proximal tibial frac- tures to 8.1% in diaphyseal fractures and 1.4% in distal fractures, with the predomi- nance at the diaphysis because the majority of muscle mass surrounds this area. McQueen et al6 reported 68 tibial frac- tures with acute compartment syndrome, of which 59 were diaphyseal fractures, 5 were tibial plateau fractures, and 4 were tibial pilon fractures.
Hope and McQueen26 re- ported the first series of pa- tients to develop acute com- partment syndrome in the ab- sence of a fracture and exclud- ed crush syndrome as a diag- nosis. They showed that these patients are typically older, have more comorbidities, and
AUGUST 2013 | Volume 36 • Number 8 621
n trauma update
have an increased chance of delay to fasciotomy, leading to increased muscle necrosis at the time of fasciotomy, cit- ing a low awareness for risk of acute compartment syndrome in an isolated soft tissue inju- ry. Posterior compartment in- volvement is more common in acute compartment syndrome without a fracture.26
CliniCal fEaturEs and diagnosis
The “6 Ps” (pain, pallor, paresthesia, paralysis, and pulselessness), which were initially developed to describe the findings seen in vascular injuries, have been used to de- scribe clinical signs associated with compartment syndrome. However, these clinical symp- toms are subject to large vari- ability and inconsistencies.27
Pulselessness and pallor are rarely associated with com- partment syndrome unless an associated vascular injury or systemic hypotension occurs. Practitioners who are unfamil- iar with the pathophysiology of compartment syndrome often place emphasis on the presence of pulses to incorrectly rule out compartment syndrome. The presence of paresthesia and pa- ralysis represent late findings after acute compartment syn- drome has likely been present for 4 hours or more.
Diagnosing compartment syndrome is difficult in clinical practice, even with the avail- ability of intracompartmental pressure measuring, and it has been argued that there is no way to determine the true rate of compartment syndrome.28 In addition, the gold standard for
diagnosis via measurement of compartment pressures has re- cently been questioned. Within a single Level I trauma institu- tion, a significant variation was found in different surgeons’ rates of compartment syndrome diagnosis. Interestingly, when looking at individual surgeons, the “more commonly a surgeon decided to check compartment pressures, the more likely the surgeon was to perform fasci- otomy,”28 which introduces the hypothesis that a high false-pos- itive rate may exist when using compartment checks. In addi- tion, Prayson et al29 prospective- ly looked at compartment pres- sures in lower-extremity frac- tures and showed that 84% of fractured extremities qualified for the diagnosis of compart- ment syndrome based on having a compartment pressure within 30 mm Hg of diastolic pressure. Prayson et al29 argued that “di- rect compartment measurement with existing thresholds and for- mulations to determine the diag-
nosis of compartment syndrome may not accurately reflect a true existence of the syndrome.”
Current methods for direct measuring and monitoring of the compartment pressures
Figure: Axial section of the lower leg. Abbreviations: AIS, anterior intermuscu- lar septum; ATA, anterior tibial artery; ATV, anterior tibial vein; DPN, deep pero- neal nerve; F, fibula; GSaV, great saphenous vein; IM, interosseous membrane; LSuCN, lateral sural cutaneous nerve; MSuCN, medial sural cutaneous nerve; PA, peroneal artery; PIS, posterior intermuscular septum; PTA, posterior tibial artery; PTV, posterior tibial vein; PV, peroneal vein; SaN, saphenous nerve; SPN, superficial peroneal nerve; SSaV, small saphenous vein; T, tibia; TIS, transverse intermuscular septum; TN, tibial nerve.
Table
Anterior Extensor hallicus longus, extensor digitorum communis, tibialis anterior, peroneous tertius
Deep peroneal nerve Anterior tibial artery
Lateral Peroneous brevis and longus
Superficial peroneal nerve, proximal portion of deep peroneal nerve
Peroneal artery
Tibial nerve branches Posterior tibial artery, popliteal artery, peroneal artery, sural arteries
Posterior deep Popliteus; tibilis posterior, flexor hallicus longus, flexor digitorum longus, popliteus
Tibial nerve Posterior tibial artery, peroneal artery
622 ORTHOPEDICS | Healio.com/Orthopedics
n trauma update
include slit catheters, side- port needles, and ultrafiltra- tion catheters. Pressure mea- surement is done either by an arterial line set or another pressure-monitoring device.30 Contrary to previous studies questioning the usefulness of compartment pressure mea- surements, McQueen et al31
estimated the sensitivity and specificity to be high. In a large retrospective review of patients who sustained a tibial diaphyseal fracture and under- went documented continuous anterior compartment pressure monitoring, the sensitivity and specificity were estimated as 94% and 98%, respectively, and the positive and negative predictive values were 93% and 99%, respectively. The study diagnosed acute com- partment syndrome only after 2 hours of continuous anterior compartment measurement with the differential pressure (diastolic-intracompartmental pressure) remaining higher than 30 mm Hg, and the au- thors recommended continu- ous monitoring over 1 single measurement.31
Ulmer3 reviewed prospec- tive studies on compartment syndrome and, despite vari- ability in the clinical history and examination, was able to draw conclusions about the usefulness of the clinical find- ings. He looked specifically at pain, pain with passive stretch, paresthesias, and paresis in the literature and was unable to determine a consensus re- garding which sign was of the greatest value due to a paucity of data. However, regarding use of these clinical findings
in diagnosing compartment syndrome, the sensitivity was low (13% to 19%), the positive predictive value was low (11% to 19%), and both the speci- ficity and negative predictive values were high (both 97% to 98%, respectively).3
Pain out of proportion to the injury is often cited as an early sensitive sign,4 yet pain is often already present at varying levels in trauma pa- tients.13,19 Pain with a passive stretch of the muscle in the area of the injury has been re- ported to be of greatest clinical value but has also been stated to be too subjective.3 Swelling and palpable tenseness may be early signs of compartment syndrome, but at best they are crude indications of acute compartment syndrome.32 It is critical to maintain a high index of suspicion in at-risk patients, and repeated serial examinations are necessary.4,33
Magnetic resonance imag- ing (MRI) has been shown to identify chronic exertional compartment syndrome34; however, the use of MRI in trauma settings is limited due to the time commitment of MRI vs the emergent nature of acute compartment syndrome. Edematous changes on MRI are partially due to the initial injury and, although MRI can show changes in late compart- ment syndrome, it is not effec- tive in diagnosing early acute compartment syndrome.35 Ultrasonography techniques are still in the early stages of development for monitor- ing compartment and perfu- sion pressures. Noninvasive ultrasound devices and pulse
phase-locked loops detect slight movements in the fas- cia corresponding with arte- rial pulsation and distinguish between normal and abnormal intramuscular pressures.36,37 The benefit of this technology is that it is noninvasive and can be performed serially to produce a trend of intramuscu- lar pressures. This may allow clinicians to detect impending acute compartment syndrome in its early stages. Near- infrared spectroscopy technol- ogy is noninvasive, measures local soft tissue oxygenation approximately 2 to 3 cm below the skin, and could provide continuous monitoring for intracompartmental hypoxia. Near-infrared spectroscopy has shown promise to become a sensitive and specific moni- tor of oxygenation of individ- ual muscle compartments and is inversely correlated with increasing compartmental pressures. However, its limita- tions include use for patients with total body hypoperfusion and for obtaining measure- ments over a deoxygenated soft tissue hematoma.35,38,39 Interestingly, a lack of infor- mation exists in the literature on this subject, but measuring somatosensory-evoked poten- tials to detect nerve dysfunc- tion may play a role in future noninvasive monitoring for compartment syndrome.40,41
In a prospective study comparing different compart- mental measuring devices, Collinge and Kuper42 reported that no single measurement should be used for determina- tion for or against performing fasciotomy, recommending
the necessity of clinical corre- lation in the diagnosis of acute compartment syndrome.
trEatmEnt, fasCiotomy, and outComEs
Definitive treatment for acute compartment syndrome is emergent fasciotomy to de- compress the compartments involved and prevent critical ischemia. Soft tissue viability is of immediate concern and has a narrow treatment win- dow. As little as 8 hours of critical ischemia results in ir- reversible damage to compart- mental muscles and nerves.8 Both single- and double- incision fasciotomy tech- niques have been described for releasing the 4 compartments of the lower extremity. In the first analysis of single- vs double-incision fasciotomy techniques for tibial fractures in acute compartment syn- drome, Bible et al43 showed similar infection and nonunion rates between the techniques and left the choice to the sur- geon.
Surgical decompression is not always indicated if the compartment syndrome has been evident for more than 48 hours and no evidence ex- ists of retained function of the components within the compartment.30 Timing of prophylactic fasciotomy is controversial, and outcome data comparing prophylactic vs therapeutic fasciotomy are retrospective and of mediocre quality. In a study of 94 pa- tients (including trauma and vascular patients), Velmahos et al44 found higher complica- tion and nonclosure rates in
AUGUST 2013 | Volume 36 • Number 8 623
n trauma update
prophylactic fasciotomy cases. The authors make a valid point that prophylactic fasciotomy is not without major complica- tions, and the risk-benefit ratio should be weighed heavily.
ConClusion Acute compartment syn-
drome remains a true ortho- pedic emergency. Despite a large amount of research and many articles discussing novel diagnostic tools, clinical ex- amination is paramount, and the documentation of findings, discussion with patients and family, and treatment plan are essential. The authors believe that measurements of com- partment pressures or other nonclinical diagnostic means should have no bearing on the urgent “get out of bed and take the patient to the [operating room].”
Alternative methods for di- agnosing compartment syn- drome have been attempted, but none have replaced high clinical suspicion and clinical examination.34 Review of the literature demonstrates the need for prospective, random- ized trials comparing prophy- lactic and therapeutic fascioto- my, as well as additional in- vestigation into reliable meth- ods of diagnosing acute com- partment syndrome.
rEfErEnCEs 1. Matsen FA III, Krugmire RB
Jr. Compartmental syndromes. Surg Gynecol Obstet. 1978; 147:943-949.
2. Bhattacharyya T, Vrahas MS. The medical-legal aspects of compart- ment syndrome. J Bone Joint Surg Am. 2004; 86:864-868.
3. Ulmer T. The clinical diagno- sis of compartment syndrome
of the lower leg: are clinical findings predictive of the dis- order? J Orthop Trauma. 2002; 16:572-577.
4. Olson SA, Glasgow RR. Acute compartment syndrome in lower extremity musculoskel- etal trauma. J Am Acad Orthop Surg. 2005; 13:436-444.
5. Eaton RG, Green WT. Epimysiotomy and fasciotomy in the treatment of Volkmann’s ischemic contracture. Orthop Clin North Am. 1972; 3:175-186.
6. McQueen MM, Gaston P, Court-Brown CM. Acute com- partment syndrome. Who is at risk? J Bone Joint Surg Br. 2000; 82:200-203.
7. Holden CE. The pathology and prevention of Volkmann’s isch- aemic contracture. J Bone Joint Surg Br. 1979; 61:296-300.
8. Whitesides TE, Heckman MM. Acute compartment syndrome: update on diagnosis and treat- ment. J Am Acad Orthop Surg. 1996; 4:209-218.
9. Heppenstall RB, Sapega AA, Scott R, et al. The compartment syndrome. An experimental and clinical study of muscular ener- gy metabolism using phospho- rus nuclear magnetic resonance spectroscopy. Clin Orthop Relat Res. 1988; (226):138-155.
10. Leversedge FJ, Moore TJ, Peterson BC, Seiler JG III. Compartment syndrome of the upper extremity. J Hand Surg. 2011; 36:544-559.
11.…
Related Documents