Clinical and Experimental Optometry 90.1 January 2007 © 2007 The Authors Journal compilation © 2007 Optometrists Association Australia 5 CLINICAL AND EXPERIMENTAL OPTOMETRY Clin Exp Optom 2007; 90: 1: 5–19 DOI:10.1111/j.1444-0938.2007.00112.x Key words: aberrations, astigmatism, cornea, corneal topography, refractive error Astigmatism is a commonly encountered refractive error, accounting for about 13 per cent of the refractive errors of the human eye. 1 Our knowledge of astigma- tism appears to have begun in the early 1800s when Thomas Young reported on his own astigmatism but it was not until 1825 that the first cylindrical lens was used by George Airy for the purpose of correct- ing his own astigmatic refractive error. 2 Since these early explorations, there has been a great deal of research carried out into various aspects of astigmatism. One reason for this research interest is the fact that the presence of astigmatism appears to have the potential to influence normal visual development. The presence of high degrees of astigmatism is associated with the development of amblyopia 3–5 and some associations have also been noted between astigmatism and the develop- ment of myopia. 6–10 Advances in technol- ogy and instrumentation mean that our ability to measure, define and analyse the eye’s optical and shape properties (includ- ing astigmatism) have improved markedly in recent years. Despite extensive research, the exact cause of astigmatism is still not known. One possible reason for astigmatic devel- opment would be a genetic aetiology. Other possible causes include mechanical interactions between the cornea and the eyelids and/or the extraocular muscles or a visual feedback model in which astigma- tism develops in response to visual cues. In this review we will consider the various hypotheses regarding the aetiology of astigmatism and examine the evidence in the literature for these theories. We will also present some new evidence from recent research in our laboratory that has investigated the role of near work and eye- lid forces on corneal shape and refractive error development. COMPONENTS OF ASTIGMATISM Ocular astigmatism can occur as a result of unequal curvature along the two prin- cipal meridia of the anterior cornea Scott A Read PhD Michael J Collins PhD Leo G Carney DSc Contact Lens and Visual Optics Laboratory, School of Optometry, Queensland University of Technology, Brisbane, Queensland, Australia E-mail: [email protected] Astigmatism is a refractive condition encountered commonly in clinical practice. This review presents an overview of research that has been carried out examining various aspects of this refractive error. We examine the components of astigmatism and the research into the prevalence and natural course of astigmatic refractive errors through- out life. The prevalence of astigmatism in various ethnic groups and diseases and syn- dromes is also discussed. We highlight the extensive investigations that have been conducted into the possible aetiology of astigmatism, however, no single model or theory of the development of astigmatism has been proven conclusively. Theories of the devel- opment of astigmatism based on genetics, extraocular muscle tension, visual feedback and eyelid pressure are considered. Observations and evidence from the literature supporting and contradicting these hypotheses are presented. Recent advances in tech- nology such as wavefront sensors and videokeratoscopes have led to an increased under- standing of ocular astigmatism and with continued improvements in technology, our knowledge of astigmatism and its genesis should continue to grow. A review of astigmatism and its possible genesis Submitted: 7 September 2006 Revised: 3 October 2006 Accepted for publication: 10 October 2006 INVITED REVIEW 14440938, 2007, 1, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/j.1444-0938.2007.00112.x by Readcube (Labtiva Inc.), Wiley Online Library on [11/03/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
A review of astigmatism and its possible genesisClinical and Experimental Optometry 90.1 January 2007© 2007 The Authors
Journal compilation © 2007 Optometrists Association Australia 5
C L I N I C A L A N D E X P E R I M E N T A L
OPTOMETRY
Key words: aberrations, astigmatism, cornea, corneal topography, refractive error
Astigmatism is a commonly encountered refractive error, accounting for about 13 per cent of the refractive errors of the human eye.1 Our knowledge of astigma- tism appears to have begun in the early 1800s when Thomas Young reported on his own astigmatism but it was not until 1825 that the first cylindrical lens was used by George Airy for the purpose of correct- ing his own astigmatic refractive error.2
Since these early explorations, there has been a great deal of research carried out into various aspects of astigmatism. One reason for this research interest is the fact that the presence of astigmatism appears to have the potential to influence normal visual development. The presence of high
degrees of astigmatism is associated with the development of amblyopia3–5 and some associations have also been noted between astigmatism and the develop- ment of myopia.6–10 Advances in technol- ogy and instrumentation mean that our ability to measure, define and analyse the eye’s optical and shape properties (includ- ing astigmatism) have improved markedly in recent years.
Despite extensive research, the exact cause of astigmatism is still not known. One possible reason for astigmatic devel- opment would be a genetic aetiology. Other possible causes include mechanical interactions between the cornea and the eyelids and/or the extraocular muscles or
a visual feedback model in which astigma- tism develops in response to visual cues. In this review we will consider the various hypotheses regarding the aetiology of astigmatism and examine the evidence in the literature for these theories. We will also present some new evidence from recent research in our laboratory that has investigated the role of near work and eye- lid forces on corneal shape and refractive error development.
COMPONENTS OF ASTIGMATISM
Ocular astigmatism can occur as a result of unequal curvature along the two prin- cipal meridia of the anterior cornea
Scott A Read PhD Michael J Collins PhD Leo G Carney DSc Contact Lens and Visual Optics Laboratory, School of Optometry, Queensland University of Technology, Brisbane, Queensland, Australia E-mail: [email protected]
Astigmatism is a refractive condition encountered commonly in clinical practice. This review presents an overview of research that has been carried out examining various aspects of this refractive error. We examine the components of astigmatism and the research into the prevalence and natural course of astigmatic refractive errors through- out life. The prevalence of astigmatism in various ethnic groups and diseases and syn- dromes is also discussed. We highlight the extensive investigations that have been conducted into the possible aetiology of astigmatism, however, no single model or theory of the development of astigmatism has been proven conclusively. Theories of the devel- opment of astigmatism based on genetics, extraocular muscle tension, visual feedback and eyelid pressure are considered. Observations and evidence from the literature supporting and contradicting these hypotheses are presented. Recent advances in tech- nology such as wavefront sensors and videokeratoscopes have led to an increased under- standing of ocular astigmatism and with continued improvements in technology, our knowledge of astigmatism and its genesis should continue to grow.
A review of astigmatism and its possible genesis
Submitted: 7 September 2006 Revised: 3 October 2006 Accepted for publication: 10 October 2006
INVITED REVIEW
nloaded from https://onlinelibrary.w
iley O nline L
s and C onditions (https://onlinelibrary.w
iley.com /term
nline L ibrary for rules of use; O
A articles are governed by the applicable C
reative C om
m ons L
Clinical and Experimental Optometry 90.1 January 2007
6
Journal compilation © 2007 Optometrists Association Australia
(known as corneal astigmatism) and/or it may be due to the posterior cornea, unequal curvatures of the front and back surfaces of the crystalline lens, decentra- tion or tilting of the lens or unequal refrac- tive indices across the crystalline lens (known as internal or residual astigma- tism). The combination of the corneal and the internal astigmatism gives the eye’s total astigmatism (that is, total astigmatism equals corneal astigmatism plus internal astigmatism). Corneal astigmatism is often classified according to the axis of asti- gmatism as being either with-the rule (WTR), oblique or against-the-rule (ATR) (Figure 1). In the past, astigmatism has been defined as ‘regular’ or ‘irregular’. Typically, irregular astigmatism is used to describe a variety of asymmetric aberra- tions such as coma, trefoil and quadrafoil. The widely adopted use of Zernike poly- nomials to describe the detailed compo- nents of the eye’s optics has made the use of the term ‘irregular’ astigmatism largely redundant.
A recent study investigating corneal topography has classified astigmatism according to the changes occurring in the astigmatism of the peripheral cornea.11
Corneal astigmatism was classified as being stable, reducing or increasing in the peripheral cornea. Of the subjects with significant corneal astigmatism tested in this study, astigmatism was found most commonly to be reducing (47 per cent of astigmatic subjects) or stable (44 per cent) in the peripheral cornea. Figure 2 illustrates these forms of corneal astigmatism.
CORNEAL AND INTERNAL ASTIGMATISM
It is well accepted that there is some rela- tionship between the eye’s corneal and internal astigmatism. In 1890, Javal pro- posed a rule that predicted the total astig- matism of the eye based on the corneal astigmatism.12 Javal’s rule states:
where At is the total astigmatism and Ac is the corneal astigmatism. The terms k and
A k p At c= + ( )
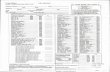
Figure 1. Example of the classification of corneal astigmatism according to the axis. Astigmatism can be classified as either with-the-rule (WTR) (where the steepest corneal meridian is oriented approximately vertically) (left), against-the-rule (ATR) (where the steepest corneal meridian is oriented close to horizontal) (right) or as oblique (where the steepest corneal meridian is oriented at an oblique angle) (centre). Axial curvature corneal topography maps are shown here for three different subjects.
Figure 2. Examples of two forms of corneal astigmatism. The maps on the left illus- trate corneal astigmatism that is stable in the peripheral cornea (or astigmatism that extends out into the peripheral cornea). The maps on the right illustrate corneal astigmatism that reduces in the peripheral cornea (or astigmatism that is primarily confined to the central cornea). Axial power maps are displayed at the top and only the cylinder power is plotted in the lower maps (for both the central and peripheral cornea).
14440938, 2007, 1, D ow
nloaded from https://onlinelibrary.w
iley O nline L
s and C onditions (https://onlinelibrary.w
iley.com /term
nline L ibrary for rules of use; O
A articles are governed by the applicable C
reative C om
m ons L
Clinical and Experimental Optometry 90.1 January 2007
7
Journal compilation © 2007 Optometrists Association Australia
p are constants approximated by 0.5 and 1.25, respectively. This rule relies on the fact that residual astigmatism is thought to be constant and ATR in most people (that is, -0.50 D ATR).
Grosvenor, Quintero and Perrigin13 sug- gested a simplification of Javal’s rule. Regression analysis was carried out to investigate the relationship between cor- neal and total astigmatism. The slope of this regression line is equivalent to the constant ‘p’ (from Javal’s rule), and the y intercept is equivalent to constant ‘k’. The slope of the regression line was found to be slightly less than one, and the y inter- cept close to 0.5. Based on these results, the authors proposed a simplified Javal’s rule of At = Ac - 0.5. This simplified rule was found to fit their data more closely than the original Javal’s rule, which sug- gests that an internal astigmatism of mag- nitude 0.5 D is relatively constant across subjects with different amounts of corneal astigmatism.
Keller and colleagues14 investigated the relationship between corneal and total astigmatism by measuring corneal astig- matism with a computer-assisted videok- eratoscope. The corneal topographical data were converted into a best fit sphero- cylinder for a number of different pupil sizes and subjective refraction was mea- sured using the same pupil sizes. Corneal astigmatism was plotted against total astig- matism for the different pupil sizes and the relationship between corneal and total astigmatism was found to be inde- pendent of pupil size. The results from this study supported Javal’s rule as simpli-
fied by Grosvenor, Quintero and Perrigin (1988).
Kelly, Mihashi and Howland15 used an instrument that allowed simultaneous cap- ture of corneal and total eye aberrations on a population of young subjects. They found that some corneal aberrations are compensated by the internal optics of the eye, including horizontal/vertical astigma- tism, lateral coma and spherical aberra- tion. They suggested that the horizontal/ vertical astigmatism compensation is an active process determined through a fine-tuning, emmetropisation process. No significant compensation was found for oblique astigmatism in this population.
Dunne, Elawad and Barnes16 investi- gated residual astigmatism, by measuring the difference between ocular and total astigmatism (by cylindrical decomposi- tion). The average residual astigmatism was found to be -0.46 × 98.2° for right eyes and -0.50 × 99.4° for left eyes. In ap- proximately two-thirds of eyes, the axis of the residual astigmatism was found to be perpendicular to the axis of corneal astigmatism.
Several studies have investigated the astigmatism contributed by the posterior corneal surface.17–20 These studies have found levels of astigmatism for the poste- rior cornea ranging from 0.18–0.31 D. The curvature of the posterior cornea combined with the refractive index differ- ence between the cornea and the aqueous means that the posterior corneal astigma- tism is of opposite sign to that of the ante- rior cornea. Therefore, the compensation of corneal astigmatism by the eye’s inter-
nal optics can be attributed, in part, to the astigmatism of the posterior cornea.
The compensation of corneal astigma- tism by the internal optics of the eye has been known for many years.12,15,16 The numerous studies into Javal’s rule tend to indicate that this compensation is a pas- sive process (that is, the majority of the population has approximately 0.5 D of internal astigmatism, opposite in sign to the corneal astigmatism). Some authors15
have suggested the possibility of an active ‘feedback driven’ process operat- ing to reduce the total astigmatism of the eye (particularly horizontal/vertical astigmatism).
PREVALENCE OF ASTIGMATISM AND CHANGES WITH AGE
There have been many studies that have attempted to define the prevalence of astigmatism in the population and to illus- trate the typical changes that occur in astigmatism throughout life. These inves- tigations provide some clues to the pos- sible causes of astigmatism. Figure 3 illustrates the typical changes that occur in astigmatism throughout life.
Astigmatism in early life (infancy and early childhood) Generally, studies have shown that in the first months of life, infants exhibit a high prevalence of significant degrees of astig- matism,21–30 which appears to be corneal in origin.24,27,29 The cornea of newborns is steep and exhibits large degrees of astig- matism.27,29,31 Isenberg and co-workers29
Figure 3. The typical changes that occur in astigmatism throughout life
Early childhood
· Most common axis ATR?
Adulthood
Older adulthood
40+ years
· Shift in corneal astigmatism axis towards ATR being most common
14440938, 2007, 1, D ow
nloaded from https://onlinelibrary.w
iley O nline L
s and C onditions (https://onlinelibrary.w
iley.com /term
nline L ibrary for rules of use; O
A articles are governed by the applicable C
reative C om
m ons L
Clinical and Experimental Optometry 90.1 January 2007
8
Journal compilation © 2007 Optometrists Association Australia
used videokeratoscopy to measure the cor- neal curvature of newborns (up to eight days after birth) and found an average of six dioptres of corneal astigmatism. Stud- ies have also shown that the steepest, most astigmatic corneas occur in the newborns with the lowest birth weight and lowest post-conceptional age.27 While studies have consistently found high degrees of corneal astigmatism to be present in infancy, there is some conflicting evidence of the most common axis of astigmatism. Perhaps indicating the difficulties of obtaining accurate measurements on new- born infants or suggesting a large amount of variability in the corneal shape of infants, some studies have found a pre- dominance of WTR corneal astigma- tism,26,29,30 while others have shown a predominance of ATR corneal astigma- tism in infants.22–25,27
As infants grow older, the prevalence of high degrees of astigmatism typically reduces or, in other words, an emmetropi- sation of the astigmatic refractive error occurs.21–29 Dobson, Fulton and Sebris22
and Gwiazda and colleagues23 found a shift in astigmatism from a predominance of higher degrees of ATR astigmatism in children younger than four years, to a pre- dominance of low levels of WTR astigma- tism in children older than four years. Gwiazda and colleagues23 postulated that pressure from the eyelids on the cornea over time may be causing the shift in astig- matic axis from ATR to WTR in children.
Studies of preschool-age children gen- erally show a relatively low prevalence of high degrees of astigmatism (that is, greater than one dioptre) that is predom- inantly WTR in nature.32–34 Huynh and associates34 investigated a large population of six-year-old children and found that only 4.8 per cent of children exhibited greater than one dioptre of ocular astig- matism and 75 per cent of subjects exhib- ited WTR corneal astigmatism.
In summary, at birth children exhibit a high incidence of astigmatism that is cor- neal in origin. As children grow older, the cornea flattens with significantly reduced astigmatism. Over the age of four years, the prevalence of large amounts of astigmatism is low, with small
amounts of WTR astigmatism being found most commonly.
Astigmatism in adults Astigmatism in young adults (younger than 40 years) occurs commonly but in relatively low amounts.35,36 In an investiga- tion of young adults aged 20 to 30 years, Satterfield36 found that 63 per cent of sub- jects exhibited 0.25 D or more of ocular astigmatism, however, the majority of sub- jects with measurable astigmatism exhib- ited less than one dioptre. In a cross- sectional study, Fledelius and Stubgaard37
found that 46 per cent of the total popu- lation had corneal astigmatism of greater than 0.5 D but only 4.7 per cent of the population exhibited greater than 1.5 D of corneal astigmatism. Generally, studies have shown that in young adults, WTR astigmatism occurs most commonly.35,37–42
With increasing age, a general shift in the axis of astigmatism is found from a predominance of WTR astigmatism (in adults younger than 40 years) to a pre- dominance of ATR astigmatism (in adults older than 40 years).35,38–40,42,43 This shift in astigmatic axis in older age appears to be due to changes in corneal curvature.38–40,42
In a cross-sectional study of corneal and total astigmatism, Anstice38 found that internal astigmatism remained relatively stable over time and that changes in astig- matism throughout life were due prima- rily to changes in corneal curvature. Baldwin and Mills39 investigated longitudi- nal changes in corneal and total astigma- tism in patients over a 40-year period and found a steepening of the cornea and an increase in ATR astigmatism with aging. The majority of this change in astigmatism was due to corneal change, that is, a steep- ening of the horizontal meridian of the cornea. As will be discussed later, this change in corneal curvature may be related to the reduction in tension of the eyelids that typically occurs with age.
In summary, young adult subjects typi- cally display small degrees of WTR astig- matism and in older adult years a shift in astigmatism occurs where ATR astigma- tism becomes more prevalent. Astigma- tism most commonly occurs due to the curvature of the cornea and the changes
in astigmatism that occur throughout life also appear to be due primarily to corneal change.
ASTIGMATISM IN RIGHT AND LEFT EYES
There is widespread agreement that some degree of symmetry exists between the refractive errors of right and left eyes. Sev- eral studies have noted mirror symmetry to occur between the axes of astigmatism of right and left eyes.16,44,45 McKendrick and Brennan41 measured corneal and ocular refraction (with autorefraction and autokeratometry) for both eyes in a group of subjects. The mean and spread of astig- matic errors was similar for right and left eyes. The axes of corneal and total astig- matism were found to be similar between the two eyes.46 Most subjects were found to display either mirror (for example, right eye axis 10°, left eye axis 170°) or direct (for example, right eye axis 10°, left eye axis 10°) symmetry of their astigmatic axes. There was no predominance of either mirror or direct symmetry of astig- matic axes when analysis was carried out for the population. Figure 4 illustrates the corneal topography from a normal subject who shows mirror symmetry between the corneal astigmatism of the right and left eyes.
ASTIGMATISM AND OTHER REFRACTIVE ERRORS
There is some evidence to suggest that the presence of astigmatism may be associated with the presence of spherical refractive errors. The presence of astigmatism has been found to be associated with myopic refractive errors, that is, astigmatism was associated with higher degrees of myo- pia.6–10,47,48 Fulton, Hansen and Petersen6
suggested that uncorrected astigmatic errors influenced the development of myopia and that the optical blur from uncorrected astigmatism may be a trigger for myopic development. The presence and changes in astigmatism have been found by some investigators to be associ- ated with an increased progression of myopia.6,10,49 In a longitudinal study of
14440938, 2007, 1, D ow
nloaded from https://onlinelibrary.w
iley O nline L
s and C onditions (https://onlinelibrary.w
iley.com /term
nline L ibrary for rules of use; O
A articles are governed by the applicable C
reative C om
m ons L
Clinical and Experimental Optometry 90.1 January 2007
9
refractive error, Gwiazda and colleagues7
found that their subjects exhibiting signif- icant ATR astigmatism and myopia in infancy were more likely to develop myo- pia at school age. In contrast with these studies, other investigators50,51 have found little to no association between the pres- ence of astigmatism and the presence and progression of myopic refractive errors.
While there is some equivocal evidence, there does appear to be an association between astigmatism and the develop- ment and progression of myopia. The exact nature of this relationship and the mechanisms underlying it are not fully understood.
ASTIGMATISM IN ETHNIC GROUPS
The studies that have been discussed up to this point have generally been con- ducted on populations consisting of pre- dominantly healthy Caucasian subjects. Studies of populations with different eth- nic backgrounds (particularly those with higher incidences of astigmatism) may provide further insight into the aetiology of astigmatism. Several different ethnic groups appear to exhibit an increased prevalence of astigmatism.
Subjects of Native American ethnic origin have an increased prevalence of high levels of astigmatism, particularly WTR.52–57 The recent study by Harvey,
Dobson and Miller57 on a population of Native American school children, found that 42 per cent of subjects exhibited ocu- lar astigmatism of 1.00 D or greater. This high degree of astigmatism is corneal in origin55,56 and it has been postulated that these high degrees of WTR astigmatism may relate to heredity or nutritional fac- tors.52,53,55,58 Lyle, Grosvenor and Kean53
postulated that poor nutrition may lead to reduced corneal rigidity and result in increased corneal astigmatism due to pres- sure from the upper eyelid causing the cornea to become flatter in the horizontal meridian and steeper in the vertical.
There is also an increased prevalence of astigmatism in some populations of East Asian subjects.10,59–61 Kame, Jue and Shigekuni60 presented retrospective longi- tudinal data on changes in corneal astig- matism in a clinical population of East Asian…
Journal compilation © 2007 Optometrists Association Australia 5
C L I N I C A L A N D E X P E R I M E N T A L
OPTOMETRY
Key words: aberrations, astigmatism, cornea, corneal topography, refractive error
Astigmatism is a commonly encountered refractive error, accounting for about 13 per cent of the refractive errors of the human eye.1 Our knowledge of astigma- tism appears to have begun in the early 1800s when Thomas Young reported on his own astigmatism but it was not until 1825 that the first cylindrical lens was used by George Airy for the purpose of correct- ing his own astigmatic refractive error.2
Since these early explorations, there has been a great deal of research carried out into various aspects of astigmatism. One reason for this research interest is the fact that the presence of astigmatism appears to have the potential to influence normal visual development. The presence of high
degrees of astigmatism is associated with the development of amblyopia3–5 and some associations have also been noted between astigmatism and the develop- ment of myopia.6–10 Advances in technol- ogy and instrumentation mean that our ability to measure, define and analyse the eye’s optical and shape properties (includ- ing astigmatism) have improved markedly in recent years.
Despite extensive research, the exact cause of astigmatism is still not known. One possible reason for astigmatic devel- opment would be a genetic aetiology. Other possible causes include mechanical interactions between the cornea and the eyelids and/or the extraocular muscles or
a visual feedback model in which astigma- tism develops in response to visual cues. In this review we will consider the various hypotheses regarding the aetiology of astigmatism and examine the evidence in the literature for these theories. We will also present some new evidence from recent research in our laboratory that has investigated the role of near work and eye- lid forces on corneal shape and refractive error development.
COMPONENTS OF ASTIGMATISM
Ocular astigmatism can occur as a result of unequal curvature along the two prin- cipal meridia of the anterior cornea
Scott A Read PhD Michael J Collins PhD Leo G Carney DSc Contact Lens and Visual Optics Laboratory, School of Optometry, Queensland University of Technology, Brisbane, Queensland, Australia E-mail: [email protected]
Astigmatism is a refractive condition encountered commonly in clinical practice. This review presents an overview of research that has been carried out examining various aspects of this refractive error. We examine the components of astigmatism and the research into the prevalence and natural course of astigmatic refractive errors through- out life. The prevalence of astigmatism in various ethnic groups and diseases and syn- dromes is also discussed. We highlight the extensive investigations that have been conducted into the possible aetiology of astigmatism, however, no single model or theory of the development of astigmatism has been proven conclusively. Theories of the devel- opment of astigmatism based on genetics, extraocular muscle tension, visual feedback and eyelid pressure are considered. Observations and evidence from the literature supporting and contradicting these hypotheses are presented. Recent advances in tech- nology such as wavefront sensors and videokeratoscopes have led to an increased under- standing of ocular astigmatism and with continued improvements in technology, our knowledge of astigmatism and its genesis should continue to grow.
A review of astigmatism and its possible genesis
Submitted: 7 September 2006 Revised: 3 October 2006 Accepted for publication: 10 October 2006
INVITED REVIEW
nloaded from https://onlinelibrary.w
iley O nline L
s and C onditions (https://onlinelibrary.w
iley.com /term
nline L ibrary for rules of use; O
A articles are governed by the applicable C
reative C om
m ons L
Clinical and Experimental Optometry 90.1 January 2007
6
Journal compilation © 2007 Optometrists Association Australia
(known as corneal astigmatism) and/or it may be due to the posterior cornea, unequal curvatures of the front and back surfaces of the crystalline lens, decentra- tion or tilting of the lens or unequal refrac- tive indices across the crystalline lens (known as internal or residual astigma- tism). The combination of the corneal and the internal astigmatism gives the eye’s total astigmatism (that is, total astigmatism equals corneal astigmatism plus internal astigmatism). Corneal astigmatism is often classified according to the axis of asti- gmatism as being either with-the rule (WTR), oblique or against-the-rule (ATR) (Figure 1). In the past, astigmatism has been defined as ‘regular’ or ‘irregular’. Typically, irregular astigmatism is used to describe a variety of asymmetric aberra- tions such as coma, trefoil and quadrafoil. The widely adopted use of Zernike poly- nomials to describe the detailed compo- nents of the eye’s optics has made the use of the term ‘irregular’ astigmatism largely redundant.
A recent study investigating corneal topography has classified astigmatism according to the changes occurring in the astigmatism of the peripheral cornea.11
Corneal astigmatism was classified as being stable, reducing or increasing in the peripheral cornea. Of the subjects with significant corneal astigmatism tested in this study, astigmatism was found most commonly to be reducing (47 per cent of astigmatic subjects) or stable (44 per cent) in the peripheral cornea. Figure 2 illustrates these forms of corneal astigmatism.
CORNEAL AND INTERNAL ASTIGMATISM
It is well accepted that there is some rela- tionship between the eye’s corneal and internal astigmatism. In 1890, Javal pro- posed a rule that predicted the total astig- matism of the eye based on the corneal astigmatism.12 Javal’s rule states:
where At is the total astigmatism and Ac is the corneal astigmatism. The terms k and
A k p At c= + ( )
Figure 1. Example of the classification of corneal astigmatism according to the axis. Astigmatism can be classified as either with-the-rule (WTR) (where the steepest corneal meridian is oriented approximately vertically) (left), against-the-rule (ATR) (where the steepest corneal meridian is oriented close to horizontal) (right) or as oblique (where the steepest corneal meridian is oriented at an oblique angle) (centre). Axial curvature corneal topography maps are shown here for three different subjects.
Figure 2. Examples of two forms of corneal astigmatism. The maps on the left illus- trate corneal astigmatism that is stable in the peripheral cornea (or astigmatism that extends out into the peripheral cornea). The maps on the right illustrate corneal astigmatism that reduces in the peripheral cornea (or astigmatism that is primarily confined to the central cornea). Axial power maps are displayed at the top and only the cylinder power is plotted in the lower maps (for both the central and peripheral cornea).
14440938, 2007, 1, D ow
nloaded from https://onlinelibrary.w
iley O nline L
s and C onditions (https://onlinelibrary.w
iley.com /term
nline L ibrary for rules of use; O
A articles are governed by the applicable C
reative C om
m ons L
Clinical and Experimental Optometry 90.1 January 2007
7
Journal compilation © 2007 Optometrists Association Australia
p are constants approximated by 0.5 and 1.25, respectively. This rule relies on the fact that residual astigmatism is thought to be constant and ATR in most people (that is, -0.50 D ATR).
Grosvenor, Quintero and Perrigin13 sug- gested a simplification of Javal’s rule. Regression analysis was carried out to investigate the relationship between cor- neal and total astigmatism. The slope of this regression line is equivalent to the constant ‘p’ (from Javal’s rule), and the y intercept is equivalent to constant ‘k’. The slope of the regression line was found to be slightly less than one, and the y inter- cept close to 0.5. Based on these results, the authors proposed a simplified Javal’s rule of At = Ac - 0.5. This simplified rule was found to fit their data more closely than the original Javal’s rule, which sug- gests that an internal astigmatism of mag- nitude 0.5 D is relatively constant across subjects with different amounts of corneal astigmatism.
Keller and colleagues14 investigated the relationship between corneal and total astigmatism by measuring corneal astig- matism with a computer-assisted videok- eratoscope. The corneal topographical data were converted into a best fit sphero- cylinder for a number of different pupil sizes and subjective refraction was mea- sured using the same pupil sizes. Corneal astigmatism was plotted against total astig- matism for the different pupil sizes and the relationship between corneal and total astigmatism was found to be inde- pendent of pupil size. The results from this study supported Javal’s rule as simpli-
fied by Grosvenor, Quintero and Perrigin (1988).
Kelly, Mihashi and Howland15 used an instrument that allowed simultaneous cap- ture of corneal and total eye aberrations on a population of young subjects. They found that some corneal aberrations are compensated by the internal optics of the eye, including horizontal/vertical astigma- tism, lateral coma and spherical aberra- tion. They suggested that the horizontal/ vertical astigmatism compensation is an active process determined through a fine-tuning, emmetropisation process. No significant compensation was found for oblique astigmatism in this population.
Dunne, Elawad and Barnes16 investi- gated residual astigmatism, by measuring the difference between ocular and total astigmatism (by cylindrical decomposi- tion). The average residual astigmatism was found to be -0.46 × 98.2° for right eyes and -0.50 × 99.4° for left eyes. In ap- proximately two-thirds of eyes, the axis of the residual astigmatism was found to be perpendicular to the axis of corneal astigmatism.
Several studies have investigated the astigmatism contributed by the posterior corneal surface.17–20 These studies have found levels of astigmatism for the poste- rior cornea ranging from 0.18–0.31 D. The curvature of the posterior cornea combined with the refractive index differ- ence between the cornea and the aqueous means that the posterior corneal astigma- tism is of opposite sign to that of the ante- rior cornea. Therefore, the compensation of corneal astigmatism by the eye’s inter-
nal optics can be attributed, in part, to the astigmatism of the posterior cornea.
The compensation of corneal astigma- tism by the internal optics of the eye has been known for many years.12,15,16 The numerous studies into Javal’s rule tend to indicate that this compensation is a pas- sive process (that is, the majority of the population has approximately 0.5 D of internal astigmatism, opposite in sign to the corneal astigmatism). Some authors15
have suggested the possibility of an active ‘feedback driven’ process operat- ing to reduce the total astigmatism of the eye (particularly horizontal/vertical astigmatism).
PREVALENCE OF ASTIGMATISM AND CHANGES WITH AGE
There have been many studies that have attempted to define the prevalence of astigmatism in the population and to illus- trate the typical changes that occur in astigmatism throughout life. These inves- tigations provide some clues to the pos- sible causes of astigmatism. Figure 3 illustrates the typical changes that occur in astigmatism throughout life.
Astigmatism in early life (infancy and early childhood) Generally, studies have shown that in the first months of life, infants exhibit a high prevalence of significant degrees of astig- matism,21–30 which appears to be corneal in origin.24,27,29 The cornea of newborns is steep and exhibits large degrees of astig- matism.27,29,31 Isenberg and co-workers29
Figure 3. The typical changes that occur in astigmatism throughout life
Early childhood
· Most common axis ATR?
Adulthood
Older adulthood
40+ years
· Shift in corneal astigmatism axis towards ATR being most common
14440938, 2007, 1, D ow
nloaded from https://onlinelibrary.w
iley O nline L
s and C onditions (https://onlinelibrary.w
iley.com /term
nline L ibrary for rules of use; O
A articles are governed by the applicable C
reative C om
m ons L
Clinical and Experimental Optometry 90.1 January 2007
8
Journal compilation © 2007 Optometrists Association Australia
used videokeratoscopy to measure the cor- neal curvature of newborns (up to eight days after birth) and found an average of six dioptres of corneal astigmatism. Stud- ies have also shown that the steepest, most astigmatic corneas occur in the newborns with the lowest birth weight and lowest post-conceptional age.27 While studies have consistently found high degrees of corneal astigmatism to be present in infancy, there is some conflicting evidence of the most common axis of astigmatism. Perhaps indicating the difficulties of obtaining accurate measurements on new- born infants or suggesting a large amount of variability in the corneal shape of infants, some studies have found a pre- dominance of WTR corneal astigma- tism,26,29,30 while others have shown a predominance of ATR corneal astigma- tism in infants.22–25,27
As infants grow older, the prevalence of high degrees of astigmatism typically reduces or, in other words, an emmetropi- sation of the astigmatic refractive error occurs.21–29 Dobson, Fulton and Sebris22
and Gwiazda and colleagues23 found a shift in astigmatism from a predominance of higher degrees of ATR astigmatism in children younger than four years, to a pre- dominance of low levels of WTR astigma- tism in children older than four years. Gwiazda and colleagues23 postulated that pressure from the eyelids on the cornea over time may be causing the shift in astig- matic axis from ATR to WTR in children.
Studies of preschool-age children gen- erally show a relatively low prevalence of high degrees of astigmatism (that is, greater than one dioptre) that is predom- inantly WTR in nature.32–34 Huynh and associates34 investigated a large population of six-year-old children and found that only 4.8 per cent of children exhibited greater than one dioptre of ocular astig- matism and 75 per cent of subjects exhib- ited WTR corneal astigmatism.
In summary, at birth children exhibit a high incidence of astigmatism that is cor- neal in origin. As children grow older, the cornea flattens with significantly reduced astigmatism. Over the age of four years, the prevalence of large amounts of astigmatism is low, with small
amounts of WTR astigmatism being found most commonly.
Astigmatism in adults Astigmatism in young adults (younger than 40 years) occurs commonly but in relatively low amounts.35,36 In an investiga- tion of young adults aged 20 to 30 years, Satterfield36 found that 63 per cent of sub- jects exhibited 0.25 D or more of ocular astigmatism, however, the majority of sub- jects with measurable astigmatism exhib- ited less than one dioptre. In a cross- sectional study, Fledelius and Stubgaard37
found that 46 per cent of the total popu- lation had corneal astigmatism of greater than 0.5 D but only 4.7 per cent of the population exhibited greater than 1.5 D of corneal astigmatism. Generally, studies have shown that in young adults, WTR astigmatism occurs most commonly.35,37–42
With increasing age, a general shift in the axis of astigmatism is found from a predominance of WTR astigmatism (in adults younger than 40 years) to a pre- dominance of ATR astigmatism (in adults older than 40 years).35,38–40,42,43 This shift in astigmatic axis in older age appears to be due to changes in corneal curvature.38–40,42
In a cross-sectional study of corneal and total astigmatism, Anstice38 found that internal astigmatism remained relatively stable over time and that changes in astig- matism throughout life were due prima- rily to changes in corneal curvature. Baldwin and Mills39 investigated longitudi- nal changes in corneal and total astigma- tism in patients over a 40-year period and found a steepening of the cornea and an increase in ATR astigmatism with aging. The majority of this change in astigmatism was due to corneal change, that is, a steep- ening of the horizontal meridian of the cornea. As will be discussed later, this change in corneal curvature may be related to the reduction in tension of the eyelids that typically occurs with age.
In summary, young adult subjects typi- cally display small degrees of WTR astig- matism and in older adult years a shift in astigmatism occurs where ATR astigma- tism becomes more prevalent. Astigma- tism most commonly occurs due to the curvature of the cornea and the changes
in astigmatism that occur throughout life also appear to be due primarily to corneal change.
ASTIGMATISM IN RIGHT AND LEFT EYES
There is widespread agreement that some degree of symmetry exists between the refractive errors of right and left eyes. Sev- eral studies have noted mirror symmetry to occur between the axes of astigmatism of right and left eyes.16,44,45 McKendrick and Brennan41 measured corneal and ocular refraction (with autorefraction and autokeratometry) for both eyes in a group of subjects. The mean and spread of astig- matic errors was similar for right and left eyes. The axes of corneal and total astig- matism were found to be similar between the two eyes.46 Most subjects were found to display either mirror (for example, right eye axis 10°, left eye axis 170°) or direct (for example, right eye axis 10°, left eye axis 10°) symmetry of their astigmatic axes. There was no predominance of either mirror or direct symmetry of astig- matic axes when analysis was carried out for the population. Figure 4 illustrates the corneal topography from a normal subject who shows mirror symmetry between the corneal astigmatism of the right and left eyes.
ASTIGMATISM AND OTHER REFRACTIVE ERRORS
There is some evidence to suggest that the presence of astigmatism may be associated with the presence of spherical refractive errors. The presence of astigmatism has been found to be associated with myopic refractive errors, that is, astigmatism was associated with higher degrees of myo- pia.6–10,47,48 Fulton, Hansen and Petersen6
suggested that uncorrected astigmatic errors influenced the development of myopia and that the optical blur from uncorrected astigmatism may be a trigger for myopic development. The presence and changes in astigmatism have been found by some investigators to be associ- ated with an increased progression of myopia.6,10,49 In a longitudinal study of
14440938, 2007, 1, D ow
nloaded from https://onlinelibrary.w
iley O nline L
s and C onditions (https://onlinelibrary.w
iley.com /term
nline L ibrary for rules of use; O
A articles are governed by the applicable C
reative C om
m ons L
Clinical and Experimental Optometry 90.1 January 2007
9
refractive error, Gwiazda and colleagues7
found that their subjects exhibiting signif- icant ATR astigmatism and myopia in infancy were more likely to develop myo- pia at school age. In contrast with these studies, other investigators50,51 have found little to no association between the pres- ence of astigmatism and the presence and progression of myopic refractive errors.
While there is some equivocal evidence, there does appear to be an association between astigmatism and the develop- ment and progression of myopia. The exact nature of this relationship and the mechanisms underlying it are not fully understood.
ASTIGMATISM IN ETHNIC GROUPS
The studies that have been discussed up to this point have generally been con- ducted on populations consisting of pre- dominantly healthy Caucasian subjects. Studies of populations with different eth- nic backgrounds (particularly those with higher incidences of astigmatism) may provide further insight into the aetiology of astigmatism. Several different ethnic groups appear to exhibit an increased prevalence of astigmatism.
Subjects of Native American ethnic origin have an increased prevalence of high levels of astigmatism, particularly WTR.52–57 The recent study by Harvey,
Dobson and Miller57 on a population of Native American school children, found that 42 per cent of subjects exhibited ocu- lar astigmatism of 1.00 D or greater. This high degree of astigmatism is corneal in origin55,56 and it has been postulated that these high degrees of WTR astigmatism may relate to heredity or nutritional fac- tors.52,53,55,58 Lyle, Grosvenor and Kean53
postulated that poor nutrition may lead to reduced corneal rigidity and result in increased corneal astigmatism due to pres- sure from the upper eyelid causing the cornea to become flatter in the horizontal meridian and steeper in the vertical.
There is also an increased prevalence of astigmatism in some populations of East Asian subjects.10,59–61 Kame, Jue and Shigekuni60 presented retrospective longi- tudinal data on changes in corneal astig- matism in a clinical population of East Asian…
Related Documents