Ann R Coll Surg Engl 2002; 84: 100-105 Original article A combined medical and surgical approach to hydatid disease: 12 years' experience at the Hospital for Tropical Diseases, London HM Ayles', EL Corbett', I Taylor2, AGA Cowie2, J Blighl, K Walmsley3, ADM Bryceson' 'Hospital For Tropical Diseases, Mortimer Market Centre, London, UK 'Department of Surgery, Royal Free and University College Medical School, London, UK 3Department of Imaging, University College London Hospitals NHS Trust, London, UK Background: There is no consensus as to the most appropriate treatment for the varied and often complicated presentations of hydatid disease in Britain. We looked at our own results over a 12- year period to see if a consistent and logical plan had emerged. Patients and Methods: 70 patients presenting between 1986 and 1998 were analysed retrospectively, with regard to their presentation, diagnosis, treatment and outcome, with particular reference to the use of chemotherapy, and to the difficulties of post-treatment assessment by serology and imaging. Results: 37 patients had been treated previously. 35 had hepatic cysts and 26 multiple cysts. 4 patients were treated by surgery alone, 44 by chemotherapy and surgery, and 14 by chemotherapy alone. The combined use of albendazole and praziquantel pre-operatively reduced significantly the number of cysts that contained viable protoscolices: 1/25 versus 5/8 that received albendazole alone (P = 0.00013). During the 12-year period, it became our policy to aim for 3 months drug treatment (albendazole throughout with praziquantel for 2 weeks), re-assess and proceed either to surgery or to continue with chemotherapy. Conclusions: It is possible to construct an algorithm for the management of patients with hydatid disease by chemotherapy and surgery, but the assessment of results by indirect techniques remains difficult. Key words: Hydatid disease - Albendazole - Praziquantel ydatid disease is a common zoonosis caused by the The cysts are often asymptomatic until they reach a large larval cysts of Echinococcus granulosus. The disease is size, press on neighbouring structures or leak or rupture, endemic in parts of the world where there is intimate thereby causing allergic reactions and releasing their contact between man and the definitive and intermediate contents and disseminating the disease. Until recently, the hosts, usually sheep and dogs. Hydatid cysts most mainstay of treatment has been surgical. Over the last 15 commonly form in the liver, but may occur in any organ. years, two chemotherapeutic agents (albendazole and Ann R Coll Surg Engl 2002; 84 Correspondence to: Prof. I Taylor, Department of Surgery, Royal Free and University College Medical School, 67-73 Riding House Street, London WlW 7EJ, UK. Tel: +44 207 679 9312; Fax: +44 207 636 5176; E-mail: [email protected] The Royal College of Surgeons of England 100

A combined medical and surgical approach to hydatid disease: 12 years' experience at the Hospital for Tropical Diseases, London
Dec 19, 2022
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
Original article
A combined medical and surgical approach to hydatid disease: 12 years' experience at the Hospital for Tropical Diseases, London
HM Ayles', EL Corbett', I Taylor2, AGA Cowie2, J Blighl, K Walmsley3, ADM Bryceson'
'Hospital For Tropical Diseases, Mortimer Market Centre, London, UK 'Department of Surgery, Royal Free and University College Medical School, London, UK 3Department ofImaging, University College London Hospitals NHS Trust, London, UK
Background: There is no consensus as to the most appropriate treatment for the varied and often complicated presentations of hydatid disease in Britain. We looked at our own results over a 12- year period to see if a consistent and logical plan had emerged. Patients and Methods: 70 patients presenting between 1986 and 1998 were analysed retrospectively, with regard to their presentation, diagnosis, treatment and outcome, with particular reference to the use of chemotherapy, and to the difficulties of post-treatment assessment by serology and imaging. Results: 37 patients had been treated previously. 35 had hepatic cysts and 26 multiple cysts. 4 patients were treated by surgery alone, 44 by chemotherapy and surgery, and 14 by chemotherapy alone. The combined use of albendazole and praziquantel pre-operatively reduced significantly the number of cysts that contained viable protoscolices: 1/25 versus 5/8 that received albendazole alone (P = 0.00013). During the 12-year period, it became our policy to aim for 3 months drug treatment (albendazole throughout with praziquantel for 2 weeks), re-assess and proceed either to surgery or to continue with chemotherapy. Conclusions: It is possible to construct an algorithm for the management of patients with hydatid disease by chemotherapy and surgery, but the assessment of results by indirect techniques remains difficult.
Key words: Hydatid disease - Albendazole - Praziquantel
ydatid disease is a common zoonosis caused by the The cysts are often asymptomatic until they reach a large larval cysts of Echinococcus granulosus. The disease is size, press on neighbouring structures or leak or rupture,
endemic in parts of the world where there is intimate thereby causing allergic reactions and releasing their contact between man and the definitive and intermediate contents and disseminating the disease. Until recently, the hosts, usually sheep and dogs. Hydatid cysts most mainstay of treatment has been surgical. Over the last 15 commonly form in the liver, but may occur in any organ. years, two chemotherapeutic agents (albendazole and
Ann R Coll Surg Engl 2002; 84
Correspondence to: Prof. I Taylor, Department of Surgery, Royal Free and University College Medical School, 67-73 Riding House Street, London WlW 7EJ, UK. Tel: +44 207 679 9312; Fax: +44 207 636 5176; E-mail: [email protected]
The Royal College of Surgeons of England
100
A COMBINED MEDICAL AND SURGICAL APPROACH TO HYDATID DISEASE: 12 YEARS' EXPERIENCE
praziquantel) have become available, but there are still no clear indications or evidenced-based guidelines for their use." 2 The ideal management for patients with operable disease remains uncertain. We have retrospectively analysed the management and operative complications of 70 cases of hydatid disease presenting to the Hospital for Tropical Diseases during the last 12 years, to assess the impact of these newer therapeutic strategies and to attempt to define a coherent policy for management.
were found for 70 (95%) of these patients. Fifty-nine patients (84%) presented during the study period; the rest had first presented with hydatid disease between 1964 and 1986 and were still under active surveillance or treatment. Of the 70 patients, 43 (61%) were male and 27 (39%) were female. The median age at diagnosis was 32 years (range, 10-78 years). Patients came from many countries (Table 1). Occupational and travel histories suggested that 10 of the 15 cases from England and Wales had acquired their hydatid disease whilst travelling abroad.
Patients and Methods
All patients presenting with suspected hydatid disease to the Hospital for Tropical Diseases from 1986 to 1998 were identified and case notes retrieved. The case notes were reviewed by two doctors (EC and HA) and data entered and analysed using epi-info v. 6 (CDC, Atlanta, GA, USA).
Details of management were extracted from the notes and outcomes were judged on clinical, laboratory and radiological assessment.
Diagnosis of hydatid disease was made by a combination of radiological, ultrasonic and serological tests and by examination of cyst material for the presence of protoscolices. Serological tests induded enzyme linked immunosorbent assay (ELISA), complement fixation (CF) and immunoblot.3 Viability of protoscolices was determined by microscopic examiination of cyst fluid, looking for the exclusion of eosin and the presence of flame cells.4 Histology was used to assess viability of germinal membrane in operative specimens.
Patients were followed up with repeated serological testing and serial imaging.
Results
Patients
A total of 74 patients who attended the Hospital for Tropical Diseases between June 1986 and June 1998 were identified retrospectively from laboratory and hospital records as suffering from hydatid disease. Clinical records
Table 1 Country oforigin ofpatients
Country of origin Number (%) Most likely place hydatid acquired (%)
England/Wales 15 (21.4) 5 (7.1) Cyprus 13 (18.6) 14 (20) Turkey 12 (17.1) 15 (21.4) Middle East 12 (17.1) 13 (18.6) Indian subcontinent 8 (11.4) 9 (12-9) Rest of Europe 6 (8.6) 6 (8.6) Africa 4 (5.7) 6 (8.6)
In 2 cases the place where the disease was acquired could not be identified.
Presentation
The most common presenting symptom was abdominal pain, reflecting the site of disease. Presenting symptoms had frequently been mistaken for other pathologies, because of failure to consider the diagnosis or to take an adequate geographical history. The most common incorrect diagnoses were cholecystitis or appendicitis (for abdominal hydatid disease) and non-resolving pneumonia (for those with chest symptoms). Some asymptomatic cases were detected by routine medical screening or by screening of family members of known hydatid cases.
Previous treatment
Thirty-seven (53%) patients had previously received treatment. Of these, 34 had previously undergone surgery, 2 in combination with drug therapy. Three patients had received drug therapy alone, one with albendazole and 2 with mebendazole. Of the 34 patients who had undergone previous surgery, 15 (44%) had done so abroad. Twenty-three (68%) underwent 1 operation and the remainder 2-9 operations. The diagnosis was known at the time of surgery in only 21 (64%) cases.
Diagnosis and assessment of disease
Hydatid disease was diagnosed by the combination of characteristic radiology and positive serology in the majority of our patients.
Table 2 Site of disease
Site Number (%)
Liver only 33 (47.8) Other abdomen/pelvis 15 (21.7) Chest only 8 (11.6) Both sides of diaphragm 6 (8.7) Bony 5 (7.2) Other 2 (2.9)
1 patient had no cysts on referral to the Hospital for Tropical Diseases.
Ann R Coll Surg Engl 2002; 84
AYLES
101
A COMBINED MEDICAL AND SURGICAL APPROACH TO HYDATID DISEASE: 12 YEARS' EXPERIENCE
Table 3 Number of cysts identified in each patient
Number of cysts Number (%)
2-5 21 (30) >5 5(7.1)
Unknown 8 (11.4)
The site and number of cysts were determined by radiology or ultrasound scanning. The most common site of disease was liver alone in 33 patients (48%; Table 2). Half had one cyst and 37% had 2 or more (Table 3).
Serology
ELISA was performed in 62 cases and was positive in 54 of these (87%).
Treatment
After assessment, 48 patients were treated surgically (44 of them in combination with drug therapy), 14 patients were treated with drug therapy alone, and 8 patients received no treatment either because their cysts were thought to be dead or they were considered to have received adequate therapy elsewhere.
Drug treatment
A total of 39 patients received albendazole and praziquantel in combination and 19 received albendazole alone; 12 received no drug therapy (8 with no treatment and 4 who had surgery alone). The regimen of drugs received reflected the date of presentation. No patient was treated with praziquantel alone.
Praziquantel was given for a median of 2 weeks (range, 1-40 weeks) at a dose of 50 mg/kg/day. Albendazole was given for a median of 3 months (range 1-60 months) at a dose of 400 mg twice daily; adverse drug effects were recorded in 11 patients, 5 with nausea and 6 with abnormal liver function tests. Therapy was discontinued in 2 patients due to deranged liver function.
During this 12-year period, it became our policy to aim for 3 months' drug treatment before surgery, albendazole throughout and praziquantel for 2 weeks, and to assess the response to treatment or progression of the disease after this initial treatment course. In those patients assessed in this way, 29 out of 58 (50%) were considered to have shown clinical evidence of response (defined as a reduction in symptoms), 20 out of 57 (35%) showed laboratory evidence of response (defined as a reduction in serological optical density or eosinophil count) and 22 out of 58 (38%) showed radiological evidence of response (defined by a reduction in cyst size on imaging). None showed unequivocal evidence,
by these indirect tests, that the parasite had been killed or the disease cured.
Surgery
Surgery was performed on 48 patients at a median of 6.5 months after presentation (range, 0-240 months). We have classified the timing of surgery into early (<3 months) normal (3-12 months) and late (>12 months). Twelve patients received early surgery, either because they were seen before drug treatment became routine policy or because of impending or actual rupture or of secondary bacterial infection within a cyst. Thirteen patients received late, usually palliative surgery for multiple disease or because of concomitant problems.
Thirty-two patients underwent abdominal surgery, 3 thoracic surgery and 4 combined thoraco-abdominal surgery. The other cases involved a variety of sites including bone and pelvis. In total, 41 patients received anti-scolicidal drugs prior to surgery (albendazole, mebendazole, prazi- quantel or a combination).
The most common operation was pericystectomy using a freezing cone (46% overall). Only four were simple aspirations.
The operation of pericystectomy using a freezing cone involves mobilisation of the liver and dissection of the hydatid cyst within the liver so that it is sufficiently mobile to enable a truncated metal cone to be placed on its surface. By circulating nitrous oxide gas through a tube situated in its narrow rim, the cone becomes sealed to the surface of the cyst wall by ice thus preventing spillage of content into the peritoneal cavity. In addition, the area was isolated with silver nitrate soaked packs. A circular eclipse of the cyst wall was excised using a
pointed knife and sent for histology. The cyst contents were then aspirated or physically removed, usually with sponge holding forceps. The cavity was repeatedly irrigated with silver nitrate until all evidence of scolices and hydatid material had been removed. The cavity was then carefully inspected for evidence of bile leakage. If small biliary radicals were seen they were oversewn. The contents of the cyst cavity were sent separately to parasitology to test for active disease. Following cystectomy, the residual cavity was filled with mobilised omentum.
In three cases, there was rupture of the cyst with intra- operative leakage. Evidence of bile fistulae was present in 10 patients but these settled spontaneously; although in one patient the fistula drained for nearly one year.
Parasitological assessment
Cyst material from the surgical procedure was assessed for viability either by eosin exclusion or by histology. Of 25
Ann R Coll Surg Engl 2002; 84
AYLES
102
A COMBINED MEDICAL AND SURGICAL APPROACH TO HYDATID DISEASE: 12 YEARS' EXPERIENCE
patients receiving combination albendazole/praziquantel in whom it was possible to obtain operative material, viable protoscolices were demonstrated in only 1 (4%) compared with 5 out of 8 patients (63%) receiving albendazole alone. This difference is highly statistically significant (Fisher's exact test P = 0.0013). Treatment regimen was not however randomised.
Recurrence
Recurrence was suspected in 25 patients after treatment and confirmed in 12. Those in whom it was not confirmed were found to have another pathology or a complication of the residual cyst cavity with secondary infection within the cyst cavity. Confirmed recurrence occurred at a median of 23 months after initial therapy (range, 2-144 months). Recurrence did not seem to be associated with the type of treatment received initially. This lack of association could be due to the small numbers involved. Recurrence was commonest in bony disease (4 out of 5 patients).
Outcome
Patients were followed for a median of 30 months (range, 1-340 months). Three patients have died, none as a direct consequence of their hydatid disease or surgery. When last assessed, 51 (73%) were considered to be 'cured' of their hydatid disease, 58 (83%) had residual radiological abnormalities, usually cystic cavities, and 30 (42%) had unoperated cysts, either due to the large number of initial cysts, inoperable position or cysts which were considered to be non-viable. Of 66 patients with symptoms, 13 (20%) had persistent pain and 4 (6%) were physically disabled as a consequence of their hydatid bone disease.
Discussion
The experience of hydatid disease that we have presented is anecdotal reflecting routine clinical practice, but it serves to highlight the changes in available treatment for hydatid disease over the last decade. With the availability of newer drug treatments, there is a glaring lack of consensus for management of hydatid disease and a lack of evidence on which to base this management.
The most widely studied drug used against hydatid is the benzimidazole compound albendazole.5 Albendazole sulphoxide, the active metabolite, reaches predictable levels in the serum after an oral dose, but levels in cyst fluid are slow to rise, less predictable and may not reach therapeutic levels (-200 ig/1).6'7 Albendazole is extremely effective in vitro and in animal models against both cyst ultrastructure8 and protoscolices.7 A randomised,
controlled trial in humans demonstrated a decrease in viability of cysts and protoscolices as well as disintegration of cyst wall membrane.9 To achieve these benefits, albendazole must be given at high dosage for a prolonged period, but the optimum duration for a given type of disease has not been determined. Previous studies have also shown that medical therapy works best in young, small cysts but works poorly in bone hydatid.10 Other agents have been investigated, notably praziquantel. Searching the literature is disappointing as only one report of 4 patients treated with a combination of albendazole and praziquantel was found.11 These patients showed good response to medication without surgery. Praziquantel is well absorbed and, in a few days at conventional doses, produces predictable levels in serum and cyst fluid that are well in excess of those required to kill protoscolices. 2-14 It also acts synergistically with albendazole against protoscolices in vitro.15 However, at dosages that can be used in humans, it does not produce levels adequate to kill the germinal membrane nor does it enhance the effect of albendazole on the germinal membrane.16
Conventional surgical procedures, although successful in the vast majority, may be a major undertaking and have a high complication rate especially at the second or third attempt (44% overall in our series). Similar complication rates have been found in other series.17-19 An advantage of conventional surgery is the removal of bulk disease and the obliteration of cyst cavities, which if left can become secondarily infected. More recently, less invasive procedures have been explored. Studies of laparoscopic techniques20 have shown good results as has percutaneous drainage under ultrasonic guidance.2' The main risk from these minimally invasive procedures is that of cyst rupture and leakage of contents causing dissemination of disease.
The complications of both conventional and minimally invasive surgery can be minimised by the adjunctive use of oral anti-scolicidal agents peri-operatively," and it would seem logical to give a combination of praziquantel with albendazole to sterilise the cyst contents.15 No standard approach to the treatment of hydatid
disease has emerged, partly due to the advances in treatment but mainly due to the fact that it is a chronic disease where treatment effect is hard to measure. Commonly-used markers of viability are the eosinophil count and serological tests, combined with sequential radiological assessment, but surveillance must be for many years and there is no test for 'cure'. A variety of serological tests exist for the detection of hydatid disease.4 Previous studies have compared the sensitivity and specificity of these tests and found the ELISA to be most sensitive.23 At the Hospital for Tropical Diseases, an ELISA is the main test used with a sensitivity of -90% and
Ann R Coll Surg Engl 2002; 84
AYLES
103
A COMBINED MEDICAL AND SURGICAL APPROACH TO HYDATID DISEASE: 12 YEARS' EXPERIENCE
a specificity of -96% in this laboratory (unpublished data). Cases with borderline positivity are subjected to further testing using either CFT or immunoblot. During their period of follow-up, our patients had a series of ELISA tests sometimes showing a gradual decline in optical density, but rarely becoming negative even after 10 years, demonstrating the problems of using this test to establish cure. Antigen detection may be more useful for follow-up than serology,24 but the assay is not available. Newer tests are required to help in this problem.
hnaging too was unreliable in establishing parasito- logical cure. Even if chemotherapy kills the parasite, the cyst may remain. Dead cysts and postoperative defects could not always be distinguished from viable cysts.
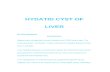
No 'long-term' data exist for the efficacy of medical therapy alone and, therefore, from our experience at the Hospital for Tropical Diseases we have developed an algorithm which combines medical and surgical management for this complex disease (Fig. 1). We consider that medical therapy with albendazole and praziquantel should be used as an adjunct to surgery. In 19 patients who received albendazole alone, at a dose of approximately 10 mg/kg for an average duration of 12 weeks, radiographic improvement was seen in 7 (37%). In those patients proceeding to surgery, 63% of cysts contained viable protoscolices (as determined by eosin exclusion). By contrast, of 40 patients who received dual therapy with praziquantel and albendazole, 15 (38%, the same proportion as in those receiving albendazole alone) showed radiographic evidence of improvement but at surgery only 4% of cysts contained viable protoscolices (P < 0.0013 compared to albendazole alone). For most hepatic cysts, 2 weeks praziquantel and 3 months albendazole should be given to kill all protoscolices, damage or kill the genrinal membrane, reduce cyst pressure and make surgery easier and safer. If re-assessment at 3 months shows that the cyst is disappearing, albendazole may be continued. The actual time necessary to kill a susceptible cyst is unknown - 3 months is probably inadequate; we tend to give it for 1 year and then re- assess. Even though chemotherapy may kill the parasite, the cyst may not collapse norbe absorbed. The dead material may become secondarily infected and re-present as an abscess. We would also recommend medical therapy with 1
year of albendazole in cases with inoperative disease, multi-site disease and in patients too unwell or unwilling to undergo surgery. After one year, the disease may be so reduced in volume that surgery becomes a possibility. Bony disease has a poor outcome despite the combination of drug therapy and surgery.
In our series, adverse effects from albendazole were uncommon. Of our cases, 15% had a transient rise in liver enzymes but these abnormalities settled spontaneously when the drug was stopped. In one patient, with extensive bony and pelvic disease, we pushed albendazole treatment
Management plan
Early surgery Delayed or no surgery * leakage not settling Plan for prolonged on drug therapy albendazole if:
* intolerable symptomns Plan for elective surgery * multicystic disease * dangerous site after * inoperable site
* 2 weeks praziquantel * recurrent disease * 4-12 weeks * patient unfit
Follow albendazole * patient preference (unless pulmonary)
Reassess after 1st drug treatment block
Figure 1 Algorithm for the management of hydatid disease.
to the point of causing jaundice; liver function normalised when the drug…
A combined medical and surgical approach to hydatid disease: 12 years' experience at the Hospital for Tropical Diseases, London
HM Ayles', EL Corbett', I Taylor2, AGA Cowie2, J Blighl, K Walmsley3, ADM Bryceson'
'Hospital For Tropical Diseases, Mortimer Market Centre, London, UK 'Department of Surgery, Royal Free and University College Medical School, London, UK 3Department ofImaging, University College London Hospitals NHS Trust, London, UK
Background: There is no consensus as to the most appropriate treatment for the varied and often complicated presentations of hydatid disease in Britain. We looked at our own results over a 12- year period to see if a consistent and logical plan had emerged. Patients and Methods: 70 patients presenting between 1986 and 1998 were analysed retrospectively, with regard to their presentation, diagnosis, treatment and outcome, with particular reference to the use of chemotherapy, and to the difficulties of post-treatment assessment by serology and imaging. Results: 37 patients had been treated previously. 35 had hepatic cysts and 26 multiple cysts. 4 patients were treated by surgery alone, 44 by chemotherapy and surgery, and 14 by chemotherapy alone. The combined use of albendazole and praziquantel pre-operatively reduced significantly the number of cysts that contained viable protoscolices: 1/25 versus 5/8 that received albendazole alone (P = 0.00013). During the 12-year period, it became our policy to aim for 3 months drug treatment (albendazole throughout with praziquantel for 2 weeks), re-assess and proceed either to surgery or to continue with chemotherapy. Conclusions: It is possible to construct an algorithm for the management of patients with hydatid disease by chemotherapy and surgery, but the assessment of results by indirect techniques remains difficult.
Key words: Hydatid disease - Albendazole - Praziquantel
ydatid disease is a common zoonosis caused by the The cysts are often asymptomatic until they reach a large larval cysts of Echinococcus granulosus. The disease is size, press on neighbouring structures or leak or rupture,
endemic in parts of the world where there is intimate thereby causing allergic reactions and releasing their contact between man and the definitive and intermediate contents and disseminating the disease. Until recently, the hosts, usually sheep and dogs. Hydatid cysts most mainstay of treatment has been surgical. Over the last 15 commonly form in the liver, but may occur in any organ. years, two chemotherapeutic agents (albendazole and
Ann R Coll Surg Engl 2002; 84
Correspondence to: Prof. I Taylor, Department of Surgery, Royal Free and University College Medical School, 67-73 Riding House Street, London WlW 7EJ, UK. Tel: +44 207 679 9312; Fax: +44 207 636 5176; E-mail: [email protected]
The Royal College of Surgeons of England
100
A COMBINED MEDICAL AND SURGICAL APPROACH TO HYDATID DISEASE: 12 YEARS' EXPERIENCE
praziquantel) have become available, but there are still no clear indications or evidenced-based guidelines for their use." 2 The ideal management for patients with operable disease remains uncertain. We have retrospectively analysed the management and operative complications of 70 cases of hydatid disease presenting to the Hospital for Tropical Diseases during the last 12 years, to assess the impact of these newer therapeutic strategies and to attempt to define a coherent policy for management.
were found for 70 (95%) of these patients. Fifty-nine patients (84%) presented during the study period; the rest had first presented with hydatid disease between 1964 and 1986 and were still under active surveillance or treatment. Of the 70 patients, 43 (61%) were male and 27 (39%) were female. The median age at diagnosis was 32 years (range, 10-78 years). Patients came from many countries (Table 1). Occupational and travel histories suggested that 10 of the 15 cases from England and Wales had acquired their hydatid disease whilst travelling abroad.
Patients and Methods
All patients presenting with suspected hydatid disease to the Hospital for Tropical Diseases from 1986 to 1998 were identified and case notes retrieved. The case notes were reviewed by two doctors (EC and HA) and data entered and analysed using epi-info v. 6 (CDC, Atlanta, GA, USA).
Details of management were extracted from the notes and outcomes were judged on clinical, laboratory and radiological assessment.
Diagnosis of hydatid disease was made by a combination of radiological, ultrasonic and serological tests and by examination of cyst material for the presence of protoscolices. Serological tests induded enzyme linked immunosorbent assay (ELISA), complement fixation (CF) and immunoblot.3 Viability of protoscolices was determined by microscopic examiination of cyst fluid, looking for the exclusion of eosin and the presence of flame cells.4 Histology was used to assess viability of germinal membrane in operative specimens.
Patients were followed up with repeated serological testing and serial imaging.
Results
Patients
A total of 74 patients who attended the Hospital for Tropical Diseases between June 1986 and June 1998 were identified retrospectively from laboratory and hospital records as suffering from hydatid disease. Clinical records
Table 1 Country oforigin ofpatients
Country of origin Number (%) Most likely place hydatid acquired (%)
England/Wales 15 (21.4) 5 (7.1) Cyprus 13 (18.6) 14 (20) Turkey 12 (17.1) 15 (21.4) Middle East 12 (17.1) 13 (18.6) Indian subcontinent 8 (11.4) 9 (12-9) Rest of Europe 6 (8.6) 6 (8.6) Africa 4 (5.7) 6 (8.6)
In 2 cases the place where the disease was acquired could not be identified.
Presentation
The most common presenting symptom was abdominal pain, reflecting the site of disease. Presenting symptoms had frequently been mistaken for other pathologies, because of failure to consider the diagnosis or to take an adequate geographical history. The most common incorrect diagnoses were cholecystitis or appendicitis (for abdominal hydatid disease) and non-resolving pneumonia (for those with chest symptoms). Some asymptomatic cases were detected by routine medical screening or by screening of family members of known hydatid cases.
Previous treatment
Thirty-seven (53%) patients had previously received treatment. Of these, 34 had previously undergone surgery, 2 in combination with drug therapy. Three patients had received drug therapy alone, one with albendazole and 2 with mebendazole. Of the 34 patients who had undergone previous surgery, 15 (44%) had done so abroad. Twenty-three (68%) underwent 1 operation and the remainder 2-9 operations. The diagnosis was known at the time of surgery in only 21 (64%) cases.
Diagnosis and assessment of disease
Hydatid disease was diagnosed by the combination of characteristic radiology and positive serology in the majority of our patients.
Table 2 Site of disease
Site Number (%)
Liver only 33 (47.8) Other abdomen/pelvis 15 (21.7) Chest only 8 (11.6) Both sides of diaphragm 6 (8.7) Bony 5 (7.2) Other 2 (2.9)
1 patient had no cysts on referral to the Hospital for Tropical Diseases.
Ann R Coll Surg Engl 2002; 84
AYLES
101
A COMBINED MEDICAL AND SURGICAL APPROACH TO HYDATID DISEASE: 12 YEARS' EXPERIENCE
Table 3 Number of cysts identified in each patient
Number of cysts Number (%)
2-5 21 (30) >5 5(7.1)
Unknown 8 (11.4)
The site and number of cysts were determined by radiology or ultrasound scanning. The most common site of disease was liver alone in 33 patients (48%; Table 2). Half had one cyst and 37% had 2 or more (Table 3).
Serology
ELISA was performed in 62 cases and was positive in 54 of these (87%).
Treatment
After assessment, 48 patients were treated surgically (44 of them in combination with drug therapy), 14 patients were treated with drug therapy alone, and 8 patients received no treatment either because their cysts were thought to be dead or they were considered to have received adequate therapy elsewhere.
Drug treatment
A total of 39 patients received albendazole and praziquantel in combination and 19 received albendazole alone; 12 received no drug therapy (8 with no treatment and 4 who had surgery alone). The regimen of drugs received reflected the date of presentation. No patient was treated with praziquantel alone.
Praziquantel was given for a median of 2 weeks (range, 1-40 weeks) at a dose of 50 mg/kg/day. Albendazole was given for a median of 3 months (range 1-60 months) at a dose of 400 mg twice daily; adverse drug effects were recorded in 11 patients, 5 with nausea and 6 with abnormal liver function tests. Therapy was discontinued in 2 patients due to deranged liver function.
During this 12-year period, it became our policy to aim for 3 months' drug treatment before surgery, albendazole throughout and praziquantel for 2 weeks, and to assess the response to treatment or progression of the disease after this initial treatment course. In those patients assessed in this way, 29 out of 58 (50%) were considered to have shown clinical evidence of response (defined as a reduction in symptoms), 20 out of 57 (35%) showed laboratory evidence of response (defined as a reduction in serological optical density or eosinophil count) and 22 out of 58 (38%) showed radiological evidence of response (defined by a reduction in cyst size on imaging). None showed unequivocal evidence,
by these indirect tests, that the parasite had been killed or the disease cured.
Surgery
Surgery was performed on 48 patients at a median of 6.5 months after presentation (range, 0-240 months). We have classified the timing of surgery into early (<3 months) normal (3-12 months) and late (>12 months). Twelve patients received early surgery, either because they were seen before drug treatment became routine policy or because of impending or actual rupture or of secondary bacterial infection within a cyst. Thirteen patients received late, usually palliative surgery for multiple disease or because of concomitant problems.
Thirty-two patients underwent abdominal surgery, 3 thoracic surgery and 4 combined thoraco-abdominal surgery. The other cases involved a variety of sites including bone and pelvis. In total, 41 patients received anti-scolicidal drugs prior to surgery (albendazole, mebendazole, prazi- quantel or a combination).
The most common operation was pericystectomy using a freezing cone (46% overall). Only four were simple aspirations.
The operation of pericystectomy using a freezing cone involves mobilisation of the liver and dissection of the hydatid cyst within the liver so that it is sufficiently mobile to enable a truncated metal cone to be placed on its surface. By circulating nitrous oxide gas through a tube situated in its narrow rim, the cone becomes sealed to the surface of the cyst wall by ice thus preventing spillage of content into the peritoneal cavity. In addition, the area was isolated with silver nitrate soaked packs. A circular eclipse of the cyst wall was excised using a
pointed knife and sent for histology. The cyst contents were then aspirated or physically removed, usually with sponge holding forceps. The cavity was repeatedly irrigated with silver nitrate until all evidence of scolices and hydatid material had been removed. The cavity was then carefully inspected for evidence of bile leakage. If small biliary radicals were seen they were oversewn. The contents of the cyst cavity were sent separately to parasitology to test for active disease. Following cystectomy, the residual cavity was filled with mobilised omentum.
In three cases, there was rupture of the cyst with intra- operative leakage. Evidence of bile fistulae was present in 10 patients but these settled spontaneously; although in one patient the fistula drained for nearly one year.
Parasitological assessment
Cyst material from the surgical procedure was assessed for viability either by eosin exclusion or by histology. Of 25
Ann R Coll Surg Engl 2002; 84
AYLES
102
A COMBINED MEDICAL AND SURGICAL APPROACH TO HYDATID DISEASE: 12 YEARS' EXPERIENCE
patients receiving combination albendazole/praziquantel in whom it was possible to obtain operative material, viable protoscolices were demonstrated in only 1 (4%) compared with 5 out of 8 patients (63%) receiving albendazole alone. This difference is highly statistically significant (Fisher's exact test P = 0.0013). Treatment regimen was not however randomised.
Recurrence
Recurrence was suspected in 25 patients after treatment and confirmed in 12. Those in whom it was not confirmed were found to have another pathology or a complication of the residual cyst cavity with secondary infection within the cyst cavity. Confirmed recurrence occurred at a median of 23 months after initial therapy (range, 2-144 months). Recurrence did not seem to be associated with the type of treatment received initially. This lack of association could be due to the small numbers involved. Recurrence was commonest in bony disease (4 out of 5 patients).
Outcome
Patients were followed for a median of 30 months (range, 1-340 months). Three patients have died, none as a direct consequence of their hydatid disease or surgery. When last assessed, 51 (73%) were considered to be 'cured' of their hydatid disease, 58 (83%) had residual radiological abnormalities, usually cystic cavities, and 30 (42%) had unoperated cysts, either due to the large number of initial cysts, inoperable position or cysts which were considered to be non-viable. Of 66 patients with symptoms, 13 (20%) had persistent pain and 4 (6%) were physically disabled as a consequence of their hydatid bone disease.
Discussion
The experience of hydatid disease that we have presented is anecdotal reflecting routine clinical practice, but it serves to highlight the changes in available treatment for hydatid disease over the last decade. With the availability of newer drug treatments, there is a glaring lack of consensus for management of hydatid disease and a lack of evidence on which to base this management.
The most widely studied drug used against hydatid is the benzimidazole compound albendazole.5 Albendazole sulphoxide, the active metabolite, reaches predictable levels in the serum after an oral dose, but levels in cyst fluid are slow to rise, less predictable and may not reach therapeutic levels (-200 ig/1).6'7 Albendazole is extremely effective in vitro and in animal models against both cyst ultrastructure8 and protoscolices.7 A randomised,
controlled trial in humans demonstrated a decrease in viability of cysts and protoscolices as well as disintegration of cyst wall membrane.9 To achieve these benefits, albendazole must be given at high dosage for a prolonged period, but the optimum duration for a given type of disease has not been determined. Previous studies have also shown that medical therapy works best in young, small cysts but works poorly in bone hydatid.10 Other agents have been investigated, notably praziquantel. Searching the literature is disappointing as only one report of 4 patients treated with a combination of albendazole and praziquantel was found.11 These patients showed good response to medication without surgery. Praziquantel is well absorbed and, in a few days at conventional doses, produces predictable levels in serum and cyst fluid that are well in excess of those required to kill protoscolices. 2-14 It also acts synergistically with albendazole against protoscolices in vitro.15 However, at dosages that can be used in humans, it does not produce levels adequate to kill the germinal membrane nor does it enhance the effect of albendazole on the germinal membrane.16
Conventional surgical procedures, although successful in the vast majority, may be a major undertaking and have a high complication rate especially at the second or third attempt (44% overall in our series). Similar complication rates have been found in other series.17-19 An advantage of conventional surgery is the removal of bulk disease and the obliteration of cyst cavities, which if left can become secondarily infected. More recently, less invasive procedures have been explored. Studies of laparoscopic techniques20 have shown good results as has percutaneous drainage under ultrasonic guidance.2' The main risk from these minimally invasive procedures is that of cyst rupture and leakage of contents causing dissemination of disease.
The complications of both conventional and minimally invasive surgery can be minimised by the adjunctive use of oral anti-scolicidal agents peri-operatively," and it would seem logical to give a combination of praziquantel with albendazole to sterilise the cyst contents.15 No standard approach to the treatment of hydatid
disease has emerged, partly due to the advances in treatment but mainly due to the fact that it is a chronic disease where treatment effect is hard to measure. Commonly-used markers of viability are the eosinophil count and serological tests, combined with sequential radiological assessment, but surveillance must be for many years and there is no test for 'cure'. A variety of serological tests exist for the detection of hydatid disease.4 Previous studies have compared the sensitivity and specificity of these tests and found the ELISA to be most sensitive.23 At the Hospital for Tropical Diseases, an ELISA is the main test used with a sensitivity of -90% and
Ann R Coll Surg Engl 2002; 84
AYLES
103
A COMBINED MEDICAL AND SURGICAL APPROACH TO HYDATID DISEASE: 12 YEARS' EXPERIENCE
a specificity of -96% in this laboratory (unpublished data). Cases with borderline positivity are subjected to further testing using either CFT or immunoblot. During their period of follow-up, our patients had a series of ELISA tests sometimes showing a gradual decline in optical density, but rarely becoming negative even after 10 years, demonstrating the problems of using this test to establish cure. Antigen detection may be more useful for follow-up than serology,24 but the assay is not available. Newer tests are required to help in this problem.
hnaging too was unreliable in establishing parasito- logical cure. Even if chemotherapy kills the parasite, the cyst may remain. Dead cysts and postoperative defects could not always be distinguished from viable cysts.
No 'long-term' data exist for the efficacy of medical therapy alone and, therefore, from our experience at the Hospital for Tropical Diseases we have developed an algorithm which combines medical and surgical management for this complex disease (Fig. 1). We consider that medical therapy with albendazole and praziquantel should be used as an adjunct to surgery. In 19 patients who received albendazole alone, at a dose of approximately 10 mg/kg for an average duration of 12 weeks, radiographic improvement was seen in 7 (37%). In those patients proceeding to surgery, 63% of cysts contained viable protoscolices (as determined by eosin exclusion). By contrast, of 40 patients who received dual therapy with praziquantel and albendazole, 15 (38%, the same proportion as in those receiving albendazole alone) showed radiographic evidence of improvement but at surgery only 4% of cysts contained viable protoscolices (P < 0.0013 compared to albendazole alone). For most hepatic cysts, 2 weeks praziquantel and 3 months albendazole should be given to kill all protoscolices, damage or kill the genrinal membrane, reduce cyst pressure and make surgery easier and safer. If re-assessment at 3 months shows that the cyst is disappearing, albendazole may be continued. The actual time necessary to kill a susceptible cyst is unknown - 3 months is probably inadequate; we tend to give it for 1 year and then re- assess. Even though chemotherapy may kill the parasite, the cyst may not collapse norbe absorbed. The dead material may become secondarily infected and re-present as an abscess. We would also recommend medical therapy with 1
year of albendazole in cases with inoperative disease, multi-site disease and in patients too unwell or unwilling to undergo surgery. After one year, the disease may be so reduced in volume that surgery becomes a possibility. Bony disease has a poor outcome despite the combination of drug therapy and surgery.
In our series, adverse effects from albendazole were uncommon. Of our cases, 15% had a transient rise in liver enzymes but these abnormalities settled spontaneously when the drug was stopped. In one patient, with extensive bony and pelvic disease, we pushed albendazole treatment
Management plan
Early surgery Delayed or no surgery * leakage not settling Plan for prolonged on drug therapy albendazole if:
* intolerable symptomns Plan for elective surgery * multicystic disease * dangerous site after * inoperable site
* 2 weeks praziquantel * recurrent disease * 4-12 weeks * patient unfit
Follow albendazole * patient preference (unless pulmonary)
Reassess after 1st drug treatment block
Figure 1 Algorithm for the management of hydatid disease.
to the point of causing jaundice; liver function normalised when the drug…
Related Documents