Glucocorticoids (GC): GC are among the most effective anti-inflammatory and immunosuppressive therapeutic options, and have thus become a cornerstone of therapy for many rheumatic disorders – but check place-in-therapy. - Place in Therapy: Used as adjunctive therapy in combination with other DMARDs. RA is the only disease in which GC therapy is often started and maintained at a low dose as additional therapy. Highly effective,<10mg/day - Joint-Sparing Effect: Theorized to be based on the inhibition of pro-inflammatory cytokines IL-1 and TNF TNFa: Major player in pro-inflammatory response, induces more cytokine production, expression of adhesion molecules - Forms: The two forms of TNFa are related by TACE, the TNFa Converting Enzyme o Membrane-Bound: TNFa (26kDa) o Soluble TNFa (17kDa) - Receptors: Though similar, the two TNFa receptors differ in their intracellular domain and signaling pathway o TNFR-1: Constitutively expressed in all tissues, capable of inducing apoptosis via Death Domain. § Internalized TNF recruits TRADD, leading to DNA degradation and cell death. o TNFR-2: Only expressed on Immune cells, capable of inducing NFkB signaling pathways § Activation recruits TRAF2, activating NFkBà Production of cytokines, inhibition of apoptosis § Produces: pro-inflammatory TNFa and IL-1b, Upregulation of Adhesion molecules (ICAMs) - Targets for Inhibition of TNFa: TNFa molecule, TNFR, TACE, Signaling pathway, NFkB Infliximab (Remicade): Biological DMARD - Chimeric (25% murine, 75% human) mAb - MoA: “Neutralize Cytokines”. Bind and neutralize both Soluble and Membrane-bound TNFa - AE: Infusion Rxn (itch, flush, N), HA, Abdominal pain. o Increased risk of infection due to immunosuppression. (URTI – Tuberculosis) o Increased risk of non-Hodgkins lymphoma o Immunogenicity: Patient develops HAMA (human anti-nouse Ab) towards Infliximab. Thus, we efficacy has a limited timeline, which can be extended by concurrent immunosuppressive therapy. Tocilizumab (Actemra): Biological DMARD – Humanized mAb - First anti-IL6R mAb approved for arthritis, used for moderate to severe RA for those who have failed an anti- TNF. IL-6 is a chemical messenger involved in destructive immune responses, found overproduced in the joints - MoA: “Receptor Blockade”, targets the IL-6 receptor Abatacept (Orencia): Biological DMARD – Fusion Protein Checkpoint Inhibitor - MoA: Modified IgG domain recognizes CD80/86, binds and prevents CD28 interaction, producing negative feedback to inhibit T cell activation and inhibiting inflammatory cytokine production Janus Kinase Inhibitors: The first oral DMARD (2012) – newest drugs to combat RA - Drug: Tofacitinib (Xeljanz) - MoA: Jakinhibs interrupt signaling downstream of a multiplicity of cytokines by inhibiting cytokine receptors, rather than blocking one cytokine at a time. AE: Increased serious infections (Infection-risk) (12/1) Chevalier Lecture: Rheumatoid Arthritis Epidemiology: Affecting 1-2% of people world-wide, this disease affects 3x as many women as men and is one of the most common causes of disability. It has been associated with decreased life expectancy - Risk Factors: Smoking (x3, and worse prognosis!), Genetic Susceptibility (mom/dad? +6%), Gender specific factors (hormones?), Occupational exposure, infectious triggers, presence of autoantibodies (RF, anti-CCP) Pathophysiology: Autoimmune disease characterized by an imbalance of pro-/anti-inflammatory cytokines. Patients present with chronic inflammation and proliferation of synovial tissue (Synovitis), which can invade the cartilage and bone producing erosions ~ breakdown of bone in the joint space. Once damaged, it is irreversible Clinical Presentation: RA is usually a disease of the small joints - Symmetrical Joint Swelling (Synovitis) - Morning Stiffness lasting ³ 1 hour - Low-grade fever, weight loss, fatigue, weakness, loss of appetite - Joint pain, tenderness, and muscle aches - In the hands, the Proximal interphalangeal and Metacarpophalangeal joints are most commonly affected - Late Complications: Ulnar Deviation, Boutonniere deformities, and Muscular atrophy. Bony erosions. Significant difficulty performing Activities of Daily Living (ADLs)

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
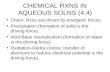
Glucocorticoids (GC): GC are among the most effective anti-inflammatory and immunosuppressive therapeutic options, and have thus become a cornerstone of therapy for many rheumatic disorders – but check place-in-therapy.
- Place in Therapy: Used as adjunctive therapy in combination with other DMARDs. RA is the only disease in which GC therapy is often started and maintained at a low dose as additional therapy. Highly effective,<10mg/day
- Joint-Sparing Effect: Theorized to be based on the inhibition of pro-inflammatory cytokines IL-1 and TNF TNFa: Major player in pro-inflammatory response, induces more cytokine production, expression of adhesion molecules
- Forms: The two forms of TNFa are related by TACE, the TNFa Converting Enzyme o Membrane-Bound: TNFa (26kDa) o Soluble TNFa (17kDa)
- Receptors: Though similar, the two TNFa receptors differ in their intracellular domain and signaling pathway o TNFR-1: Constitutively expressed in all tissues, capable of inducing apoptosis via Death Domain.
§ Internalized TNF recruits TRADD, leading to DNA degradation and cell death. o TNFR-2: Only expressed on Immune cells, capable of inducing NFkB signaling pathways
§ Activation recruits TRAF2, activating NFkBà Production of cytokines, inhibition of apoptosis § Produces: pro-inflammatory TNFa and IL-1b, Upregulation of Adhesion molecules (ICAMs)
- Targets for Inhibition of TNFa: TNFa molecule, TNFR, TACE, Signaling pathway, NFkB Infliximab (Remicade): Biological DMARD - Chimeric (25% murine, 75% human) mAb
- MoA: “Neutralize Cytokines”. Bind and neutralize both Soluble and Membrane-bound TNFa - AE: Infusion Rxn (itch, flush, N), HA, Abdominal pain.
o Increased risk of infection due to immunosuppression. (URTI – Tuberculosis) o Increased risk of non-Hodgkins lymphoma o Immunogenicity: Patient develops HAMA (human anti-nouse Ab) towards Infliximab. Thus, we efficacy
has a limited timeline, which can be extended by concurrent immunosuppressive therapy. Tocilizumab (Actemra): Biological DMARD – Humanized mAb
- First anti-IL6R mAb approved for arthritis, used for moderate to severe RA for those who have failed an anti-TNF. IL-6 is a chemical messenger involved in destructive immune responses, found overproduced in the joints
- MoA: “Receptor Blockade”, targets the IL-6 receptor Abatacept (Orencia): Biological DMARD – Fusion Protein Checkpoint Inhibitor
- MoA: Modified IgG domain recognizes CD80/86, binds and prevents CD28 interaction, producing negative feedback to inhibit T cell activation and inhibiting inflammatory cytokine production
Janus Kinase Inhibitors: The first oral DMARD (2012) – newest drugs to combat RA - Drug: Tofacitinib (Xeljanz) - MoA: Jakinhibs interrupt signaling downstream of a multiplicity of cytokines by inhibiting cytokine receptors,
rather than blocking one cytokine at a time. AE: Increased serious infections (Infection-risk) (12/1) Chevalier Lecture: Rheumatoid Arthritis Epidemiology: Affecting 1-2% of people world-wide, this disease affects 3x as many women as men and is one of the most common causes of disability. It has been associated with decreased life expectancy
- Risk Factors: Smoking (x3, and worse prognosis!), Genetic Susceptibility (mom/dad? +6%), Gender specific factors (hormones?), Occupational exposure, infectious triggers, presence of autoantibodies (RF, anti-CCP)
Pathophysiology: Autoimmune disease characterized by an imbalance of pro-/anti-inflammatory cytokines. Patients present with chronic inflammation and proliferation of synovial tissue (Synovitis), which can invade the cartilage and bone producing erosions ~ breakdown of bone in the joint space. Once damaged, it is irreversible Clinical Presentation: RA is usually a disease of the small joints
- Symmetrical Joint Swelling (Synovitis) - Morning Stiffness lasting ³ 1 hour - Low-grade fever, weight loss, fatigue, weakness, loss of
appetite - Joint pain, tenderness, and muscle aches - In the hands, the Proximal interphalangeal and
Metacarpophalangeal joints are most commonly affected - Late Complications: Ulnar Deviation, Boutonniere
deformities, and Muscular atrophy. Bony erosions. Significant difficulty performing Activities of Daily Living (ADLs)
RA Disease Course: Most commonly, RA has a gradual rather than abrupt onset. Patients will experience a waxing and waning of inflammation, that progressively worsens correlating with structural changes. Eventually, joint destruction and deformity ensues.
- Extra-Articular Manifestations: Occurring in 40% of patients, it is critical to assume and monitor for complications such as: Vasculitis, Interstitial Lung Disease, Myositis, CAD, CHF, PVD, Anemia, Neutropenia
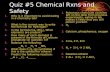
Diagnostic Criteria for Rheumatoid Arthritis - American College of Rheumatology (ACR): RA Diagnostic Criteria: Put out in 1987, but still used
o At least 4 of 7: Morning Stiffness, Arthritis in ³ 3 joint areas, Arthritis of hand joints, Symmetric Arthritis, Rheumatoid Nodules, Serum Rheumatoid Factor (RF, also anti-CCP), Radiographic changes
- ACR/EULAR Modified Criteria: Released in 2010, aimed to diagnose disease earlier for studies and trials o ³ 6 Points = Definite RA. Points distributed to 4 categories: o Joint Involvement o Serology: RF and anti-CCP(occurs in 70% of cases, but predicts with 97-99% of confidence RA dx) o Acute Phase Reactants: Monitor CRP and ESR (Sed. Rate), Used to monitor medication efficacy o Duration of Symptoms: Viral infection may present similar to RA, \ ³ 6weeks à rule out viral
- Evaluating Disease Activity – During Treatment, utilize the DAS28 Score to monitor treatment progress o DAS28: Disease Activity Score. Scored 0-9.4, this is the most commonly used tool by physicians treating
RA. Major Components: Inflammatory Markers (CRP, ESR) and ADL interview. (Remission < 2.6) Treatment Goals
Control Disease: Prevent Joint Destruction Alleviate Pain Maintain ADLs
Maximize QoL Ultimate Goal: No swelling, pain, stiffness, fatigue, à Induce complete remission
Non-Pharmacologic Therapy - Rest the joint, rest your body. Get 8 hours of sleep nightly - Physical Therapy (PT): Maintaining passive range of motion and engaging in exercise will help maintain joint
function and muscular integrity. Achievement of Ideal Body Weight (IBW) is ideal ;) - Stop Smoking Now.
Non-DMARDs - Corticosteroids
o Drugs: PO (Prednisone, Methylprednisolone) and IV (Triamcinolone, Methylprednisolone) o Function: Control symptoms quickly (days), Offer some anti-erosive effects. o Indication: First-line therapy for the treatment of Acute Flares (higher doses). May be used at low doses
(<7.5mg/day) chronically for maintenance. May be used Systemically or Intra-articularly o Limitations: Highly preferred to avoid corticosteroid long-term use due to adverse effects. Try to add a
disease-modifying (steroid-sparing) agent, like [Osteoporosis = Bisphosphonates], [HyperTG = Statin] o Monitoring: BP, CMP, Glucose (hyperglycemia), WeightÝ, HT, Weight and fluid retention, Cataracts
- NSAIDs o Function: Used for anti-inflammatory effects, analgesic effect is merely an additional benefit o Dosing: Must be taken regularly, continuously, to be effective. Effect may take 2-3 weeks. o Monitoring: BP, CBC, SCr, LFT
Prior to DMARD Therapy - Understand the Risk: Many DMARDs are hepatotoxic, some are CV damaging, and all are Myelosuppressive - Labs: Serology, Titers, Organ Function - Vaccinations: Avoid live attenuated vaccines while on biologic DMARDs! Killed vaccines only. - Tests/Exams: Consider ECHO, Infection history - Therapy Initiation: START ASAP! DMARDs can help reduce the progression of the disease, and take a while (1-
3mo) to work. Begin as soon as possible, providing Coverage with an NSAID or ‘Roid until it kicks in. DMARDs- Non-Biological - MTX, SSZ, HCQ, LFN –
- Methotrexate (MTX) Cornerstone of therapy o Place in Therapy: Initial DMARD in most cases, prevalent in later stages. o MoA: Dihydrofolate reductase inhibitor, inhibiting purine synthesis leading to reduced cell turnover of
dividing cells. Additionally, it inhibits production of IL-1 (pro-inflammatory) o Dosing: Initial Dose 10mg PO/qWeekly, max 25mg weekly. 2.5mg tabs. Onset 1-2mo
§ Supplement with 1-3mg/qday Folic Acid to decrease stomatitis, N/D, Alopecia o ContraX: Boozers, Pregnancy (Teratogenic, X), Renal/Liver Impairment, Lung disease
DMARD? = Disease-Modifying Anti-Rheumatic Drugs
- Leflunomide (LFN) Alt to MTX o Place in Therapy: Used as an alternative to MTX, ~equal efficacy and toxicity. o MoA: Dihydroorotate dehydrogenase inhibitor, inhibiting pyrimidine synthesis leading to reduced
lymphocyte production. o Tox: Enterohepatic Recirculationà Long half-life, up to 2 years to eliminate, (Teratogenic, X)
- Sulfasalazine (SSZ) To be used in combo with HCQ ± MTX o Place in Therapy: Used in combination with HCQ or MTX. Onset in 1-3mo o AE: Major GI (N/V/D) which wane over time (take with food), Rash. Sulfa allergy
§ Skin and urine may turn orange, educate them that its ok to be a carrot o Warfarin DDI: Protein-binding issue, SSZ knocks off Warfarin, INRÝ
- Hydroxychloroquine (HCQ) Slow and nice comforting med to be used in combo with SSZ±MTX o Place in Therapy: Used in combination with SSZ and/or MTX. Slow onset, 2-6mo o MoA: Downregulates the immune response by reducing antigen processing by pH adjustment, thus
lowering APC activities. o AE: Well-tolerated, watch for GI or rash. o Ocular Toxicity: Potential for corneal crystal deposits. Get yearly eye exams! Sx? à D/c!
§ Sx: blurry vision/decreased vision. Will resolve upon d/c. § Retinopathy: Irreversible damage that is asymptomatic, a bull’s eye maculopathy. Loss of
peripheral vision, slowly progressing to loss of central vision § Risk factors: High dose, high cumulative dose, Renal/hepatic impairment, old, eye issues
- Pregnancy/Fertility Concerns in Non-biologic DMARDs o HCQ and SSZ = Ok! Ok for breast feeding and pregnancy o MTX: Category X. Avoid in Pregnancy and Breastfeeding. D/C 3mo before tryna conceive o LFN: Category X. Avoid in Pregnancy and Breastfeeding. Requires Washout if tryna conceive
§ Wash-Out: Without wash out, may take up to 2 years to reach low Teriflunomide levels • Cholestyramine 8g TID x11d -OR- Act. Charcoal Suspension 50g BID x11d
Advancement of DMARD Therapy – Therapy should be modified if: - (1) Repetitive Flares, (2) Unacceptable Disease Activity, (3) Progressive Joint Damage - Add a bDMARD or Jak Inhibitor if continued activity on non-bioDMARDs
o Options: Monotherapy of bDMARD or increased combination therapy o Anti-TNFa therapies are generally first-line in this case, due to efficacy and clinical experience
DMARDs- Biologic - - Administered parenterally (SubQ, IV), bDMARDs begin to show efficacy rather quickly (days-weeks) compared
to non-bioDMARDs, with their maximal improvement in 12-16 weeks. They’ve been used in other immune-related disorders, such as ankylosing spondylitis, CD, and UC. Unfortunately, they are expensive with serious side effects and often require prior authorizations from their insurance.
- Place in Therapy: Used in Moderate-Severe RA as mono- or combination with non-bioDMARDs. It can be used as a steroid sparing agent, and patients generally continue their current non-bioDMARDs.
- Serious Overlapping AE: Do NOT combine ³ 1 bDMARD. Infection, Malignancy, Neutropenia, Injection site rxns, Antibody formation (low dose MTX helps prevent Ab formation and prolongs drug’s utility)
- Anti-TNFa Agents: First-line biologics due to (1) Efficacy, (2) Fast onset, (3) SubQ dosing o Choosing: There is no evidence that any one Anti-TNF is better than another, may switch within class o Understanding the Risks: Infection, Malignancy, Skin Cancer, Hepatosplenic T-Cell Lymphoma
§ Infection Risk: Patients are susceptible to opportunistic invaders, TB/latentTB, HepB reactivation • TB Test performed before initiating therapy
o (+) à Get X-Ray à (+) à Check Sputum for AFB à (+) à Specialist! o LTB identified? Start Isoniazid therapy (x9mo), after 1 month may start anti-TNF o (-) à Start Anti-TNF
• HepB check for Surface Ag and Core Ag before starting § Malignancy Risk: Lymphomas and Leukemia are most common § Skin Cancer: Especially non-melanoma skin cancer
o AE: Psoriasis, Lupus-like syndrome, Injection site rxns, worsening of HF (ContraX Stage 3/4), CNS Demyelinating disorders (Optic neuritis, MS, Seizures), Neutropenia, Hepatotoxicity)
o Pregnancy: Certolizumab is the safest due to minimal placental transfer, though contraindicated in the last trimester of pregnancy. Tofacitinib is the only bDMARD that gets into breast milk
§ Fetus exposed to biologics? Avoid live vaccinations for 6 months (ContraX Rotavirus Vacc)
- Abatacept (Orencia): Soluble fusion protein mimicking CTLA-4 – Inhibiting T cell activation o Efficacy: Onset in 4 weeks, as a result this is often not a chosen therapy. Though SubQ dosing! o AE: HA, URI, Infection, Nausea, Malignancy, Infusion Rxns o ContraX: COPD and Smokers
- Rituximab (Rituxan): Anti-CD20 mAb – Depletes B cells o Dosing: To be used in combination with MTX. Infusion on Day 0, Day 15, then once every 6 months o Advantages: No increased incidence of TB or malignancy. Recommended biologic for patients with
Cancer hx o Disadvantages: Infusion reactions are very intense and common (38-45%)
§ ContraX In CVD patients due to risk of Cardiac Arrhythmias § REMS ‘Touch’: PML risk due to previous JC virus infection - Fatal 30-50% § Cancer Hx + HepB Hx = Reactivation of Hep B [Prescreen for HepB+C]
- IL-6 Inhibitors: Tocilizumab (Actemra), Sarilumab (Kevzara) SubQ formulations o MoA: Decreases IL-6 mediated signaling to slow inflammatory processes o ContraX: ANC<2000 PLT<100,000 (Toc) PLT<150,000 (Sar) ALT/AST > 1.5x ULN o AE: GI perforation and Dyslipidemia (monitor lipids)
- Janus Kinase Inhibitor (JAK)- New class to be used as monotherapy or in combo with MTX o Tofacitinib (Xeljanz): Blocks Jak Stat pathway, thus influencing cellular process of hematopoiesis and
immune cell function § This is an oral medication with excellent bioavailability, requiring 70% liver metabolism and
30% renal excretion. It is ineffective if used with 3A4 inducers, toxic if used with 3A4 inhibitors § AE: Lipid changes, GI perforation, TB infections, malignancy. Avoid using with other
immunosuppressant medications such as AZA, TAC, CSA § ContraX: Using with another bDMARD, ANC<1000, CBC<500, Hb<9
Monitoring: It is critical to understand that monitoring does not always mean we are checking for toxicity or general negative effects. The most important component of therapy to monitor is Efficacy
- Efficacy Monitoring: Presence of inflammation, xray progression, degree of pain, duration of morning stiffness, duration of fatigue, reduction in ESR or CRP (our inflammatory markers), DAS28 scores
- Toxicity Monitoring: Depends on the therapy – Excellent chart, check it
Related Documents