Annual Report 2015 Successful transformation through local collaboration

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

AnnualReport
2015Successful transformation through local collaboration

1
A message from the president:Successful transformation from the ground up On behalf of the Coalition for a Healthy Oregon (COHO) and our member coordinated care organizations (CCOs), I want to thank the hundreds of community partners working with us at the local level to transform health care in Oregon. This includes the CCOs’ community advisory councils, public health and human service departments, elected officials, schools, diverse nonprofit organizations, city and county police and sheriffs’ departments, faith-based organizations, hospitals, medical centers, and especially the health care providers we work with every day.
These partners help COHO members provide quality, patient-centered care in our communities. Leveraging resources efficiently, we are improving health outcomes, providing access to care and lowering costs throughout Oregon’s health care delivery system.
This annual report showcases innovative services and programs that are helping move Oregon forward. In particular, this report illustrates how COHO and our community partners are integrating physical, behavioral and dental health services, breaking down local barriers to care and focusing on prevention.
Yet, uncertainty and challenges remain. COHO’s members are committed to serving Oregonians now and in the future. But CCOs cannot do it alone. CCOs require long-term financial and programmatic stability to be able to make long-term investments in our communities. We must take steps now to ensure sustainability. This is essential to successfully continuing to transform health care for Oregonians.
Collaborative partnerships are also essential to Oregon’s success. Partnerships at all levels, ranging from members at the local community level to state leaders, are absolutely necessary to accomplishing health care transformation. It’s no surprise that all the stories in this report reflect collaboration. That’s how we roll.
In partnership,
Ruth A. Rogers BaumanPresident, Coalition for a Healthy OregonChief Executive Officer, ATRIO Health Plans

1 2
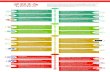
COHO: Serving nearly half of OHP membersThe Coalition for a Healthy Oregon (COHO) is an association of organizations that work with coordinated care organizations (CCOs) or provide direct care as CCOs. We serve nearly half of the state’s Oregon Health Plan (OHP) members.* COHO members are part of our communities. Each of us has a thorough understanding of local health issues, which is the foundation for providing comprehensive, wraparound physical, dental, mental and behavioral health care.
This is what transformation looks like. Our collaborative community partnerships and innovative programs break down barriers and increase access to health care for thousands of Oregonians. The kind of health care that grows healthy kids, prevents costly low-birth-weight babies, supports teen clinics and manages chronic diseases to kick expensive conditions out of the emergency room.
The return on Oregon’s investment can be measured in several ways.
Cost control: Oregon controls costs by paying CCOs a fixed per member payment rather than a costly fee-for-service payment that rewards expensive high-utilization. Thus, CCOs take the risk for any increased health care costs.
Quality care: CCOs provide patient-centered, integrated care that focuses on keeping Oregonians healthy. We keep quality up and costs down. CCOs are accountable to the state via 17 data-driven quality metrics.
Access: CCOs ensure members receive prompt and appropriate care at all levels – again as a way to keep quality up and costs down. For example, the Oregon Health Authority’s most recent metrics analysis, “Oregon’s Health System Transformation 2014 Final Report,” shows that as CCOs increase access to primary care, inappropriate emergency department visits have decreased 22 percent statewide.
* OHP numbers as of October 2015

3
For adults with mental illnesses, accessing appropriate, ongoing health care can be overwhelming — resulting in long gaps in care, overuse of emergency resources and hospital stays. To address this problem, AllCare Health is helping provide integrated health care and social support at Compass House, a community center for adults with mental health issues.
Compass House was founded in 2013 using evidence-based models. It connects members with integrated physical, dental and mental health care, along with social support and opportunities for personal, educational and career advancement.
AllCare Health’s financial support has helped the center develop a speaker’s bureau, present weekly at the Rogue Regional Medical Center’s Behavioral Health Unit, improve transportation support for members and hire a full-time outreach coordinator.
This AllCare Health-funded coordinator contacts inactive Compass House members and encourages them to get connected, and partners with community organizations to identify and reach out to possible new members. The coordinator also works with the in-patient behavioral health unit to contact patients before they’re discharged.
One of these patients was Kahnema. She says, “I used to be isolated and Compass House really helps me connect with others. Staff and the other members are a great source of personal empowerment and encouragement.” So much so that she now serves on several community committees and advocates to break down barriers to care and increase understanding of mental health issues.Compass House’s integrated, whole-person care model helps members manage their illnesses and stay connected to community and health resources.
“This safe, peer-driven environment goes a long way toward improving quality of life and keeping members out of the ER and hospital,” says Heather Hartman, AllCare Health’s Behavioral Integration Manager.
Case in point: In its first year of operation, only three percent of active Compass House members required hospitalization due to mental illness.
Supporting Compass House is just part of AllCare Health’s efforts to integrate physical and behavioral health for better outcomes. It created the community-based Birch Grove Collaborative with La Clinica Del Valle, Jackson County Mental Health, OnTrack and the Addictions Recovery Center in Jackson County.
In Josephine County, AllCare Health partnered with Options for Southern Oregon to develop a Tier III Primary Care Patient-Centered Home Clinic to serve members with chronic mental health conditions. In Curry County, AllCare financially supports Curry Community Health.
Supporting community mental health services
Serving 50,475 Oregonians living in Curry, Jackson, Josephine and southern Douglas counties
Compass House members advocate for better mental health services.

3 4
Overuse of emergency resources isn’t just costly to health care systems. It also keeps patients from getting consistent preventive care and ongoing health management. A collaborative initiative between Umpqua Health Alliance (UHA) and Mercy Medical Center is reducing costs and improving health outcomes by increasing patients’ access to primary care services.
UHA’s Community Care Transition (CCT) team consists of two nurses and two support employees who serve as patient advocates, connecting UHA members with primary care providers and community services after they are discharged from Mercy’s emergency department. CCT was established in October 2014, and in its first year the team had nearly 4,000 patient referrals. In the same timeframe, Mercy saw a decrease in the percentage of patients who were readmitted to the emergency department within 30 days of their last visit.
When a UHA member is admitted to the emergency room, hospital workers collect information about the member’s primary care provider. If the member has no provider or hasn’t established care, he or she signs a release form and the referral team notifies CCT. A team member then contacts the patient to discuss care and any issues that might be a barrier to attending a follow-up primary care appointment.
In the cases where patients aren’t established with a primary care physician or don’t know who their doctor is, the team works to connect them with a clinic. They also work with uninsured patients to start the screening process for OHP benefits. For
patients who have trouble with transportation to and from an appointment, CCT helps coordinate appropriate transportation. And for social needs that arise, transition team members help by connecting patients with local social service organizations.
Of the patients the team is able to reach after discharge, a full 69 percent end up having a successful appointment with a primary care provider. CCT also works to reach “lost” patients who can’t be contacted after several attempts. These patients make up nearly 40 percent of all emergency department referrals.
“These conversations don’t happen in the ED,” says D’Dee Hopkins, Nurse Manager for the CCT team. “We provide patients with access to primary care relationships that will help them get and stay healthy.”
Connecting members from the emergency department to primary care
Serving 26,282 Oregonians living in Douglas County

5
In 2014, Trillium launched the Trillium Integration Incubator Program (TIIP) to pilot a new model of integrated health care for its members. The program tested a progressive, holistic approach to physical care and behavioral health at eight clinics — and it was so successful that Trillium has standardized the integrated model of care, effective April 2016.
Of the eight medical homes that received program startup grants from Trillium, four were primary care clinics and four were behavioral health clinics. Each clinic now includes both physical health and behavioral providers on their care teams, vastly increasing community access to a full range of health care resources.
Here’s how it works: If a member arrives at an appointment to discuss treatment for diabetes and the primary care physician notices symptoms of depression, that member can see a mental health specialist for a same-day visit. In the same way, if a member comes in for mental health services and the provider learns about a physical health issue, a primary care provider is available to assess and treat the person on the spot.
Providers share clinical information and patient medical data in one place, working together to provide holistic care.
This isn’t just an added convenience for Trillium members. It can make the difference between receiving care — or not.
According to TIIP program head and Trillium’s Behavioral Health Medical Services Director Lynnea Lindsey-Pengelly, Ph.D., MSCP, this program bridges the accessibility gap for many members who struggle to show up for appointments. Integrated care increases the likelihood that after patients walk in the door to see mental health providers they already know, they’ll feel comfortable staying to receive the additional care they need. This is also true in the primary care clinic, where patients may access behavioral health services without the possible stigma of going to a mental health agency.
The feeling of safety and the knowledge that staff are adapting to accommodate their needs and changing schedules truly creates access to care — and keeps high-risk members out of the expensive emergency department.
“This system is cost effective for Trillium because it greatly reduces inappropriate visits to the emergency department and hospital admissions,” Dr. Lindsey-Pengelly says. “While it is too preliminary to be exact, we can already tell that the savings will jump off the page for our behavioral health medical homes.
“This is a very progressive approach to health care that defines what transformation really means. This approach gets the right care to the right patient at the right time.”
Making integrated care a reality
Serving 96,267 Oregonians living in Lane County
“This approach gets the right care to the right
patient at the right time.”

5 6
Seventy-five percent of Cascade Health Alliance (CHA) members don’t have access to reliable transportation. This poses significant challenges, especially for those who have chronic illnesses and lack mobility.
The inability to get to medical appointments, pick up prescriptions, attend health-related support groups, and even shop for healthy foods to meet dietary needs is a major obstacle to consistent and successful medical treatment. Over time, a lack of access to ongoing care, medication and other recommended treatments can compound health issues, leading to excessive use of emergency resources, preventable hospital stays and unhealthy communities.
That’s why CHA partnered with Sky Lakes Medical Center to provide high-risk members with improved access to whole-person health care and community resources through a groundbreaking Care Management program, which includes non-emergent medical transportation (NEMT). The program’s objective is to reduce ED use and hospital admissions by increasing attendance at health care appointments and improving care/treatment plan compliance.
For example, a 50-year-old Bonanza resident named Paula was having trouble getting to her primary care appointments due to physical mobility issues. Her husband was unable to get her in and out of their vehicle and she was also unable to use a taxi service. She was stuck at home and had become depressed. When her medical problems worsened, she would go to the ER because the ambulance could transport her.She thought that was her only option. It wasn’t until she got connected with a community health worker that she was able to access the services she needed and see improvements in her health.
“By providing transportation and support to our members, we’re able to get them to their doctor’s office instead of the ER,” says Cristal Neri, community health worker. “A lot of it is educating the patient on how and when to use the ED, as well as clinic’s extended hours and same-day appointments.”
Members like Paula are assigned to community health workers who help dissolve barriers to care by providing a wide range of services, including in-home assistance with meal preparation and physical accommodations, social support and a connection to community services.
The Care Management program started with three vans and three community health workers assigned to CHA-referred high-risk patients. Membership expanded between 2014 and 2015 to include 145 active cases served by five community health workers. The program has also added a registered nurse case manager and two certified nursing assistants.
Paula and Cristal on their way to a clinic appointment.
Breaking down barriers: Sometimes it takes a ride
Serving 17,843 Oregonians living in Klamath County
“By providing transportation and support to our members, we’re able to get them to their
doctor’s office instead of the ER.”

7
Using an innovative strategy that focuses on both intervention and prevention, FamilyCare is working to achieve better health outcomes for Portland area youth between the ages of 15 and 25.
The “transition-age youth” (TAY) population makes up more than 18,000 of FamilyCare’s members. Nearly 75 percent of these individuals come from low-income backgrounds, about half are Hispanic and African American, and many are “hot spotters” — those who frequently use costly emergency services instead of establishing care with a primary health clinic. These young adults may be disconnected from education and employment, many have been involved in the justice and foster care systems, and many lack stable living situations.
“Our health care systems are built on children and adults,” says Meg Pitman, FamilyCare’s Director of Community Partnerships for Transition Age Youth. “There is a big gap in care for youth ages 15 to 25.” She adds that these gaps can lead to costly ED visits, as well as poor health outcomes.
Unfortunately, not enough is known about this population’s needs to serve them effectively — a problem FamilyCare is seeking to resolve with the help of community partners and youth representatives.
FamilyCare is developing a Community Health Improvement Plan (CHIP) that targets 15- to 25-year-olds in the Portland metro region in order to bridge gaps in care. Plan creators are drawing upon many different data sources to inform outreach strategies, including FamilyCare claims data, government and justice system records, national and state statistics, youth surveys and findings from other relevant community plans.
They’re also looking at qualitative data — such as information gleaned from youth listening sessions, interviews with community organizations and youth participation in Community Advisory Councils.
Findings will be used in two ways: First, to engage Portland’s youth with targeted outreach efforts for the purpose of improving health literacy, wellness knowledge and engagement in health care. And second, to educate the various entities that serve these populations in order to increase youth access to health resources.
After analyzing available metrics and gathering information from surveys and listening sessions, the CHIP team will align priorities with efforts that exist and those that don’t — determining where the gaps in care lie, and what can be done to address them.
Several community organizations are already serving youth populations successfully. Knowing this, FamilyCare is placing a strong emphasis on community partnerships. Grant funds have been set aside to help bolster the efforts of the most innovative and successful programs. FamilyCare also partners with existing youth councils, community efforts and health care providers who work successfully with youth.
Youth provide valuable information during a listening session.
Closing gaps in care for youth
Serving 127,568 Oregonians living in Clackamas, Multnomah, Washington and
parts of Marion counties

7 8
PrimaryHealth is increasing the number of members who follow through with behavioral health appointments, thanks to a smart initiative to integrate mental health therapists, as well as alcohol and drug treatment counselors, into primary care clinics in Grants Pass.
PrimaryHealth increased patient access to counselors by bringing mental health and chemical dependency treatment providers directly into primary care offices. They started by funding one full-time therapist to work at Grants Pass Clinic (GPC) and gradually expanded the program to include several providers at multiple primary care clinics.
One primary care provider at GPC says she encounters patients every day who are struggling with mental health symptoms ranging from depression and anxiety to suicidality or biopolar disorder. “This situation is not unique in primary care,” the provider says. “What is unique is the ability to tell my patients, ‘We can help you. There are counselors right here in the clinic who can see you right now if you would like.’ I find myself saying this often, and see the surprise in patients’ eyes when they realize that they won’t have to struggle alone any longer.”
But access is only part of the solution; employees are also working hard to break down emotional barriers to care. Providers have found that personally and warmly introducing patients to therapists on location helps alleviate fear and stress. The caring atmosphere continues when provider teams share information about patients’ progress. It’s an important attitude shift that helps patients feel comfortable and increases the likelihood they’ll return for follow-up appointments.
Through this initiative, PrimaryHealth partnered with Options for Southern Oregon, a nonprofit organization that serves as the community mental health program for Josephine County, as well as its own outpatient chemical dependency treatment center, Choices Counseling Center. Both organizations are now seeing their highest
engagement numbers in history, and are hiring new counselors and providing more services than ever before. Three area pediatricians’ offices have also brought counselors to their clinics after seeing the program’s success with adults.
PrimaryHealth’s intended model for care is now reaching more than 75 percent of membership, including children and their families. Reaching both adults and
children has the potential to increase the program’s impact by supporting families and reducing adverse childhood experiences — transforming and growing healthier future families and communities.
Integrating behavioral health care into primary care clinics
Serving 11,939 Oregonians living in Jackson, Josephine and parts of Douglas counties
“We can help you. There are counselors right
here in the clinic who can see you right now.”

9
Supporting a child with complex health needs can add hardships to families that extend far beyond care efforts and medical costs. Willamette Valley Community Health (WVCH) is breaking down barriers to better health by connecting these families with Family Support Coordinators (FSCs) — advocates who help them communicate with providers and access community resources.
FSCs have the ability to initiate creative interventions by using flexible funds Oregon sets aside for health-related costs insurance won’t cover. They’re also familiar with resources within their communities that can help meet needs that fall outside the realm of medical care, but clearly support better health outcomes.
Take Julie, a five-year-old Salem girl with limited mobility and low muscle tone due to muscular dystrophy. Julie’s primary care provider referred her to an FSC, who learned that while Julie was very independent at school using a special motorized wheelchair, she lacked the same independence and mobility at home — simply because her wheelchair was too heavy to bring inside without a ramp.
Julie’s FSC got approval to use flex funds to install a custom ADA-compliant wheelchair ramp at her home. Julie surprised her health providers by gaining more than two pounds as she waited excitedly for her ramp to be installed. She also gained autonomy and independence that will likely improve her health and reduce future health care costs.
In another case, an FSC advocated for the family of Dante, a boy in Dallas with multiple medical conditions. Dante’s family was in the process of being evicted from their home. Their struggles were compounded by the challenges of caring for a child with a severe medical condition and the stress of the eviction exacerbated Dante’s health problems.
Dante’s FSC turned to the community to help his family find temporary housing and then secure a long-term place to live through Catholic Community Services, cutting through red tape and helping transform what seemed like an impossible challenge into a situation the family could handle. Now, Dante’s family can manage his treatment more consistently,
without the strain of an unstable living situation.
WVCH’s Family Support Team partners with primary care providers from five different clinics in Salem through the Children’s Health Alliance, a Portland-based nonprofit association of private practice pediatricians. These providers help WVCH identify patients with complex health needs who could benefit from program participation. An FSC then works with the family’s entire support system —pediatrician, school staff, specialists and therapists — to help them create a well-defined integrated care plan.
Supporting members with complex health needs beyond the clinic
Serving 102,094 Oregonians living in Marion, Polk and Yamhill counties

9 10
Children who enter Oregon’s foster care system often come with uncertain health histories and fragmented medical records. Providing prompt health assessments for these children helps make sure they receive appropriate physical, mental and dental attention, without long gaps in care.
In fact, Oregon requires that a child’s health be evaluated by a qualified physician within 60 days of entering state custody. But, as necessary as these appointments are, scheduling evaluations with three different providers and transporting children around town can be stressful for foster families, especially those who host more than one child at a time.
Carla McKelvey, M.D., MPH, a Coos Bay pediatrician at North Bend Medical Center, saw firsthand how challenging it was for foster parents to coordinate evaluation appointments. She had a simple but brilliant realization: By bringing a dentist and mental health provider into her office, even just once a week, she could provide families with the opportunity to receive all three assessments at the same time.
The FEARsome Clinic was established. The name is short for Foster Education and Resources and is a nod to the fierce advocacy foster parents display for their foster children, as well as the confidence they gain by receiving the care and support they need from a strong partnership with the local coordinated care organization (CCO), Western Oregon Advanced Health (WOAH).
When families come to the clinic, Dr. McKelvey performs a short health exam and reviews any records provided by The Oregon Department of Human Services. Depending on the child’s age, a counselor from Coos Health & Wellness conducts a developmental, psychological and/or behavioral assessment. Then the dental hygienist completes a simple checkup, looking at teeth and reviewing any available dental notes.
All of a child’s health data is recorded into the clinic’s electronic health record system, and the child is referred to a primary care physician and other providers for ongoing care. The new providers access the health records and coordinate with each other to offer wraparound support.
“It used to take up to six months to do all these appointments,” says long-time foster parent Dolly Daggett. “This is so much better for the kids, as well as the foster parents.”
Establishing children with a primary care provider, dentist or therapist also removes emotional barriers to health care by providing much-needed consistency for kids who come from unstable backgrounds. To these children, a doctor or therapist is one more caring adult they can depend on seeing regularly.
Improving care for foster children with one-stop clinic
Dr. Carla McKelvey examines a young patient.
Serving 20,995 Oregonians living in Coos and Curry counties

The Coalition for a Healthy Oregon (COHO) is an association of organizations that work with coordinated care organizations (CCOs) or provide direct care as CCOs.
Find us on Facebook Visit www.cohoplans.org
Related Documents