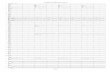
CODE OF STATE REGULATIONS 1 ROBIN CARNAHAN (4/30/09) Secretary of State Rules of Department of Health and Senior Services Division 30—Division of Regulation and Licensure Chapter 86—Residential Care Facilities and Assisted Living Facilities Title Page 19 CSR 30-86.012 Construction Standards for Assisted Living Facilities and Residential Care Facilities....................................................................3 19 CSR 30-86.022 Fire Safety Standards for Residential Care Facilities and Assisted Living Facilities ...............................................................4 19 CSR 30-86.032 Physical Plant Requirements for Residential Care Facilities and Assisted Living Facilities ..............................................................10 19 CSR 30-86.042 Administrative, Personnel and Resident Care Requirements for New and Existing Residential Care Facilities .......................................................12 19 CSR 30-86.043 Administrative, Personnel and Resident Care Requirements for Facilities Licensed as a Residential Care Facility II on August 27, 2006 that Will Comply with Residential Care Facility II Standards .............................19 19 CSR 30-86.045 Standards and Requirements for Assisted Living Facilities Which Provide Services to Residents with a Physical, Cognitive, or Other Impairment that Prevents the Individual from Safely Evacuating the Facility with Minimal Assistance ..........................................................................23 19 CSR 30-86.047 Administrative, Personnel and Resident Care Requirements for Assisted Living Facilities ...................................................................24 19 CSR 30-86.052 Dietary Requirements for Residential Care Facilities and Assisted Living Facilities ...................................................................33

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
CODE OF STATE REGULATIONS 1ROBIN CARNAHAN (4/30/09)Secretary of State
Rules of
Department of Health andSenior Services
Division 30—Division of Regulation and LicensureChapter 86—Residential Care Facilities and
Assisted Living Facilities
Title Page
19 CSR 30-86.012 Construction Standards for Assisted Living Facilities and Residential Care Facilities....................................................................3
19 CSR 30-86.022 Fire Safety Standards for Residential Care Facilitiesand Assisted Living Facilities ...............................................................4
19 CSR 30-86.032 Physical Plant Requirements for Residential Care Facilitiesand Assisted Living Facilities ..............................................................10
19 CSR 30-86.042 Administrative, Personnel and Resident Care Requirements for New andExisting Residential Care Facilities .......................................................12
19 CSR 30-86.043 Administrative, Personnel and Resident Care Requirements for FacilitiesLicensed as a Residential Care Facility II on August 27, 2006 thatWill Comply with Residential Care Facility II Standards .............................19
19 CSR 30-86.045 Standards and Requirements for Assisted Living Facilities Which ProvideServices to Residents with a Physical, Cognitive, or Other Impairmentthat Prevents the Individual from Safely Evacuating the Facility withMinimal Assistance ..........................................................................23
19 CSR 30-86.047 Administrative, Personnel and Resident Care Requirements for Assisted Living Facilities ...................................................................24
19 CSR 30-86.052 Dietary Requirements for Residential Care Facilities andAssisted Living Facilities ...................................................................33
Title 19—DEPARTMENT OFHEALTH AND SENIOR SERVICES
Division 30—Division of Regulationand Licensure
Chapter 86—Residential Care Facilitiesand Assisted Living Facilities
19 CSR 30-86.012 Construction Standardsfor Assisted Living Facilities and Residen-tial Care Facilities
PURPOSE: This rule establishes constructionstandards for Residential Care Facilities andAssisted Living Facilities.
PUBLISHER’S NOTE: The secretary of statehas determined that the publication of theentire text of the material which is incorpo-rated by reference as a portion of this rulewould be unduly cumbersome or expensive.This material as incorporated by reference inthis rule shall be maintained by the agency atits headquarters and shall be made availableto the public for inspection and copying at nomore than the actual cost of reproduction.This note applies only to the reference mate-rial. The entire text of the rule is printedhere.
AGENCY NOTE: All rules relating to long-term care facilities licensed by the depart-ment are followed by a Roman Numeral whichrefers to the class (either class I, II or III) ofstandard as designated in section 198.085.1,RSMo 2000.
(1) These standards apply to assisted livingfacilities and residential care facilities as indi-cated in the rule.
(2) A facility shall submit a copy of plans ofproposed new construction, additions to ormajor remodeling of an existing facility to theSection for Long Term Care of the Depart-ment of Health and Senior Services (here-inafter—the department). If the facility is tobe licensed for more than nine (9) residents,a registered architect or registered profes-sional engineer shall prepare the plans andspecifications for new construction or addi-tions to an existing facility in conformancewith Chapter 327, RSMo. III
(3) Construction of facilities shall begin onlyafter the plans and specifications havereceived the written approval of the depart-ment. Facilities shall then be built in confor-mance with the approved plans and specifica-tions. The facility shall notify the departmentwhen construction begins. If construction ofthe project is not started within one (1) yearafter the date of approval of the plans and
specifications and completed within a periodof three (3) years, the facility shall resubmitplans to the department for its approval andshall amend them, if necessary, to complywith the then current rules before construc-tion work is started or continued. III
(4) If the facility employs more than fifteen(15) people, it shall conform with section 504of the Rehabilitation Act of 1973. Any facili-ty that houses handicapped residents shallhave the first floor rooms and living areasdesigned to be accessible to these residents.III
(5) Facilities shall not house residents on alevel where the outside grade line is morethan three feet (3') above the floor level onthe window side of the room. II
(6) Facilities whose plans were approved afterDecember 31, 1987, shall provide a mini-mum of seventy (70) square feet per residentin private and multiple occupancy bedrooms.This square footage calculation shall includethe floor space used for closets and built-infurniture and equipment if these are for resi-dent use and the closet space does not exceedfive (5) square feet per resident. Private bed-rooms in existing facilities that are requiredto comply with the requirements of 19 CSR30-86.043 or 19 CSR 30-86.047, and multi-ple occupancy bedrooms in facilities licensedbetween November 13, 1980 and December31, 1987, shall have a minimum of sixty (60)square feet of floor space per resident. II
(7) Ceilings in bedrooms shall be a minimumof seven feet (7') in height or if a room withsloping ceiling is used, only the area wherethe ceiling height is at least seven feet (7')can be used to meet the required minimumsquare footage per resident. II
(8) Facilities shall provide bedrooms with atleast one (1) functional outside window withscreen. Window size shall be not less thanone-twentieth (1/20) or five percent (5%) ofthe required floor area. II
(9) Facilities shall provide resident roomswith a full nonlouvered door that swings intothe room. Facilities formerly licensed as res-idential care facilities II and existing prior toNovember 13, 1980, are exempt from thisrequirement. II
(10) Facilities shall permit no more than four(4) beds per bedroom, regardless of the roomsize. Facilities formerly licensed as residen-tial care facilities II and existing prior to
November 13, 1980, are exempt from thisrequirement. II
(11) One (1) tub or shower bath shall be pro-vided for each twenty (20) residents or majorfraction of twenty (20). Facilities exceedingtwenty (20) residents shall have separatebathing facilities for each sex. II
(12) One (1) toilet and lavatory shall be pro-vided for each six (6) residents or major frac-tion of six (6). Facilities formerly licensed asresidential care facilities II and in operationor whose plans were approved prior toNovember 13, 1980 are required to provideone (1) toilet for each ten (10) beds or majorfraction of ten (10) and one (1) lavatory forevery fifteen (15) residents or major fractionof fifteen (15). II
(13) Separate toilet rooms shall be providedfor each sex if common rooms with multi-stalls and stools are provided. II
(14) Bath and toilet facilities shall be conve-niently located so that residents can reachthem without passing through the kitchen,another bedroom, or auxiliary service areas.Facilities formerly licensed as residential carefacilities II and in operation or whose planswere approved prior to November 13, 1980are exempt from this requirement. III
(15) Bath and toilet facilities shall be venti-lated. III
(16) Facilities whose plans were approved orwere initially licensed after December 31,1987, shall have a community living and din-ing area separate from resident bedroomswith at least twenty-five (25) square feet perresident. The community living and diningarea may be combined with footage requiredfor another long-term care facility when thefacility is on the same premises as anotherlicensed facility. Facilities that are required tocomply with the requirements of 19 CSR 30-86.043 licensed prior to November 13, 1980,must have a living room area but they areexempt from minimum size requirements.Facilities licensed between November 13,1980 and December 31, 1987, shall have acommunity living area with twenty (20)square feet per resident for the first twenty(20) residents and an additional fifteen (15)square feet per resident over a census oftwenty (20). II
(17) Facilities shall provide the following inthe dietary area: a kitchen, dishwashing,refrigeration, and garbage disposal facilities.The facility shall arrange the kitchen andequipment to efficiently and sanitarily enable
CODE OF STATE REGULATIONS 3ROBIN CARNAHAN (4/30/09)Secretary of State
Chapter 86—Residential Care Facilities and Assisted Living Facilities 19 CSR 30-86
the storage, preparation, cooking and servingof food and drink to residents. II
(18) Residential care facilities and assistedliving facilities shall provide a designatedattendant’s working area which includes: astorage space for records; locked storagespace for medications; a handwashing sinkwith hot and cold running water, a soap dis-penser and paper towels; and a telephoneconveniently located to the area. Facilitieslicensed for twelve (12) or fewer residents areexempt from a separate working area. III
(19) Facilities shall have a laundry area in aseparate room for storing, sorting, washing,drying and distributing linen and personalclothing. Laundry facilities of a licensedlong-term care facility located on the samepremises may be used. Facilities licensed fortwelve (12) or fewer residents will be exemptfrom having a separate room for laundry butthe laundry room shall be separate from thekitchen and shall not be located in a roomused by residents. III
(20) All newly licensed facilities shall be ofsturdy construction with permanent founda-tions. III
(21) In buildings built prior to September 28,1979, corridors shall have a minimum widthof thirty-six inches (36"). First-floor residentroom doors shall be a minimum of thirty-twoinches (32") wide. Resident room doors ofthese buildings on the second floor and aboveshall be a minimum of thirty inches (30")wide. II/III
(22) In newly licensed buildings constructedon or after September 28, 1979, all residentroom doors shall be a minimum of thirty-twoinches (32") wide on all floors. Corridorsshall be a minimum of forty-eight inches(48") wide and interior stairs shall be at leastthirty-six inches (36") wide. II/III
(23) Exit doors in newly licensed facilitiesshall be at least thirty-six inches (36") wide,at least seventy-two inches (72") high andshall swing outward. II/III
(24) Residential care facilities that acceptdeaf residents, shall have appropriate assis-tive devices to enable each deaf person tonegotiate a path to safety, including, but notlimited to, visual or tactile alarm systems.II/III
(25) Residential care facilities and facilitiesformerly licensed as residential care facilitiesII whose plans were initially approved
between December 31, 1987 and December31, 1998, shall have at least one (1) hydraulicor electric motor-driven elevator if there aremore than twenty (20) residents with bed-rooms above the first floor. The elevatorinstallation(s) shall comply with all local andstate codes, American Society for Mechani-cal Engineers (ASME) A17.1, Safety Codefor Elevators, Dumbwaiters, and Escalators,and the National Fire Protection Associa-tion’s applicable codes. All facilities withplans approved on or after January 1, 1999,shall comply with all local and state codes,ASME A17.1, 1993 Safety Code for Eleva-tors and Escalators, and the 1996 NationalElectrical Code. These references are incor-porated by reference in this rule and availableat: American Society for Mechanical Engi-neers, Three Park Avenue, New York, NY10016-5990; and The American NationalStandards Institute, 11 West 42nd Street, 13thFloor, New York, NY 10036. This rule doesnot incorporate any additional amendmentsor additions. II
(26) Facilities whose plans were approved orwhich were initially licensed after December31, 1987, shall provide an air-conditioningsystem, or individual room air-conditioningunits, capable of maintaining resident-useareas at eighty-five degrees Fahrenheit(85°F) (29.4°C) at the summer design tem-perature. II
(27) Home-Like Requirements with Respectto Construction Standards.
(A) Any assisted living facility formerlylicensed as a residential care facility shall bemore home-like than institutional withrespect to construction and physical plantstandards. II
(B) Any assisted living facility licensed asa residential care facility II prior to August28, 2006, shall qualify as being more home-like than institutional with respect to con-struction and physical plant standards. II
(C) Any assisted living facility that is builtor has plans approved on or after August 28,2006, shall be more home-like than institu-tional with respect to construction and physi-cal plant standards. II
AUTHORITY: sections 198.073 and 198.076,RSMo Supp. 2007.* This rule originally filedas 13 CSR 15-15.012. Original rule filed July13, 1983, effective Oct. 13, 1983. Emergen-cy amendment filed Aug. 1, 1984, effectiveAug. 13, 1984, expired Dec. 10, 1984.Amended: Filed Sept. 12, 1984, effectiveDec. 13, 1984. Amended: Filed May 13,1987, effective Aug. 13, 1987. Amended:Filed Aug. 1, 1988, effective Nov. 10, 1988.
Amended: Filed May 11, 1998, effective Dec.30, 1998. Moved to 19 CSR 30-86.012, effec-tive Aug. 28, 2001. Amended: Filed Nov. 15,2004, effective May 30, 2005. Amended:Filed Aug. 23, 2006, effective April 30, 2007.Amended: Filed March 13, 2008, effectiveOct 30, 2008.
*Original authority: 198.073, RSMo 1979, amended1984, 1992, 1999, 2006, 2007, and 198.076, RSMo 1979,amended 1984, 2007.
19 CSR 30-86.022 Fire Safety Standardsfor Residential Care Facilities and AssistedLiving Facilities
PURPOSE: This rule establishes fire safetystandards for residential care facilities andassisted living facilities.
PUBLISHER’S NOTE: The secretary of statehas determined that the publication of theentire text of the material which is incorpo-rated by reference as a portion of this rulewould be unduly cumbersome or expensive.This material as incorporated by reference inthis rule shall be maintained by the agency atits headquarters and shall be made availableto the public for inspection and copying at nomore than the actual cost of reproduction.This note applies only to the reference mate-rial. The entire text of the rule is printedhere.
Editor’s Note: All rules relating to long-termcare facilities licensed by the department arefollowed by a Roman Numeral notation whichrefers to the class (either class I, II or III) ofstandard as designated in section 198.085.1,RSMo Supp. 1999.
(1) Definitions. For the purpose of this rule,the following definitions shall apply:
(A) Accessible spaces—shall include allrooms, halls, storage areas, basements, attics,lofts, closets, elevator shafts, enclosed stair-ways, dumbwaiter shafts, and chutes.
(B) Area of refuge—a space located in orimmediately adjacent to a path of travel lead-ing to an exit that is protected from theeffects of fire, either by means of separationfrom other spaces in the same building or itslocation, permitting a delay in evacuation.An area of refuge may be temporarily used asa staging area that provides some relativesafety to its occupants while potential emer-gencies are assessed, decisions are made,and, if applicable, evacuation has begun.
(C) Major renovation—shall include thefollowing:
1. Addition of any room(s), accessibleby residents, that either exceeds fifty percent
4 CODE OF STATE REGULATIONS (4/30/09) ROBIN CARNAHAN
Secretary of State
19 CSR 30-86—DEPARTMENT OF HEALTH ANDSENIOR SERVICES Division 30—Division of Regulation and Licensure
(50%) of the total square footage of the facil-ity or exceeds four thousand five hundred(4,500) square feet; or
2. Repairs, remodeling, or renovationsthat involve structural changes to more thanfifty percent (50%) of the building; or
3. Repairs, remodeling, or renovationsthat involve structural changes to more thanfour thousand five hundred (4,500) squarefeet of a smoke section; or
4. If the addition is separated by two (2)-hour fire-resistant construction, only theaddition portion shall meet the requirementsfor NFPA 13, 1999 edition, sprinkler system,unless the facility is otherwise required tomeet NFPA 13, 1999 edition.
(D) Fire-resistant construction—type ofconstruction in residential care and assistedliving facilities in which bearing walls,columns, and floors are of noncombustiblematerial in accordance with NFPA 101, 2000edition. All load-bearing walls, floors, androofs shall have a minimum of a one (1)-hourfire-resistant rating.
(2) General Requirements.(A) All National Fire Protection Associa-
tion (NFPA) codes and standards cited in thisrule: NFPA 10, Standard for Portable FireExtinguishers, 1998 edition; NFPA 13R,Installation of Sprinkler Systems, 1996 edi-tion; NFPA 13, Installation of Sprinkler Sys-tems, 1976 edition; NFPA 13 or NFPA 13R,Standard for the Installation of Sprinkler Sys-tems in Residential Occupancies Up to andIncluding Four Stories in Height, 1999 edi-tion; NFPA 13, Standard for the Installationof Sprinkler Systems, 1999 edition; NFPA 96,Standard for Ventilation Control and FireProtection of Commercial Cooking Opera-tions, 1998 edition; NFPA 101, The LifeSafety Code, 2000 edition; NFPA 72, Nation-al Fire Alarm Code, 1999 edition; NFPA72A, Local Protective Signaling Systems,1975 edition; NFPA 25, Standard for theInspection, Testing, and Maintenance ofWater-Based Fire Protection Systems, 1998edition; and NFPA 101A, Guide to Alterna-tive Approaches to Life Safety, 2001 edition,with regard to the minimum fire safety stan-dards for residential care facilities and assist-ed living facilities are incorporated by refer-ence in this rule and available for purchasefrom the National Fire Protection Agency, 1Batterymarch Park, Quincy, MA 02269-9101; www.nfpa.org; by telephone at (617)770-3000 or 1-800-344-3555. This rule doesnot incorporate any subsequent amendmentsor additions to the materials listed above.This rule does not prohibit facilities fromcomplying with the standards set forth innewer editions of the incorporated by refer-
ence material listed in this subsection of thisrule, if approved by the department.
(B) Facilities that were complying prior tothe effective date of this rule with prior edi-tions of the NFPA provisions referenced inthis rule shall be permitted to continue tocomply with the earlier editions, as long asthere is not an imminent danger to the health,safety, or welfare of any resident or a sub-stantial probability that death or serious phys-ical harm would result as determined by thedepartment.
(C) All facilities shall notify the depart-ment immediately after the emergency isaddressed if there is a fire in the facility orpremises and shall submit a complete writtenfire report to the department within seven (7)days of the fire, regardless of the size of thefire or the loss involved. II/III
(D) The department shall have the right ofinspection of any portion of a building inwhich a licensed facility is located unless theunlicensed portion is separated by two (2)-hour fire-resistant construction. No section ofthe building shall present a fire hazard. I/II
(E) Following the discovery of any fire, thefacility shall monitor the area and/or thesource of the fire for a twenty-four (24)-hourperiod. This monitoring shall include, at aminimum, hourly visual checks of the area.These hourly visual checks shall be docu-mented. I/II
(F) The facility shall maintain the exteriorpremises in a manner as to provide for firesafety. II
(G) Residential care facilities that acceptdeaf residents shall have appropriate assistivedevices to enable each deaf person to negoti-ate a path to safety, including, but not limit-ed to, visual or tactile alarm systems. II/III
(H) Facilities shall not use space understairways to store combustible materials. I/II
(3) Fire Extinguishers.(A) Fire extinguishers shall be provided at
a minimum of one (1) per floor, so that thereis no more than seventy-five feet (75') traveldistance from any point on that floor to anextinguisher. I/II
(B) All new or replacement portable fireextinguishers shall be ABC-rated extinguish-ers, in accordance with the provisions ofNFPA 10, 1998 edition. A K-rated extin-guisher or its equivalent shall be used in lieuof an ABC-rated extinguisher in the kitchencooking areas. II
(C) Fire extinguishers shall have a rating ofat least:
1. Ten pounds (10 lbs.), ABC-rated orthe equivalent, in or within fifteen feet (15')of hazardous areas as defined in 19 CSR 30-83.010; and
2. Five pounds (5 lbs.), ABC-rated orthe equivalent, in other areas. II
(D) All fire extinguishers shall bear thelabel of the Underwriters’ Laboratories (UL)or the Factory Mutual (FM) Laboratories andshall be installed and maintained in accor-dance with NFPA 10, 1998 edition. Thisincludes the documentation and dating of amonthly pressure check. II/III
(4) Range Hood Extinguishing Systems.(A) In facilities licensed on or before July
11, 1980, or in any facility with fewer thantwenty-one (21) beds, the kitchen shall pro-vide either:
1. An approved automatic range hoodextinguishing system properly installed andmaintained in accordance with NFPA 96,1998 edition; or
2. A portable fire extinguisher of at leastten pounds (10 lbs.) ABC-rated, or the equiv-alent, in the kitchen area in accordance withNFPA 10, 1998 edition. II/III
(B) In licensed facilities with a total oftwenty-one (21) or more licensed beds andwhose application was filed after July 11,1980, and prior to October 1, 2000:
1. The kitchen shall be provided with arange hood and an approved automatic rangehood extinguishing system unless the facilityhas an approved sprinkler system. Facilitieswith range hood systems shall continue tomaintain and test these systems; and
2. The extinguishing system shall beinstalled, tested, and maintained in accor-dance with NFPA 96, 1998 edition. II/III
(C) The range hood and its extinguishingsystem shall be certified at least twice annu-ally in accordance with NFPA 96, 1998 edi-tion. II/III
(5) Fire Drills and Evacuation Plans.(A) All facilities shall develop a written
plan for fire drills and other emergencies andevacuation and shall request consultation andassistance annually from a local fire unit. Ifthe consultation cannot be obtained, the facil-ity shall inform the state fire marshal in writ-ing and request assistance in review of theplan. II/III
(B) The plan shall include, but is not lim-ited to, the following:
1. A phased response ranging from relo-cation of residents within the facility to relo-cation to an area of refuge, if applicable, tototal evacuation. This phased response part ofthe plan shall be consistent with the directionof the local fire unit or state fire marshal andappropriate for the fire or emergency;
2. Written instructions for evacuation ofeach floor including evacuation to areas ofrefuge, if applicable, and a floor plan showing
CODE OF STATE REGULATIONS 5ROBIN CARNAHAN (4/30/09)Secretary of State
Chapter 86—Residential Care Facilities and Assisted Living Facilities 19 CSR 30-86
the location of exits, fire alarm pull stations,fire extinguishers, and any areas of refuge;
3. Evacuating residents, if necessary,from an area of refuge to a point of safetyoutside the building;
4. The location of any additional watersources on the property such as cisterns,wells, lagoons, ponds, or creeks;
5. Procedures for the safety and comfortof residents evacuated;
6. Staffing assignments;7. Instructions for staff to call the fire
department or other outside emergency ser-vices;
8. Instructions for staff to call alterna-tive resource(s) for housing residents, if nec-essary;
9. Administrative staff responsibilities;and
10. Designation of a staff member to beresponsible for accounting for all residents’whereabouts. II/III
(C) The written plan shall be accessible atall times and an evacuation diagram shall beposted on each floor in a conspicuous placeso that employees and residents can becomefamiliar with the plan and routes to safety.II/III
(D) A minimum of twelve (12) fire drillsshall be conducted annually with at least one(1) every three (3) months on each shift. Atleast four (4) of the required fire drills mustbe unannounced to residents and staff,excluding staff who are assigned to evaluatestaff and resident response to the fire drill.The fire drills shall include a resident evacu-ation at least once a year. II/III
(E) The facility shall keep a record of allfire drills. The record shall include the time,date, personnel participating, length of timeto complete the fire drill, and a narrativenotation of any special problems. III
(F) The fire alarm shall be activated duringall fire drills unless the drill is conductedbetween 9 p.m. and 6 a.m., when a facility-generated predetermined message is accept-able in lieu of the audible and visual compo-nents of the fire alarm. II/III
(6) Fire Safety Training Requirements.(A) The facility shall ensure that fire safe-
ty training is provided to all employees: 1. During employee orientation; 2. At least every six (6) months; and3. When training needs are identified as
a result of fire drill evaluations. II/III(B) The training shall include, but is not
limited to, the following: 1. Prevention of fire ignition, detection
of fire, and control of fire development; 2. Confinement of the effects of fire;
3. Procedures for moving residents to anarea of refuge, if applicable;
4. Use of alarms;5. Transmission of alarms to the fire
department;6. Response to alarms;7. Isolation of fire;8. Evacuation of immediate area and
building; 9. Preparation of floors and facility for
evacuation; and10. Use of the evacuation plan as
required by section (5) of this rule. II/III
(7) Exits, Stairways, and Fire Escapes.(A) Each floor of a facility shall have at
least two (2) unobstructed exits remote fromeach other. I/II
1. For a facility whose plans wereapproved on or before December 31, 1987,or a facility licensed for twenty (20) or fewerresidents, one (1) of the required exits from amulti-story facility shall be an outside stair-way or an enclosed stairway that is separatedby one (1)-hour rated construction from eachfloor with an exit leading directly to the out-side at grade level. Existing plaster or gyp-sum board of at least one-half inch (1/2")thickness may be considered equivalent toone (1)-hour rated construction. The otherrequired exit may be an interior stairwayleading through corridors or passageways tooutside or to a two (2)-hour rated horizontalexit as defined by paragraph 3.3.61 of the2000 edition NFPA 101. Neither of therequired exits shall lead through a furnace orboiler room. Neither of the required exitsshall be through a resident’s bedroom, unlessthe bedroom door cannot be locked. I/II
2. For a facility whose plans wereapproved after December 31, 1987, for morethan twenty (20) residents, the required exitsshall be doors leading directly outside, one(1)-hour enclosed stairs or outside stairs or atwo (2)-hour rated horizontal exit as definedby paragraph 3.3.61 of 2000 edition NFPA101. The one (1)-hour enclosed stairs shallexit directly outside at grade. Access to theseshall not be through a resident bedroom or ahazardous area. I/II
3. Only one (1) of the required exits maybe a two (2)-hour rated horizontal exit. I/II
(B) In facilities with plans approved afterDecember 31, 1987, doors to resident userooms shall not be more than one hundredfeet (100') from an exit. In facilities equippedwith a complete sprinkler system in accor-dance with NFPA 13 or NFPA 13R, 1999edition, the exit distance may be increased toone hundred fifty feet (150'). Dead-end cor-ridors shall not exceed thirty feet (30') inlength. II
(C) In residential care facilities and facili-ties formerly licensed as residential carefacilities II, floors housing residents whorequire the use of a walker, wheelchair, orother assistive devices or aids, or who areblind, must have two (2) accessible exits tograde or such residents must be housed nearaccessible exits as specified in 19 CSR 30-86.042(33) for residential care facilities and19 CSR 30-86.043(31) for facilities formerlylicensed as residential care facilities II unlessotherwise prohibited by 19 CSR 30-86.045 or19 CSR 30-86.047, facilities equipped witha complete sprinkler system, in accordancewith NFPA 13 or NFPA 13R, 1999 edition,with sprinklered attics, and smoke partitions,as defined by subsection (10)(I) of this rule,may house such residents on floors that donot have accessible exits to grade if eachrequired exit is equipped with an area ofrefuge as defined and described in subsec-tions (1)(B) and (7)(D) of this rule. I/II
(D) An “area of refuge” shall have: 1. An area separated by one (1)-hour
rated smoke walls, from the remainder of thebuilding. This area must have direct accessto the exit stairway or access the stair througha section of the corridor that is separated bysmoke walls from the remainder of the build-ing. This area may include no more than two(2) resident rooms;
2. A two (2)-way communication orintercom system with both visible and audiblesignals between the area of refuge and thebottom landing of the exit stairway, atten-dants’ work area, or other primary locationas designated in the written plan for fire drillsand evacuation;
3. Instructions on the use of the areaduring emergency conditions that are locatedin the area of refuge and conspicuously post-ed adjoining the communication or intercomsystem;
4. A sign at the entrance to the roomthat states “AREA OF REFUGE IN CASEOF FIRE” and displays the internationalsymbol of accessibility;
5. An entry or exit door that is at least aone and three-fourths inch (1 3/4") solid corewood door or has a fire protection rating ofnot less than twenty (20) minutes with smokeseals and positive latching hardware. Thesedoors shall not be lockable;
6. A sign conspicuously posted at thebottom of the exit stairway with a diagramshowing each location of the areas of refuge;
7. Emergency lighting for the area ofrefuge; and
8. The total area of the areas of refugeon a floor shall equal at least twenty (20)square feet for each resident who is blind or
6 CODE OF STATE REGULATIONS (4/30/09) ROBIN CARNAHAN
Secretary of State
19 CSR 30-86—DEPARTMENT OF HEALTH ANDSENIOR SERVICES Division 30—Division of Regulation and Licensure
requires the use of wheelchair or walkerhoused on the floor. II
(E) If it is necessary to lock exit doors, thelocks shall not require the use of a key, tool,special knowledge, or effort to unlock thedoor from inside the building. Only one (1)lock shall be permitted on each door. Delayedegress locks complying with section7.2.1.6.1 of the 2000 edition NFPA 101 shallbe permitted, provided that not more than one(1) such device is located in any egress path.Self-locking exit doors shall be equipped witha hold-open device to permit staff to reenterthe building during the evacuation. I/II
(F) If it is necessary to lock resident roomdoors, the locks shall not require the use of akey, tool, special knowledge, or effort tounlock the door from inside the room. Onlyone (1) lock shall be permitted on each door.Every resident room door shall be designedto allow the door to be opened from the out-side during an emergency when locked. Thefacility shall ensure that facility staff have themeans or mechanisms necessary to open res-ident room doors in case of an emergency.I/II
(G) All stairways and corridors shall beeasily negotiable and shall be maintained freeof obstructions. II
(H) Outside stairways shall be constructedto support residents during evacuation andshall be continuous to the ground level. Out-side stairways shall not be equipped with acounter-balanced device. They shall be pro-tected from or cleared of ice or snow. II/III
(I) Facilities with three (3) or more floorsshall comply with the provisions of Chapter320, RSMo which requires outside stairwaysto be constructed of iron or steel. II
(J) Fire escapes constructed on or afterNovember 13, 1980, whether interior orexterior, shall be thirty-six inches (36") wide,shall have eight-inch (8") maximum risers,nine-inch (9") minimum tread, no winders,maximum height between landings of twelvefeet (12'), minimum dimensions of landingsof forty-four inches (44"), landings at eachexit door, and handrails on both sides and beof sturdy construction, using at least two-inch(2") lumber. Exit doors to these fire escapesshall be at least thirty-six inches (36") wideand the door shall swing outward. II/III
(K) If a ramp is required to meet residents’needs under 19 CSR 30-86.042, the rampshall have a maximum slope of one to twelve(1:12) leading to grade. II/III
(8) Exit Signs.(A) Signs bearing the word EXIT in plain,
legible letters shall be placed at each requiredexit, except at doors directly from rooms toexit passageways or corridors. Letters of all
exit signs shall be at least six inches (6") highand principle strokes three-fourths of an inch(3/4") wide, except that letters of internallyilluminated exit signs shall not be less thanfour inches (4") high. II
(B) Directional indicators showing thedirection of travel shall be placed in corri-dors, passageways, or other locations wherethe direction of travel to reach the nearest exitis not apparent. II/III
(C) All required exit signs and directionalindicators shall be positioned so that bothnormal and emergency lighting illuminatesthem. II/III
(9) Complete Fire Alarm Systems.(A) Facilities that did not have a complete
fire alarm system prior to August 28, 2007,shall have a complete fire alarm systeminstalled in accordance with NFPA 101, Sec-tion 18.3.4, 2000 edition. The complete firealarm shall automatically transmit to the firedepartment, dispatching agency, or centralmonitoring company. The complete firealarm system shall include visual signals andaudible alarms that can be heard throughoutthe building and a main panel that intercon-nects all alarm-activating devices and audiblesignals. At a minimum, the complete firealarm system shall consist of a manual pullstation at or near each attendant’s station andeach required exit in accordance with NFPA72, 1999 edition and the following I/II:
1. For facilities with a sprinkler systemin accordance with NFPA 13, 1999 edition,smoke detectors interconnected to the com-plete fire alarm system shall be installed in allcorridors and spaces open to the corridor.Smoke detectors shall be no more than thirtyfeet (30') apart with no point on the ceilingmore than twenty-one feet (21') from asmoke detector. I/II
2. For facilities with a sprinkler systemin accordance with NFPA 13R, 1999 edition,smoke detectors interconnected to the com-plete fire alarm system shall be installed incorridors, spaces open to the corridor, and inaccessible spaces, as required by NFPA 72,1999 edition, not protected by the sprinklersystem. Smoke detectors shall be no morethan thirty feet (30') apart with no point onthe ceiling more than twenty-one feet (21')from a smoke detector. Smoke detectors shallnot be installed in areas where environmentalinfluences may cause nuisance alarms. Suchareas include, but are not limited to kitchens,laundries, bathrooms, mechanical air han-dling rooms, and attic spaces. In these areas,heat detectors interconnected to the completefire alarm system shall be installed. Bath-rooms not exceeding fifty-five (55) squarefeet and clothes closets, linen closets, and
pantries not exceeding twenty-four (24)square feet are exempt from having anydetection device if the wall and ceilings aresurfaced with limited-combustible or non-combustible material as defined in NFPA101, 2000 edition. Concealed spaces of non-combustible or limited combustible construc-tion are not required to have detectiondevices. These spaces may have limitedaccess but cannot be occupied or used forstorage. I/II
3. For facilities without an approvedsprinkler system, smoke detectors intercon-nected to the complete fire alarm system shallbe installed in all accessible spaces, asrequired by NFPA 72, 1999 edition, withinthe facility. Smoke detectors shall be no morethan thirty feet (30') apart with no point onthe ceiling more than twenty-one feet (21')from a smoke detector. Smoke detectors shallnot be installed in areas where environmentalinfluences may cause nuisance alarms. Suchareas include, but are not limited to kitchens,laundries, bathrooms, mechanical air han-dling rooms, and attic spaces. In these areas,heat detectors interconnected to the fire alarmsystem shall be installed. Bathrooms notexceeding fifty-five (55) square feet andclothes closets, linen closets, and pantries notexceeding twenty-four (24) square feet areexempt from having any detection device ifthe wall and ceilings are surfaced with limit-ed-combustible or noncombustible materialas defined in NFPA 101, 2000 edition. Con-cealed spaces of noncombustible or limitedcombustible construction are not required tohave detection devices. These spaces mayhave limited access but cannot be occupied orused for storage. I/II
(B) Facilities that had a complete firealarm system prior to August 28, 2007, shallhave a complete fire alarm system, in accor-dance with the applicable edition of NFPA72, that at a minimum contains the followingcomponents: interconnected smoke detectorsthroughout the facility, automatic transmis-sion to the fire department, dispatching agen-cy, or central monitoring company, manualpull stations at each required exit and atten-dant’s station, heat detectors, and audible andvisual alarm indicators. I/II
1. Smoke detectors interconnected to thecomplete fire alarm system shall be locatedno more than thirty feet (30') apart in thecorridors or passageways with no point in thecorridor or passageway more than fifteen feet(15') from a detector and no point in thebuilding more than thirty feet (30’) from adetector. In facilities licensed prior toNovember 13, 1980, smoke detectors locatedevery fifty feet (50') will be acceptable. I/II
CODE OF STATE REGULATIONS 7ROBIN CARNAHAN (4/30/09)Secretary of State
Chapter 86—Residential Care Facilities and Assisted Living Facilities 19 CSR 30-86
A. Facilities without an approvedsprinkler system shall have one (1) or moreindividual home-type smoke detectors perresident-use room. The individual home-typesmoke detectors shall be UL-approved bat-tery-powered detectors which sense smokeand automatically sound an alarm which canbe heard throughout the facility. I/II
B. Individual home-type detectorsshall be tested monthly and batteries shall bechanged as needed. Any fault with any detec-tor shall be corrected immediately upon dis-covery. A record shall be kept of the dates oftesting and the changing of batteries. II/III
2. Heat detectors, interconnected to thefire alarm system, shall be installed in areaswhere environmental influences may causenuisance alarms, unless the area is protectedby an approved sprinkler system. Such areasinclude, but are not limited to kitchens, laun-dries, bathrooms, mechanical air handlingrooms, and attic spaces. Bathrooms notexceeding fifty-five (55) square feet areexempt from having a heat detector if the walland ceilings are surfaced with limited-com-bustible or noncombustible material asdefined in NFPA 101, 2000 edition. I/II
(C) All facilities shall test and maintain thecomplete fire alarm system in accordancewith NFPA 72, 1999 edition. I/II
(D) All facilities shall have inspections andwritten certifications of the complete firealarm system completed by an approved qual-ified service representative in accordancewith NFPA 72, 1999 edition, at least annual-ly. I/II
(E) Facilities shall test by activating thecomplete fire alarm system at least once amonth. I/II
(F) Facilities shall maintain a record of thecomplete fire alarm tests, inspections, andcertifications required by subsections (9)(C)and (D) of this rule. III
(G) Upon discovery of a fault with thecomplete fire alarm system, the facility shallpromptly correct the fault. I/II
(H) When a complete fire alarm system isto be out of service for more than four (4)hours in a twenty-four (24)-hour period, thefacility shall immediately notify the depart-ment and the local fire authority and imple-ment an approved fire watch in accordancewith NFPA 101, 2000 edition, until the com-plete fire alarm system has returned to fullservice. I/II
(I) The complete fire alarm system shall beactivated by all of the following: sprinklersystem flow alarm, smoke detectors, heatdetectors, manual pull stations, and activationof the rangehood extinguishment system.II/III
(10) Protection from Hazards.(A) In assisted living facilities and residen-
tial care facilities licensed on or after Novem-ber 13, 1980, for more than twelve (12) res-idents, hazardous areas shall be separated byconstruction of at least a one (1)-hour fire-resistant rating. In facilities equipped with acomplete fire alarm system, the one (1)-hourfire separation is required only for furnace orboiler rooms. Hazardous areas equipped witha complete sprinkler system are not requiredto have this one (1)-hour fire separation.Doors to hazardous areas shall be self-closingand shall be kept closed unless an electro-magnetic hold-open device is used which isinterconnected with the fire alarm system.When the sprinkler option is chosen, theareas shall be separated from other spaces bysmoke-resistant partitions and doors. Thedoors shall be self-closing or automatic-clos-ing. Facilities formerly licensed as residentialcare facility I or II, and existing prior toNovember 13, 1980, shall be exempt fromthis requirement. II
(B) The storage of unnecessary com-bustible materials in any part of a building inwhich a licensed facility is located is prohib-ited. I/II
(C) Electric or gas clothes dryers shall bevented to the outside. Lint traps shall becleaned regularly to protect against fire haz-ard. II/III
(D) In facilities that are required to complywith the requirements of 19 CSR 30-86.043and were formerly licensed as residential carefacilities II on or after November 13, 1980,each floor shall be separated by constructionof at least a one (1)-hour fire resistant rating.Buildings equipped with a complete sprinklersystem may have a nonrated smoke separationbarrier between floors. Doors between floorsshall be a minimum of one and three-fourthsinches (1 3/4") thick and be solid core wooddoors or metal doors with an equivalent firerating. II
(E) In facilities licensed prior to November13, 1980, and multi-storied residential carefacilities formerly licensed as residential carefacilities I licensed on or after November 13,1980, there shall be a smoke separation bar-rier between the floors of resident-use areasand any floor below the resident-use area.This shall consist of a solid core wood dooror metal door with an equivalent fire rating atthe top or the bottom of the stairs. There shallnot be a transom above the door that wouldpermit the passage of smoke. II
(F) Atriums open between floors will bepermitted if resident room corridors are sep-arated from the atrium by one (1)-hour ratedsmoke walls. These corridors must haveaccess to at least one (1) of the required exits
without traversing any space opened to theatrium. II
(G) All doors providing separation betweenfloors shall have a self-closing deviceattached. If the doors are to be held open,electromagnetic hold-open devices shall beused that are interconnected with either anindividual smoke detector or a complete firealarm system. II
(H) All facilities shall be divided into atleast two (2) smoke sections with each sec-tion not exceeding one hundred fifty feet(150') in length or width. If the floor’sdimensions do not exceed seventy-five feet(75') in length or width, a division of thefloor into two (2) smoke sections will not berequired. II
(I) In facilities whose plans were approvedor which were initially licensed after Decem-ber 31, 1987, for more than twenty (20) res-idents and all facilities licensed after August28, 2007, each smoke section shall be sepa-rated by one (1)-hour fire rated smoke parti-tions. The smoke partitions shall be continu-ous from outside wall-to-outside wall andfrom floor-to-floor or floor-to-roof deck. Alldoors in this wall shall be at least twenty(20)-minute fire-rated or its equivalent, self-closing, and may be held open only if thedoor closes automatically upon activation ofthe complete fire alarm system. II
(J) In all facilities that were initiallylicensed on or prior to December 31, 1987and all facilities licensed for twenty (20) orfewer beds prior to August 28, 2007, eachsmoke section shall be separated by a one (1)-hour fire-rated smoke partition that extendsfrom the inside portion of an exterior wall tothe inside portion of an exterior wall andfrom the floor to the underside of the floor orroof deck above, through any concealedspaces, such as those above suspended ceil-ings, and through interstitial structural andmechanical spaces. Smoke partitions shall bepermitted to terminate at the underside of amonolithic or suspending ceiling systemwhere the following conditions are met: Theceiling system forms a continuous membrane,a smoketight joint is provided between the topof the smoke partition and the bottom of thesuspended ceiling and the space above theceiling is not used as a plenum. Smoke parti-tion doors shall be at least twenty (20)-minutefire-rated or its equivalent, self-closing, andmay be held open only if the door closesautomatically upon activation of the completefire alarm system. II
(K) Facilities whose plans were approvedor which were initially licensed after Decem-ber 31, 1987, for more than twenty (20) res-idents and which are unsprinklered shall haveone (1)-hour rated corridor walls with one
8 CODE OF STATE REGULATIONS (4/30/09) ROBIN CARNAHAN
Secretary of State
19 CSR 30-86—DEPARTMENT OF HEALTH ANDSENIOR SERVICES Division 30—Division of Regulation and Licensure
and three-quarters inch (1 3/4") solid corewood doors or metal doors with an equivalentfire rating. II
(L) If two (2) or more levels of long-termcare or two (2) different businesses are locat-ed in the same building, the entire buildingshall meet either the most strict constructionand fire safety standards for the combinedfacility or the facilities shall be separatedfrom the other(s) by two (2)-hour fire-resis-tant construction. In buildings equipped witha complete sprinkler system in accordancewith NFPA 13 or NFPA 13R, 1999 edition,this separation may be rated at one (1) hour.II
(11) Sprinkler Systems.(A) Facilities licensed on or after August
28, 2007, or any facility performing majorrenovations to the facility shall have a com-plete sprinkler system installed in accordancewith NFPA 13, 1999 edition. I/II
(B) Facilities that have sprinkler systemsinstalled prior to August 28, 2007, shalloperate, maintain, and test these systems inaccordance with NFPA 13, 1999 edition, orNFPA 13R, 1999 edition, and NFPA 25,1998 edition. I/II
(C) All residential care facilities, andassisted living facilities that do not admit orretain a resident with a physical, cognitive, orother impairment that prevents the individualfrom safely evacuating the facility with mini-mal assistance, that were licensed prior toAugust 28, 2007, with more than twenty (20)residents, and do not have an approved sprin-kler system in accordance with NFPA 13,1999 edition, or NFPA 13R, 1999 edition,shall have until December 31, 2012, to installan approved sprinkler system in accordancewith NFPA 13 or 13R, 1999 edition. I/II Thedepartment shall grant exceptions to thisrequirement if the facility meets Chapter 33of NFPA 101, 2000 edition, and the evacua-tion capability of the facility meets the stan-dards required in NFPA 101A, Guide toAlternative Approaches to Life Safety, 2001edition. I/II
(D) Single-story assisted living facilitiesthat provide care to one (1) or more residentswith a physical, cognitive, or other impair-ment that prevents the individual from safelyevacuating the facility with minimal assis-tance shall install and maintain an approvedsprinkler system in accordance with NFPA13R, 1999 edition. I/II
(E) Multi-level assisted living facilities thatprovide care to one (1) or more residents witha physical, cognitive, or other impairmentthat prevents the individual from safely evac-uating the facility with minimal assistanceshall install and maintain an approved sprin-
kler system in accordance with NFPA 13,1999 edition. I/II
(F) All facilities shall have inspections andwritten certifications of the approved sprin-kler system completed by an approved quali-fied service representative in accordance withNFPA 25, 1998 edition. The inspections shallbe in accordance with the provisions of NFPA25, 1998 edition, with certification at leastannually by a qualified service representative.I/II
(G) When a sprinkler system is to be out-of-service for more than four (4) hours in atwenty-four (24)-hour period, the facilityshall immediately notify the department andimplement an approved fire watch in accor-dance with NFPA 101, 2000 edition, until thesprinkler system has been returned to full ser-vice. I/II
(12) All facilities shall submit, by July 1,2008, a plan for compliance to the state firemarshal showing how the facility meets therequirements of sections (9) and (11) andsubsections (10)(H) and (10)(I) of this rule.If the facility’s plan for compliance does notmeet the requirements of sections (9) and(11) and subsections (10)(H) and (10)(I) ofthis rule, the facility shall provide the statefire marshal with a written plan to include ata minimum an explanation of how therequirements of sections (9) and (11) andsubsections (10)(H) and (10)(I) will be met,when they will be met, and contact informa-tion in the event the plan does not evidencecompliance with these requirements. II
(A) To qualify for a sprinkler systemexception, the facility shall present evidenceto the state fire marshal in writing that thefacility meets the safety requirements ofChapter 33 of existing residential board andcare occupancies of NFPA 101 Life SafetyCode. II
(13) Emergency Lighting.(A) Emergency lighting of sufficient inten-
sity shall be provided for exits, stairs, resi-dent corridors, and attendants’ station. II
(B) The lighting shall be supplied by anemergency service, an automatic emergencygenerator, or battery operated lighting sys-tem. This emergency lighting system shall beequipped with an automatic transfer switch.II
(C) If battery powered lights are used, theyshall be capable of operating the light for atleast one and one-half (1 1/2) hours. II
(14) Interior Finish and Furnishings.(A) In a facility licensed on or after
November 13, 1980, for more than twelve(12) residents, wall and ceiling surfaces of all
occupied rooms and all exitways shall be clas-sified either Class A or B interior finish asdefined in NFPA 101, 2000 edition. II
(B) In facilities licensed prior to November13, 1980, all wall and ceiling surfaces shallbe smooth and free of highly combustiblematerials. II
(C) In a facility licensed on or afterNovember 13, 1980, for more than twelve(12) residents, the new or replacement floorcovering and carpeting shall be Class I interi-or floor finish in nonsprinklered buildingsand Class II interior floor finish in sprin-klered buildings as defined in NFPA 101,2000 edition. II/III
(D) All new or replacement curtains anddrapes in a licensed facility shall be certifiedor treated to be flame-resistant as defined inNFPA 101, 2000 edition. II
(15) Smoking.(A) Smoking shall be permitted in desig-
nated areas only. Areas where smoking ispermitted shall be designated as such andshall be supervised either directly or by a res-ident informing an employee of the facilitythat the area is being used for smoking. II/III
(B) Ashtrays shall be made of noncom-bustible material and safe design and shall beprovided in all areas where smoking is per-mitted. II/III
(C) The contents of ashtrays shall be dis-posed of properly in receptacles made of non-combustible material. II/III
(16) Trash and Rubbish Disposal.(A) Only metal or UL- or FM-fire-resis-
tant rated wastebaskets shall be used fortrash. II
(B) Trash shall be removed from thepremises as often as necessary to prevent firehazards and public health nuisance. II
(C) No trash shall be burned within fiftyfeet (50') of any facility except in an approvedincinerator. I/II
(D) Trash may be burned only in a mason-ry or metal container. II
(E) The container shall be equipped with ametal cover with openings no larger than one-half inch (1/2") in size. III
(17) Standards for Designated SeparatedAreas.
(A) When a resident resides among theentire general population of the facility, thefacility shall take necessary measures to pro-vide such residents with the opportunity toexplore the facility and, if appropriate, itsgrounds. When a resident resides within adesignated, separated area that is secured bylimited access, the facility shall take neces-sary measures to provide such residents with
CODE OF STATE REGULATIONS 9ROBIN CARNAHAN (4/30/09)Secretary of State
Chapter 86—Residential Care Facilities and Assisted Living Facilities 19 CSR 30-86
the opportunity to explore the separated areaand, if appropriate, its grounds. If enclosedor fenced courtyards are provided, residentsshall have reasonable access to such court-yards. Enclosed or fenced courtyards that areaccessible through a required exit door shallbe large enough to provide an area of refugefor fire safety at least thirty feet (30') fromthe building. Enclosed or fenced courtyardsthat are accessible through a door other thana required exit shall have no size require-ments. II
(B) The facility shall provide freedom ofmovement for the residents to common areasand to their personal spaces. The facility shallnot lock residents out of or inside theirrooms. I/II
(C) The facility may allow resident roomdoors to be locked providing the residentsrequest to lock their doors. Any lock on aresident room door shall not require the useof a key, tool, special knowledge, or effort tolock or unlock the door from inside the resi-dent’s room. Only one (1) lock shall be per-mitted on each door. The facility shall ensurethat facility staff has the means or mecha-nisms necessary to open resident room doorsin case of an emergency. I/II
(D) The facility may provide a designated,separated area where residents, who are men-tally incapable of negotiating a pathway tosafety, reside and receive services and whichis secured by limited access if the followingconditions are met:
1. Dining rooms, living rooms, activityrooms, and other such common areas shall beprovided within the designated, separatedarea. The total area for common areas withinthe designated, separated area shall be equalto at least forty (40) square feet per resident;II/III
2. Doors separating the designated, sep-arated area from the remainder of the facilityor building shall not be equipped with locksthat require a key to open; I/II
3. If locking devices are used on exitdoors egressing the facility or on doorsaccessing the designated, separated area,delayed egress magnetic locks shall be used.These delayed egress devices shall complywith the following:
A. The lock must unlock when thefire alarm is activated;
B. The lock must unlock when thepower fails;
C. The lock must unlock within thir-ty (30) seconds after the release device hasbeen pushed for at least three (3) seconds,and an alarm must sound adjacent to thedoor;
D. The lock must be manually resetand cannot automatically reset; and
E. A sign shall be posted on the doorthat reads: PUSH UNTIL ALARMSOUNDS, DOOR CAN BE OPENED IN 30SECONDS. I/II
4. The delayed egress magnetic locksmay also be released by a key pad locatedadjacent to the door for routine use by staff.I/II
AUTHORITY: sections 198.073, 198.074,and 198.076, RSMo Supp. 2008.* This ruleoriginally filed as 13 CSR 15-15.022. Origi-nal rule filed July 13, 1983, effective Oct. 13,1983. Emergency amendment filed Aug. 1,1984, effective Aug. 13, 1984, expired Dec.10, 1984. Amended: Filed Sept. 12, 1984,effective Dec. 13, 1984. Amended: Filed May13, 1987, effective Aug. 13, 1987. Amended:Filed Aug. 1, 1988, effective Nov. 10, 1988.Amended: Filed Feb. 28, 2000, effective Sept.30, 2000. Moved to 19 CSR 30-86.022, effec-tive Aug. 28, 2001. Amended: Filed Aug. 16,2004, effective Feb. 28, 2005. Amended:Filed Aug. 1, 2005, effective Jan. 30, 2006.Amended: Filed Aug. 23, 2006, effectiveApril 30, 2007. Emergency amendment filedNov. 24, 2008, effective Dec. 4, 2008,expired June 1, 2009. Amended: Filed Nov.24, 2008, effective May 30, 2009.
*Original authority: 198.073, RSMo 1979, amended1984, 1992, 1999, 2006; 198.074, RSMo 2007; and198.076, RSMo 1979, amended 1984, 2007.
19 CSR 30-86.032 Physical Plant Require-ments for Residential Care Facilities andAssisted Living Facilities
PURPOSE: This rule establishes standardsfor the physical plant of new or existing resi-dential care facilities I and II.
PUBLISHER’S NOTE: The secretary of statehas determined that the publication of theentire text of the material which is incorpo-rated by reference as a portion of this rulewould be unduly cumbersome or expensive.This material as incorporated by reference inthis rule shall be maintained by the agency atits headquarters and shall be made availableto the public for inspection and copying at nomore than the actual cost of reproduction.This note applies only to the reference mate-rial. The entire text of the rule is printedhere.
Editor’s Note: All rules relating to long-termcare facilities licensed by the department arefollowed by a Roman Numeral notation whichrefers to the class (either class I, II or III) ofstandard as designated in section 198.085.1,RSMo 2000.
(1) Definitions. For the purpose of this rule,the following definitions shall apply:
(A) Adult day health care program shallmean a program operated by a provider certi-fied to provide Medicaid-reimbursed adultday health care services to Medicaid-eligibleparticipants in accordance with 19 CSR 70-92.010;
(B) Associated adult day health care pro-gram shall mean an adult day health care pro-gram, which is connected physically with alicensed long-term care facility but has sepa-rate designated space for an adult day healthcare program which is above the licensedspace requirement for the long-term care res-idents. An associated adult day health careprogram may share, in part, staff, equipment,utilities, dietary and security with the con-nected long-term care facility. Recipients ofadult day health care program may participatewith the residents of the long-term care facil-ity for some activities and programs;
(C) Home-like—means a self-containedlong-term care setting that integrates the psy-chosocial, organizational and environmentalqualities that are associated with being athome. Home-like may include, but is not lim-ited to the following:
1. A living room and common use areasfor social interactions and activities;
2. Kitchen and family style eating areafor use by the residents;
3. Laundry area for use by residents;4. A toilet room that contains a toilet,
lavatory and bathing unit in each resident’sroom;
5. Resident room preferences for resi-dents who wish to share a room, and for res-idents who wish to have private bedrooms;
6. Outdoor area for outdoor activitiesand recreation; and
7. A place where residents can give andreceive affection, explore their interests,exercise control over their environment,engage in interactions with others and haveprivacy, security, familiarity and a sense ofbelonging; and
(D) Non-licensed adult day care programshall mean a group program designated toprovide care and supervision to meet theneeds of four (4) or fewer impaired adults forperiods of less than twenty-four (24) hoursbut more than two (2) hours per day in along-term care facility.
(2) The building shall be substantially con-structed and shall be maintained in goodrepair and in accordance with the construc-tion and fire safety rules in effect at the timeof initial licensing. II/III
10 CODE OF STATE REGULATIONS (4/30/09) ROBIN CARNAHAN
Secretary of State
19 CSR 30-86—DEPARTMENT OF HEALTH ANDSENIOR SERVICES Division 30—Division of Regulation and Licensure
CODE OF STATE REGULATIONS 11ROBIN CARNAHAN (4/30/09)Secretary of State
Chapter 86—Residential Care Facilities and Assisted Living Facilities 19 CSR 30-86
(3) Only activities necessary to the adminis-tration of the facility shall be contained in anybuilding used as a long-term care facilityexcept as follows:
(A) Related activities may be conducted inbuildings subject to prior written approval ofthese activities by the Department of Healthand Senior Services (hereinafter—the depart-ment). Examples of these activities are HomeHealth Agencies, physician’s office, pharma-cy, ambulance service, child day care andfood service for the elderly in the communi-ty;
(B) Adult day care may be provided forfour (4) or fewer participants without priorwritten approval of the department if thelong-term care facility meets the followingstipulations:
1. The operation of the adult day carebusiness shall not interfere with the care anddelivery of services to the long-term care res-idents;
2. The facility shall only accept partici-pants in the adult day care program appropri-ate to the level of care of the facility andwhose needs can be met;
3. The facility shall not change the phys-ical layout of the facility without prior writtenapproval of the department;
4. The facility shall provide a privatearea for adult day care residents to nap orrest;
5. Adult day care participants shall notbe included in the census, and the number ofadult day care participants shall not be morethan four (4) above the licensed capacity ofthe facility; and
6. The adult day care participants, whileon-site, are to be included in the determina-tion of staffing patterns for the long-term carefacility;
(C) An associated adult day health careprogram may be operated without prior writ-ten approval if the provider of the adult dayhealth care services is certified in accordancewith 19 CSR 70-92.010. II/III
(4) All stairways shall be equipped with per-manently secured handrails on at least one (1)side. III
(5) There shall be a telephone in the facilityand additional telephones or extensions asnecessary so that help may be summonedpromptly in case of fire, accident, acute ill-ness or other emergency. II/III
(6) Bath and toilet facilities shall be providedfor the convenience, privacy, comfort andsafety of residents. Fixed partitions or cur-tains shall be provided in toilet and bath-rooms to assure privacy. II/III
(7) Newly licensed facilities shall havehandrails and grab bars affixed in all toiletand bathing areas. Existing licensed facilitiesshall have handrails and grab bars available inat least one (1) bath and toilet area. The fore-going requirements are applicable to residen-tial care facilities. All assisted living facilitiesshall have handrails and grab bars affixed inall toilet and bathing areas. II
(8) There shall be adequate storage areas forfood, supplies, linen, equipment and resi-dent’s personal possessions. III
(9) Each room or ward in which residents arehoused or to which residents have reasonableaccess shall be capable of being heated to notless than eighty degrees Fahrenheit (80°F)under all weather conditions. Temperatureshall not be lower than sixty-eight degreesFahrenheit (68°F) and the reasonable comfortneeds of individual residents shall be met.I/II
(10) In newly licensed facilities or if a newheating system is installed in an existinglicensed facility, the heating of the buildingshall be restricted to steam, hot water, per-manently installed electric heating devices ora warm air system employing central heatingplants with installation such as to safeguardthe inherent fire hazard, or approved installa-tion of outside wall heaters which bear theapproved label of the American Gas Associa-tion or National Board of Fire Underwriters.The foregoing requirements are applicable toresidential care facilities. In assisted livingfacilities, the heating of the building shall berestricted to steam, hot water, permanentlyinstalled electric heating devices or a warmair system employing central heating plantswith installation such as to safeguard theinherent fire hazard, or approved installationof outside wall heaters which bear theapproved label of the American Gas Associa-tion or National Board of Fire Underwriters.For all facilities, oil or gas heating appliancesshall be properly vented to the outside andthe use of portable heaters of any kind is pro-hibited. If approved wall heaters are used,adequate guards shall be provided to safe-guard residents. I/II
(11) Wood-burning stoves shall not beinstalled in newly licensed facilities or inexisting licensed facilities that did not previ-ously have a wood-burning stove. If wood-burning stoves are used in an existinglicensed facility, or wood-burning furnaces orfireplaces are used, flues or chimneys shallbe maintained in good condition and kept freeof accumulation of combustible materials.The foregoing requirements are applicable toresidential care facilities. Wood-burning
stoves shall not be installed in assisted livingfacilities. II
(12) Fireplaces may be used only if there is aprotective screen in place; if there is directstaff supervision of residents while in use;and the fire shall not be left burningovernight. II
(13) In facilities that are constructed or haveplans approved after July 1, 2005, electricalwiring shall be installed and maintained inaccordance with the requirements of theNational Electrical Code, 1999 edition,National Fire Protection Association, Inc.,incorporated by reference, in this rule andavailable by mail at One Batterymarch Park,Quincy, MA 02269, and local codes. Thisrule does not incorporate any subsequentamendments or additions to the materialsincorporated by reference. Facilities builtbetween September 28, 1979 and July 1,2005 shall be maintained in accordance withthe requirements of the National ElectricalCode, which was in effect at the time of theoriginal plan approval and local codes. Thisrule does not incorporate any subsequentamendments or additions. In facilities builtprior to September 28, 1979, electricalwiring shall be maintained in good repair andshall not present a safety hazard. All facili-ties shall have wiring inspected every two (2)years by a qualified electrician. II/III
(14) Lighting is restricted to electricity. II
(15) Lighting in hallways, bathrooms, recre-ational and dining areas and all resident-useareas shall be provided with a minimumintensity of ten (10) footcandles. All lights inresident-use areas shall be provided with ashade to prevent direct glare to the residents’eyes. II/III
(16) Night lights shall be provided for corri-dors, stairways and toilet areas. II
(17) A reading light shall be provided foreach resident desiring to read. Additionallighting shall be provided to meet the indi-vidual needs of each resident. III
(18) If extension cords are used, they must beUnderwriters’ Laboratory (UL)-approved orshall comply with other recognized electricalappliance approval standards and sized tocarry the current required for the applianceused. Only one (1) appliance shall be con-nected to one (1) extension cord and only two(2) appliances may be served by one (1)duplex receptacle. If extension cords areused, they shall not be placed under rugs,through doorways or located where they aresubject to physical damage. II/III
(19) If elevators are used, installation andmaintenance shall comply with local andstate codes and the National Electric Code.II/III
(20) Air conditioning, fans or a ventilatingsystem shall be available and used when theroom temperature exceeds eighty-fivedegrees Fahrenheit (85°F) and the reasonablecomfort needs of individual residents shall bemet. I/II
(21) Gas-fired water heaters shall be proper-ly installed and vented and all water heatersshall be equipped with a temperature andpressure relief valve. II
(22) Furniture and equipment shall be main-tained in good condition and shall be replacedif broken, torn, heavily soiled or damaged.Rooms shall be so designed and furnishedthat the comfort and safety of the residentsare provided for at all times. II/III
(23) Rooms shall be neat, orderly andcleaned daily. II/III
(24) An individual bed, in good repair and ofa rigid type, shall be provided to each resi-dent. Beds shall be at least thirty-six inches(36") wide. Double beds of satisfactory con-struction may be provided for married cou-ples. Rollaway, metal cots or folding bedsshall not be used. II/III
(25) A minimum of three feet (3') shall beavailable between beds when parallel. III
(26) Mattresses shall be clean, in good repairand a minimum of four inches (4") in thick-ness to provide comfort. II/III
(27) Each bed shall be provided with at leastone (1) clean, comfortable pillow. Extra pil-lows shall be available to meet the needs ofthe residents. III
(28) Screens or curtains, either portable orpermanently affixed, shall be available andused in multi-resident bedrooms to provideprivacy as needed or if requested. III
(29) Each resident shall be provided with anindividual locker or other suitable space forstorage of clothing and personal belongings.III
(30) Each resident shall be provided with anindividual rack for a towel(s) and wash-cloth(s) unless provided with a clean wash-cloth(s) or towel(s) for use each time needed.III
(31) A comfortable chair shall be availablefor each resident’s use. III
(32) Each window shall be provided with ashade, drape or curtain to restrict the amountof sunlight when necessary. III
(33) All assisted living facilities and all resi-dential care facilities whose plans areapproved or which are initially licensed formore than twelve (12) residents after Decem-ber 31, 1987 shall be equipped with a callsystem consisting of an electrical intercom-munication system, a wireless pager system,buzzer system or hand bells. An acceptablemechanism for calling attendants shall belocated in each toilet room and resident bed-room. Call systems for facilities whose plansare approved or which are initially licensedafter December 31, 1987 shall be audible inthe attendant’s work area. II/III
(34) Plumbing fixtures which are accessibleto residents and which supply hot water shallbe thermostatically controlled so that thewater temperature at the fixture does notexceed one hundred twenty degrees Fahren-heit (120°F) (49°C) and the water shall be ata temperature range between one hundredfive degrees Fahrenheit (105°F) (41°C) andone hundred twenty degrees Fahrenheit(120°F) (49°C). I/II
(35) Home-Like Requirements with Respectto Construction and Physical Plant Standards.
(A) Any assisted living facility formerlylicensed as a residential care facility shall bemore home-like than institutional withrespect to construction and physical plantstandards. II
(B) Any assisted living facility licensed asa residential care facility II prior to August28, 2006, shall qualify as being more home-like than institutional with respect to con-struction and physical plant standards. II
(C) Any assisted living facility that is builtor has plans approved on or after August 28,2006, shall be more home-like than institu-tional with respect to construction and physi-cal plant standards. II
AUTHORITY: sections 198.076, RSMo 2000and 198.005 and 198.073, RSMo Supp.2006.* This rule originally filed as 13 CSR15-15.032. Original rule filed July 13, 1983,effective Oct. 13, 1983. Emergency amend-ment filed Nov. 9, 1983, effective Nov. 19,1983, expired March 18, 1984. Amended:Filed Nov. 9, 1983, effective Feb. 11, 1984.Emergency amendment filed Aug. 1, 1984,effective Aug. 13, 1984, expired Dec. 10,1984. Amended: Filed Sept. 12, 1984, effec-tive Dec. 13, 1984. Amended: Filed May 13,
1987, effective Aug. 13, 1987. Amended:Filed Aug. 1, 1988, effective Nov. 10, 1988.Moved to 19 CSR 30-86.032, effective Aug.28, 2001. Amended: Filed Nov. 15, 2004,effective May 30, 2005. Amended: Filed Aug.23, 2006, effective April 30, 2007.
*Original authority: 198.005, RSMo 2006; 198.073,RSMo 1979, amended 1984, 1992, 1999, 2006; and198.076, RSMo 1979, amended 1984.
19 CSR 30-86.042 Administrative, Person-nel and Resident Care Requirements forNew and Existing Residential Care Facili-ties
PURPOSE: This rule establishes standardsfor administration, personnel and residentcare in residential care facilities I and II.
Editor’s Note: All rules relating to long-termcare facilities licensed by the department arefollowed by a Roman Numeral notation whichrefers to the class (either class I, II or III) ofstandard as designated in section 198.085.1,RSMo 1986.
(1) Definitions. For the purpose of this rule,the following definitions shall apply:
(A) Department—Department of Healthand Senior Services;
(B) Outbreak—an occurrence in a commu-nity or region of an illness(es) similar innature, clearly in excess of normal expectan-cy and derived from a common or a propa-gated source; and
(C) Evacuate the facility—moving to anarea of refuge or from one (1) smoke sectionto another or exiting the facility.
(2) For a residential care facility, a personshall be designated as administrator/managerwho is either currently licensed as a nursinghome administrator or is at least twenty-one(21) years of age, has never been convicted ofan offense involving the operation of a long-term care or similar facility and who attendsat least one (1) continuing education work-shop within each calendar year given by orapproved by the department. When used inthis chapter of rules, the term manager shallmean that person who is designated by theoperator to be in general administrativecharge of a residential care facility. It shall beconsidered synonymous to “administrator” asdefined in section 198.006, RSMo and theterms administrator and manager may beused interchangeably. II/III
(3) The administrator/manager of a residen-tial care facility shall have successfully com-pleted the state approved Level I Medication
12 CODE OF STATE REGULATIONS (4/30/09) ROBIN CARNAHAN
Secretary of State
19 CSR 30-86—DEPARTMENT OF HEALTH ANDSENIOR SERVICES Division 30—Division of Regulation and Licensure
Aide course unless he or she is a physician,pharmacist, licensed nurse or a certifiedmedication technician, or if the facility isoperating in conjunction with a skilled nurs-ing facility or intermediate care facility on thesame premises, or, for an assisted living facil-ity, if the facility employs on a full-time basis,a licensed nurse who is available seven (7)days per week. II/III
(4) The operator shall be responsible toassure compliance with all applicable lawsand regulations. The administrator/managershall be fully authorized and empowered tomake decisions regarding the operation of thefacility and shall be held responsible for theactions of all employees. The administra-tor/manager’s responsibilities shall includeoversight of residents to assure that theyreceive care appropriate to their needs. II/III
(5) The administrator/manager shall devotesufficient time and attention to the manage-ment of the facility as is necessary for thehealth, safety and welfare of the residents. II
(6) The administrator/manager shall desig-nate, in writing, a staff member in charge inthe administrator/manager’s absence. II/III
(7) The facility shall not care for more resi-dents than the number for which the facilityis licensed. If the facility operates a non-licensed adult day care program within thelicensed facility, the day care participantsshall be counted in the staffing determinationduring the hours the day care participants arein the facility. II/III
(8) The facility’s current license shall beposted in a conspicuous place and noticesprovided to the facility by the departmentgranting exception(s) to regulatory require-ments shall be posted alongside of the facili-ty’s license. III
(9) All personnel responsible for residentcare shall have access to the legal name ofeach resident, name and telephone number ofresident’s physician, resident’s designee orlegally authorized representative in the eventof emergency. II/III
(10) All persons who have any contact withthe residents in the facility shall not know-ingly act or omit any duty in a manner whichwould materially and adversely affect thehealth, safety, welfare or property of resi-dents. No person who is listed on theEmployee Disqualification List (EDL) main-tained by the department as required by sec-tion 198.070, RSMo shall work or volunteer
in the facility in any capacity whether or notemployed by the operator. For the purpose ofthis rule, a volunteer is an unpaid individualformally recognized by the facility as provid-ing a direct care service to residents. Thefacility is required to check the EDL for indi-viduals who volunteer to perform a servicefor which the facility might otherwise have tohire an employee. The facility is not requiredto check the EDL for individuals or groupssuch as scout groups, bingo or sing-alongleaders. The facility is not required to checkthe EDL for an individual such as a priest,minister or rabbi visiting a resident who is amember of the individual’s congregation.However, if the minister, priest or rabbiserves as a volunteer facility chaplain, thefacility is required to check the EDL sincethe individual would have potential contactwith all residents. I/II
(11) Prior to allowing any person who hasbeen hired in a full-time, part-time or tempo-rary position to have contact with any resi-dents the facility shall, or in the case of tem-porary employees hired through or contractedfor an employment agency, the employmentagency shall prior to sending a temporaryemployee to a provider:
(A) Request a criminal background checkfor the person, as provided in section 43.540,RSMo. Each facility must maintain in itsrecord documents verification that the back-ground checks were requested and the natureof the response received for each suchrequest. II
1. The facility must ensure that anyapplicant or person hired or retained who dis-closes prior to the receipt of the criminalbackground check that he or she has beenconvicted of, pled guilty or pled nolo con-tendere to in this state or any other state orhas been found guilty of a crime, which ifcommitted in Missouri would be a class A orB felony violation of Chapter 565, 566, or569, RSMo or any violation of subsection198.070.3, RSMo or of section 568.020,RSMo, will not have contact with residents.I/II
2. Upon receipt of the criminal back-ground check, the facility must ensure that ifthe criminal background check indicates thatthe person hired or retained by the facility hasbeen convicted of, pled guilty or pled nolocontendere to in this state or any other stateor has been found guilty of a crime, which ifcommitted in Missouri would be a class A orB felony violation of Chapter 565, 566, or569, RSMo or any violation of subsection198.070.3, RSMo or of section 568.020,RSMo, the person will not have contact withresidents unless the facility obtains verifica-
tion from the department that a good causewaiver has been granted and maintains a copyof the verification in the individual’s person-nel file; I/II
(B) Make an inquiry to the department,whether the person is listed on the employeedisqualification list as provided in section660.315, RSMo. The inquiry may be madevia Internet at www.dhss.mo.gov/EDL/;II/III
(C) If the person has registered with thedepartment’s Family Care Safety Registry(FCSR), the facility may utilize the Registryin order to meet the requirements of subsec-tions (1)(A) and (11)(B) of this rule. TheFCSR is available via Internet atwww.dhss.mo.gov/EDL/; and II/III
(D) For persons for whom the facility hascontracted for professional services (e.g.,plumbing or air conditioning repair) that willhave contact with any resident, the facilitymust either require a criminal backgroundcheck or ensure that the individual is suffi-ciently monitored by facility staff while in thefacility to reasonably ensure the safety of allresidents. I/II
(12) A facility shall not employ as an agent oremployee who has access to controlled sub-stances any person who has been found guiltyor entered a plea of guilty or nolo contenderein a criminal prosecution under the laws ofany state or of the United States for anyoffense related to controlled substances. II
(A) A facility may apply in writing to thedepartment for a waiver of this section for aspecific employee.
(B) The department may issue a writtenwaiver to a facility upon determination that awaiver would be consistent with the publichealth and safety. In making this determina-tion, the department shall consider the dutiesof the employee, the circumstances surround-ing the conviction, the length of time sincethe conviction was entered, whether a waiverhas been granted by the department’s Bureauof Narcotics and Dangerous Drugs pursuantto 19 CSR 30-1.034 when the facility is reg-istered with that agency, whether a waiver hasbeen granted by the federal Drug Enforce-ment Administration (DEA) pursuant to 21CFR 1301.76 when the facility is also regis-tered with that agency, the security measurestaken by the facility to prevent the theft anddiversion of controlled substances, and anyother factors consistent with public healthand safety. II/III
(13) The facility must develop and implementwritten policies and procedures which requirethat persons hired for any position which is tohave contact with any patient or resident have
CODE OF STATE REGULATIONS 13ROBIN CARNAHAN (4/30/09)Secretary of State
Chapter 86—Residential Care Facilities and Assisted Living Facilities 19 CSR 30-86
been informed of their responsibility to dis-close their prior criminal history to the facil-ity as required by section 660.317.5, RSMo.The facility must also develop and implementpolicies and procedures which ensure that thefacility does not knowingly hire, after August28, 1997, any person who has or may havecontact with a patient or resident, who hasbeen convicted of, plead guilty or nolo con-tendere to, in this state or any other state, orhas been found guilty of any class A or Bfelony violation of Chapter 565, 566 or 569,RSMo, or any violation of subsection 3 ofsection 198.070, RSMo, or of section568.020, RSMo. II/III
(14) All persons who have or may have con-tact with residents shall at all time when onduty or delivering services wear an identifi-cation badge. The badge shall give theirname, title and, if applicable, the status oftheir license or certification as any kind ofhealth care professional. This rule shall applyto all personnel who provide services to anyresident directly or indirectly. III
(15) All personnel shall be able physicallyand emotionally to work in a long-term carefacility. I/II
(16) Personnel who have been diagnosed witha communicable disease may begin work orreturn to duty only with written approval by aphysician or physician’s designee which indi-cates any limitations. II
(17) The administrator/manager shall beresponsible for preventing an employeeknown to be diagnosed with communicabledisease from exposing residents to such dis-ease. The facility’s policies and proceduresmust comply with the department’s regula-tions pertaining to communicable diseases,specifically 19 CSR 20-20.010 through 19CSR 20-20.100. II/III
(18) The facility shall screen residents andstaff for tuberculosis as required for long-term care facilities by 19 CSR 20-20.100. II
(19) Prior to or on the first day that a newemployee works in the facility he or she shallreceive orientation of at least one (1) hourappropriate to his or her job function. Thisshall include at least the following:
(A) Job responsibilities;(B) Emergency response procedures;(C) Infection control and handwashing pro-
cedures and requirements;(D) Confidentiality of resident informa-
tion;(E) Preservation of resident dignity;
(F) Information regarding what constitutesabuse/neglect and how to report abuse/neglect to the department (1-800-392-0210);
(G) Information regarding the EmployeeDisqualification List;
(H) Instruction regarding the rights of res-idents and protection of property; and
(I) Instruction regarding working with res-idents with mental illness. II/III
(20) In addition to the orientation trainingrequired in section (19) of this rule any facil-ity that provides care to any resident havingAlzheimer’s disease or related dementia shallprovide orientation training regarding mental-ly confused residents such as those withAlzheimer’s disease and related dementias asfollows:
(A) For employees providing direct care tosuch persons, the orientation training shallinclude at least three (3) hours of trainingincluding at a minimum an overview of men-tally confused residents such as those havingAlzheimer’s disease and related dementias,communicating with persons with dementia,behavior management, promoting indepen-dence in activities of daily living, and under-standing and dealing with family issues; II/III
(B) For other employees who do not pro-vide direct care for, but may have daily con-tact with, such persons, the orientation train-ing shall include at least one (1) hour oftraining including at a minimum an overviewof mentally confused residents such as thosehaving dementias as well as communicatingwith persons with dementia; and II/III
(C) For all employees involved in the careof persons with dementia, dementia-specifictraining shall be incorporated into ongoingin-service curricula. II/III
(21) The administrator/manager shall main-tain on the premises an individual personnelrecord on each facility employee, which shallinclude the following:
(A) The employee’s name and address;(B) Social Security number;(C) Date of birth;(D) Date of employment;(E) Documentation of experience and edu-
cation including for positions requiring licen-sure or certification, documentation evidenc-ing competency for the position held, whichincludes copies of current licenses, tran-scripts when applicable, or for those individ-uals requiring certification, such as level Imedication aides (LIMA), certified nurseaides, certified medication technicians(CMT) and insulin administration aides;printing the Web Registry search results pageavailable at www.dhss.mo.gov/cnaregistry
shall meet the requirements of the employer’scheck regarding valid certification:
(F) References, if available;(G) The results of background checks
required by section 660.317, RSMo; and acopy of any good cause waiver granted by thedepartment, if applicable;
(H) Position in the facility;(I) Written statement signed by a licensed
physician or physician’s designee indicatingthe person can work in a long-term care facil-ity and indicating any limitations;
(J) Documentation of the employee’s tuber-cilin screening status;
(K) Documentation of what the employeewas instructed on during orientation training;and
(L) Reason for termination if the employeewas terminated due to abuse or neglect of aresident, residents’ rights issues or residentinjury. III
(22) Personnel records shall be maintainedfor at least two (2) years following termina-tion of employment. III
(23) There shall be written documentationmaintained in the facility showing actualhours worked by each employee. III
(24) No one individual shall be on duty withresponsibility for oversight of residents longerthan eighteen (18) hours per day except in aresidential care facility licensed for twelve(12) or fewer residents. I/II
(25) Employees who are counted in meetingthe minimum staffing ratio and employeeswho provide direct care to the residents shallbe at least sixteen (16) years of age. III
(26) One (1) employee at least eighteen (18)years of age shall be on duty at all times. I/II
(27) Staffing for Residential Care Facility.(A) The facility shall have an adequate
number and type of personnel on duty at alltimes for the proper care of residents andupkeep of the facility. At a minimum, one (1)employee shall be on duty for every forty (40)residents to provide protective oversight toresidents and for fire safety. I/II
Staff Residents1 1–402 41–803 81–1204 121–160
(B) The required staff person shall be inthe facility awake, dressed and prepared toassist residents in case of emergency, exceptthat in a facility licensed for twelve (12) orfewer residents, this person may be asleepduring the night hours. In a facility licensed
14 CODE OF STATE REGULATIONS (4/30/09) ROBIN CARNAHAN
Secretary of State
19 CSR 30-86—DEPARTMENT OF HEALTH ANDSENIOR SERVICES Division 30—Division of Regulation and Licensure
for twenty (20) or fewer residents, therequired staff person may be asleep if there isa sprinkler system or if there is a completeautomatic fire detection system. I/II
(C) In a facility of more than one hundred(100) residents, the administrator/managershall not be counted when determining thepersonnel required. II
(D) If the facility is opened in conjunctionwith and is immediately adjacent to and con-tiguous to another licensed long-term carefacility and if—
1. The resident bedrooms of the resi-dential care facility are on the same floor oron the ground floor immediately below thatof the other licensed facility;
2. There is an approved call system ineach resident’s bedroom and bathroom or apatient-controlled system connected to a nurs-ing station of the other licensed facility;
3. There is a complete fire alarm systemin the residential care facility connected tothe complete fire alarm system in the otherlicensed facility;
4. The staffing of the other licensedfacility is greater than their minimumrequirements; and
5. Periodic visits to the residential carefacility are made by a staff person to deter-mine the welfare of the resident in the resi-dential care facility; then, for a facility serv-ing twenty (20) or fewer residents, there neednot be an attendant on duty during the dayand evening shifts and the attendant may beasleep during the night shift; or if the facilityis on the same floor as the other licensedfacility, there need not be an attendant atnight. If there are more than twenty (20) res-idents, there shall be at least one (1) staff per-son awake and dressed at all times for everyforty (40) residents or fraction of forty (40).I/II
(E) Those facilities which have only anasleep attendant during the night-time periodand those facilities which have only the min-imum staff required by subsection (27)(D)during the night-time period shall not acceptresidents who are blind, use assistive devices,such as walkers or wheelchairs, or who needcare greater than can be provided with thestaffing pattern in those facilities. Those res-idents who were living in a residential carefacility prior to July 11, 1980, may remain inthat facility with an asleep attendant eventhough they may be blind, deaf or use assis-tive devices provided they can demonstratethe ability to reach safety unassisted or withassistive devices. II
(28) All residents shall be physically andmentally capable of negotiating a normal pathto safety unassisted or with the use of assis-tive devices within five (5) minutes of being
alerted of the need to evacuate the facility asdefined in subsection (1)(C) of this rule. I/II
(29) Residents suffering from short periods ofincapacity due to illness, injury or recupera-tion from surgery may be allowed to remainor be readmitted from a hospital if the periodof incapacity does not exceed forty-five (45)days and written approval of a physician isobtained for the resident to remain in or bereadmitted to the facility. II/III
(30) The facility shall not admit or continueto care for residents whose needs cannot bemet. If necessary services cannot be obtainedin or by the facility, the resident shall bepromptly referred to appropriate outsideresources or discharged from the facility. I/II
(31) In the event a resident is transferredfrom the facility, staff shall forward a reportof the resident’s current medical status,physician’s orders/prescriptions, and if appli-cable, a copy of the resident’s advanceddirectives/living will to the facility to whichthe resident is being transferred. If the resi-dent is transferring to a private residence,facility staff shall provide the reports to theresident or his or her designee or legallyauthorized representative. II/III
(32) Residents admitted to a facility on refer-ral by the Department of Mental Health shallhave an individual treatment plan or individ-ual habilitation plan on file prepared by theDepartment of Mental Health, updated annu-ally. II
(33) Placement of residents in the buildingshall be determined by their abilities. Thoseresidents who require the use of a walker orwho are blind shall be housed on a floorwhich has direct exits at grade, a ramp or nomore than two (2) steps to grade with ahandrail unless an area of refuge as defined in19 CSR 30-86.022 is provided. Those resi-dents who use a wheelchair shall be able todemonstrate the ability to transfer to andfrom the wheelchair unassisted. They shall behoused near an exit and there shall be a directexit at grade or a ramp or an area of refugeas defined in 19 CSR 30-86.022. II
(34) Requirements for facilities which admitor retain residents with mental illness ormental retardation diagnosis and residentswith assaultive or disruptive behaviors:
(A) Each resident who exhibits mental andpsychosocial adjustment difficulty(ies) shallreceive treatment and services to address theresident’s needs and behaviors as stated in theindividual service plan; I/II
(B) If specialized rehabilitative services formental illness or mental retardation arerequired to enable a resident to reach and tocomply with the individualized service plan,the facility must ensure the required servicesare provided; and II
(C) The facility shall maintain in the resi-dent’s record the most recent progress notesand personal plan developed and provided bythe Department of Mental Health or desig-nated administrative agent for each residentwhose care is funded by the Department ofMental Health or designated administrativeagent. III
(35) The use of interventions to manage dis-ruptive or assaultive resident behaviors shallbe employed with sufficient safeguards toensure the safety, welfare and rights of theresident and shall be in accordance with thetherapeutic goals for the resident. I/II
(36) Residents under sixteen (16) years of ageshall not be admitted. III
(37) Residents admitted or readmitted to thefacility shall have an admission physical ex-amination by a licensed physician. Docu-mentation should be obtained prior to admis-sion but shall be on file not later than ten (10)days after admission and shall contain infor-mation regarding the resident’s current medi-cal status and any special orders or proce-dures which should be followed. If theresident is admitted directly from a hospitalor another long-term care facility and isaccompanied on admission by a report whichreflects his/her current medical status, anadmission physical will not be required. II/III
(38) The facility shall follow appropriateinfection control procedures. The administra-tor or his or her designee shall make a reportto the local health authority or the departmentof the presence or suspected presence of anydiseases or findings listed in 19 CSR 20-20.020, sections (1)–(3) according to thespecified time frames as follows:
(A) Category I diseases or findings shall bereported to the local health authority or to thedepartment within twenty-four (24) hours offirst knowledge or suspicion by telephone,facsimile, or other rapid communication;I/II
(B) Category II diseases or findings shallbe reported to the local health authority orthe department within three (3) days of firstknowledge or suspicion; I/II
(C) Category III. The occurrence of anoutbreak or epidemic of any illness, diseaseor condition which may be of public healthconcern, including any illness in a food han-dler that is potentially transmissible through
CODE OF STATE REGULATIONS 15ROBIN CARNAHAN (4/30/09)Secretary of State
Chapter 86—Residential Care Facilities and Assisted Living Facilities 19 CSR 30-86
food. This also includes public health threatssuch as clusters of unusual diseases or mani-festations of illness and clusters of unex-plained deaths. Such incidents shall bereported to the local authority or to thedepartment by telephone, facsimile, or otherrapid communication within twenty-four (24)hours of first knowledge or suspicion. I/II
(39) Protective oversight shall be providedtwenty-four (24) hours a day. For residentsdeparting the premises on voluntary leave,the facility shall have, at a minimum, a pro-cedure to inquire of the resident or resident’sguardian of the resident’s departure, of theresident’s estimated length of absence fromthe facility, and of the resident’s whereaboutswhile on voluntary leave. I/II
(40) Residents shall receive proper care tomeet their needs. Physician orders shall befollowed. I/II
(41) In case of behaviors that present a rea-sonable likelihood of serious harm to himselfor herself or others, serious illness, signifi-cant change in condition, injury or death,staff shall take appropriate action and shallpromptly attempt to contact the individuallisted in the resident’s record as the legallyauthorized representative, designee or place-ment authority. The facility shall contact theattending physician or designee and notify thelocal coroner or medical examiner immedi-ately upon the death of any resident of thefacility prior to transferring the deceased res-ident to a funeral home. II/III
(42) The facility shall encourage and assisteach resident based on his or her individualpreferences and needs, to be clean and free ofbody and mouth odor. II
(43) Except in the case of emergency, the res-ident shall not be inhibited by chemicaland/or physical restraints that would limitself-care or ability to negotiate a path to safe-ty unassisted or with assistive devices. I/II
(44) If the resident brings unsealed medica-tions to the facility, the medications shall notbe used unless a pharmacist, physician ornurse examines, identifies and determines thecontents to be suitable for use. The individ-ual performing the identification shall docu-ment his or her review. II/III
(45) Self-control of prescription medicationby a resident may be allowed only if approvedin writing by the resident’s physician andallowed by facility policy. A resident may bepermitted to control the storage and use ofnonprescription medication unless there is a
physician’s written order or facility policy tothe contrary. Written approval for self-controlof prescription medication shall be rewrittenas needed but at least annually and after anyperiod of hospitalization. II/III
(46) All medication shall be safely stored atproper temperature and shall be kept in asecured location behind at least one (1)locked door or cabinet. Medication shall beaccessible only to persons authorized toadminister medications. II/III
(A) If access is controlled by the resident,a secured location shall mean in a lockedcontainer, a locked drawer in a bedside tableor dresser or in a resident’s private room iflocked in his or her absence, although thisdoes not preclude access by a responsibleemployee of the facility. II/III
(B) Schedule II controlled substances shallbe stored in locked compartments separatefrom non-controlled medications, except thatsingle doses of Schedule II controlled sub-stances may be controlled by a resident incompliance with the requirements for self-control of medication of this rule. II/III
(C) Medication that is not in current useand is not destroyed shall be stored separate-ly from medication that is in current use.II/III
(47) All prescription medications shall besupplied as individual prescriptions exceptwhere an emergency medication supply isallowed. All medications, including over-the-counter medications shall be packaged andlabeled in accordance with applicable profes-sional pharmacy standards and state and fed-eral drug laws. Labeling shall include acces-sory and cautionary instructions as well asthe expiration date, when applicable, and thename of the medication as specified in thephysician’s order. Medication labels shall notbe altered by facility staff and medicationsshall not be repackaged by facility staff exceptas allowed by section (48) of this rule. Over-the-counter medications for individual resi-dents shall be labeled with at least the resi-dent’s name. II/III
(48) Controlled substances and other pre-scription and non-prescription medicationsfor administration when a resident temporar-ily leaves a facility shall be provided as fol-lows:
(A) Separate containers of medications forthe leave period may be prepared by the phar-macy. The facility shall have a policy andprocedure for families to provide adequateadvance notice so that medications can beobtained from the pharmacy; II/III
(B) Prescription medication cards or othermultiple-dose prescription containers current-ly in use in the facility may be provided byany authorized facility medication staff mem-ber if the containers are labeled by the phar-macy with complete pharmacy prescriptionlabeling for use. Original manufacturer con-tainers of non-prescription medications,along with instructions for administration,may be provided by any authorized facilitymedication staff member; II/III
(C) When medications are supplied by thepharmacy in customized patient medicationpackages that allow separation of individualdose containers, the required number of con-tainers may be provided by any authorizedfacility medication staff member. The indi-vidual dose containers shall be placed in anouter container that is labeled with the nameand address of the facility and the date; II/III
(D) When multiple doses of a medicationare required and it is not reasonably possibleto obtain prescription medication labeled bythe pharmacy, and it is not appropriate tosend a container of medication currently inuse in the facility, up to a twenty-four (24)-hour supply of each prescription or non-pre-scription medication may be provided by alicensed nurse in United States Pharmacopeia(USP) approved containers labeled with thefacility name and address, resident’s name,medication name and strength, quantity,instructions for use, date, initials of individu-al providing, and other appropriate informa-tion; II/III
(E) When no more than a single dose of amedication is required, any authorized facili-ty medication staff member may prepare thedose as for in-facility administration in a USPapproved container labeled with the facilityname and address, resident’s name, medica-tion name and strength, quantity, instructionsfor use, date, initials of person providing, andother appropriate information;
(F) The facility may have a policy that lim-its the quantity of medication sent with a res-ident without prior approval of the prescriber;II/III
(G) Returned containers shall be identifiedas having been sent with the resident, andshall not later be returned to the pharmacy forreuse; and II/III
(H) The facility shall maintain accuraterecords of medications provided to andreturned by the resident. II/III
(49) Upon discharge or transfer of a resident,the facility shall release prescription medica-tions, including controlled substances, heldby the facility for the resident when the physi-cian writes an order for each medication to bereleased. Medications shall be labeled by the
16 CODE OF STATE REGULATIONS (4/30/09) ROBIN CARNAHAN
Secretary of State
19 CSR 30-86—DEPARTMENT OF HEALTH ANDSENIOR SERVICES Division 30—Division of Regulation and Licensure
CODE OF STATE REGULATIONS 17ROBIN CARNAHAN (4/30/09)Secretary of State
Chapter 86—Residential Care Facilities and Assisted Living Facilities 19 CSR 30-86
pharmacy with current instructions for use.Prescription medication cards or other con-tainers may be released if the containers arelabeled by the pharmacy with complete phar-macy prescription labeling. II/III
(50) Injections shall be administered only bya physician or licensed nurse, except thatinsulin injections may be administered by aCMT or LIMA who has successfully com-pleted the state-approved course for insulinadministration, taught by a department-approved instructor. A resident who requiresinsulin, may administer his or her owninsulin if approved in writing by the resi-dent’s physician and trained to do so by alicensed nurse or physician. The facility isresponsible to monitor the resident’s condi-tion and continued ability for self-administra-tion. I/II
(51) The administrator/manager shall developand implement a safe and effective system ofmedication control and use, which assuresthat all residents’ medications are adminis-tered by personnel at least eighteen (18) yearsof age, in accordance with physicians’instructions using acceptable nursing tech-niques. The facility shall employ a licensednurse eight (8) hours per week for every thir-ty (30) residents to monitor each resident’scondition and medication. Administration ofmedication shall mean delivering to a resi-dent his or her prescription medication eitherin the original pharmacy container, or forinternal medication, removing an individualdose from the pharmacy container and plac-ing it in a small container or liquid mediumfor the resident to remove from the containerand self-administer. External prescriptionmedication may be applied by facility person-nel if the resident is unable to do so and theresident’s physician so authorizes. All indi-viduals who administer medication shall betrained in medication administration and, ifnot a physician or a licensed nurse, shall be acertified medication technician or level Imedication aide. I/II
(52) Medication Orders.(A) Physician’s instructions, as evidenced
by the prescription label or by signed order ofa physician, shall be accurately followed. Ifthe physician changes the order which is des-ignated on a prescription label, there shall beon file in the resident’s record a signed physi-cian’s order to that effect with the amendedinstructions for use or until the prescriptionlabel is changed by the pharmacy to reflectthe new order. II/III
(B) Physician’s written and signed ordersare not required, but if it is the facility’s or
physician’s policy to use the orders, they shallinclude: name of the medication, dosage,frequency and route of administration and theorders shall be renewed at least every three(3) months. Computer generated signaturesmay be used if safeguards are in place to pre-vent their misuse. Computer identificationcodes shall be accessible to and used only bythe individuals whose signatures they repre-sent. Orders that include optional doses orinclude pro re nata (PRN) administration fre-quencies shall specify a maximum frequencyand the reason for administration. II/III
(C) Telephone and other verbal ordersshall be received only by a licensed nurse,medication technician, level I medicationaide or pharmacist and shall be immediatelyreduced to writing and signed by that indi-vidual. If a telephone or other verbal order isgiven to a medication technician or level Imedication aide, an initial dosage shall not beadministered until the order has beenreviewed by telephone, facsimile or in personby a licensed nurse or pharmacist. II
(D) The review shall be documented by thelicensed nurse’s or pharmacist’s signaturewithin seven (7) days. III
(E) The physician shall sign all telephoneand other verbal orders within seven (7) days.III
(F) Medication staff shall record adminis-tration of medication on a medication sheet ordirectly in the resident’s record. If adminis-tration of medication is recorded on a medi-cation sheet, the medication sheet shall bemade part of the resident’s medical record.The same individual who prepares andadministers the medication shall record theadministration. II/III
(53) Influenza and pneumococcal polysaccha-ride immunizations may be administered perphysician-approved facility policy afterassessment for contraindications.
(A) The facility shall develop a policy thatprovides recommendations and assessmentparameters for the administration of suchimmunizations. The policy shall be approvedby the facility medical director for facilitieshaving a medical director, or by each resi-dent’s attending physician for facilities thatdo not have a medical director, and shallinclude the requirements to:
1. Provide education regarding thepotential benefits and side effects of theimmunization to each resident or the resi-dent’s designee or legally authorized repre-sentative; II/III
2. Offer the immunization to the resi-dent or obtain permission from the resident’sdesignee or legally authorized representativewhen it is medically indicated, unless the res-
ident has already been immunized as recom-mended by the policy; II/III
3. Provide the opportunity to refuse theimmunization; and II/III
4. Perform an assessment for contraindi-cations. II/III
(B) The assessment for contraindicationsand documentation of the education andopportunity to refuse the immunization shallbe dated and signed by the nurse performingthe assessment and placed in the medicalrecord. II/III
(C) The facility shall with the approval ofeach resident’s physician, access screeningand immunization through outside sources,such as county or city health departments,and the facility shall document in the medicalrecord that the requirements in subsection(53)(B) were performed by outside sources.II/III
(54) Stock supplies of nonprescription medi-cation may be kept when specific medicationsare approved in writing by a consulting physi-cian, a registered nurse or a pharmacist. Nostock supply of prescription medication maybe kept in the facility. II/III
(55) Records shall be maintained uponreceipt and disposition of all controlled sub-stances and shall be maintained separatelyfrom other records, for two (2) years.
(A) Inventories of controlled substancesshall be reconciled as follows: II/III
1. Controlled Substance Schedule IImedications shall be reconciled each shift;and II
2. Controlled Substance Schedule III–Vmedications shall be reconciled at least week-ly and as needed to ensure accountability.II/III
(B) Inventories of controlled substancesshall be reconciled by the following:
1. Two (2) medication personnel, one ofwhom is a licensed nurse; or
2. Two (2) medication personnel, one ofwhom is the administrator/manager when nonurse is available on staff; or
3. Two (2) medication personnel eithermedication technicians or level I medicationaides when neither a licensed nurse nor theadministrator/manager is available. II/III
(C) Receipt records shall include the date,source of supply, resident name and prescrip-tion number when applicable, medicationname and strength, quantity and signature ofthe supplier and receiver. Administrationrecords shall include the date, time, residentname, medication name, dose administeredand the initials of the individual administer-ing. The signature and initials of each medi-cation staff documenting on the medication
administration record must be signed in thesignature area of the medication record.II/III
(D) When self-control of medication isapproved a record shall be made of all con-trolled substances transferred to and adminis-tered from the resident’s room. Inventoryreconciliation shall include controlled sub-stances transferred to the resident’s room.I/II
(56) Documentation of the wasting of con-trolled substances at the time of administra-tion shall include the reason for the waste andthe signature of another medication staffmember or the administrator who witnessesthe waste. If no medication staff member orthe administrator is available at the time ofadministration, the controlled substance shallbe properly labeled, clearly identified asunusable, stored in a locked area, anddestroyed as soon as a medication staff mem-ber or the administrator is available to wit-ness the waste. When no medication staffmember or the administrator is available andthe controlled substance is contaminated bypatient body fluids, the controlled substanceshall be destroyed immediately and the cir-cumstances documented. II/III
(57) At least every three (3) months in a res-idential care facility, a pharmacist or regis-tered nurse shall review the controlled sub-stance record keeping including reconcilingthe inventories of controlled substances. Thisshall be done at the time of the drug regimenreview of each resident. All discrepancies incontrolled substance records shall be report-ed to the administrator or manager for reviewand investigation. The theft or loss of con-trolled substances shall be reported as fol-lows: II/III
(A) The facility shall notify the depart-ment’s Section for Long Term Care (SLTC)and other appropriate authorities of any theftor significant loss of any controlled substancemedication written as an individual prescrip-tion for a specific resident upon the discoveryof the theft or loss. The facility shall consid-er at least the following factors in determin-ing if a loss is significant:
1. The actual quantity lost in relation tothe total quantity;
2. The specific controlled substancelost;
3. Whether the loss can be associatedwith access by specific individuals;
4. Whether there is a pattern of losses,and if the losses appear to be random or not;
5. Whether the controlled substance isa likely candidate for diversion; and
6. Local trends and other indicators ofdiversion potential; II/III
(B) If an insignificant amount of such con-trolled substance is lost during lawful activi-ties, which includes but are not limited toreceiving, record keeping, access auditing,administration, destruction and returning tothe pharmacy, a description of the occurrenceshall be documented in writing and main-tained with the facility’s controlled substancerecords. The documentation shall include thereason for determining that the loss wasinsignificant. II/III
(58) A pharmacist or registered nurse shallreview the medication regimen of each resi-dent. This shall be done at least every three(3) months in a residential care facility. Thereview shall be performed in the facility andshall include, but shall not be limited to, indi-cation for use, dose, possible medicationinteractions and medication/food interactions,contraindications, adverse reactions and areview of the medication system utilized bythe facility. Irregularities and concerns shallbe reported in writing to the resident’s physi-cian and to the administrator/manager. Ifafter thirty (30) days, there is no action takenby a resident’s physician and significant con-cerns continue regarding a resident’s or resi-dents’ medication order(s), the administra-tor/manager shall contact or recontact thephysician to determine if he or she receivedthe information and if there are any newinstructions. II/III
(59) All medication errors and adverse reac-tions shall be promptly documented andreported to the administrator/manager andthe resident’s physician. If the pharmacymade a dispensing error, it shall also bereported to the issuing pharmacy. II/III
(60) Medications that are not in current useshall be disposed of as follows:
(A) Single doses of contaminated, refused,or otherwise unusable non-controlled sub-stance medications may be destroyed by anyauthorized medication staff member at thetime of administration. Single doses of unus-able controlled substance medications shallbe destroyed according to section (56) of thisrule;
(B) Discontinued medications may beretained up to one hundred twenty (120) daysprior to other disposition if there is reason tobelieve, based on clinical assessment of theresident, that the medication might bereordered;
(C) Medications may be released to theresident or family upon discharge accordingto section (49) of this rule;
(D) After a resident has expired, medica-tions, except for controlled substances, maybe released to the resident’s legal representa-tive upon written request of the legal repre-sentative that includes the name of the medi-cation and the reason for the request;
(E) Medications may be returned to thepharmacy that dispensed the medications pur-suant to 4 CSR 220-3.040 or returned pur-suant to the Prescription Drug RepositoryProgram, 19 CSR 20-50.020;
(F) All other medications, including allcontrolled substances and all expired or oth-erwise unusable medications, shall bedestroyed within thirty (30) days as follows:II/III
1. Medications shall be destroyed withinthe facility by a pharmacist and a licensednurse or by two (2) licensed nurses or whentwo (2) licensed nurses are not available onstaff by two (2) individuals who have author-ity to administer medications, one (1) ofwhom shall be a licensed nurse or a pharma-cist; and II/III
2. A record of medication destroyedshall be maintained and shall include the res-ident’s name, date, medication name andstrength, quantity, prescription number, andsignatures of the individuals destroying themedications; and II/III
(G) A record of medication released orreturned to the pharmacy shall be maintainedand shall include the resident’s name, date,medication name and strength, quantity, pre-scription number, and signatures of the indi-viduals releasing and receiving the medica-tions. III
(61) Residents shall be encouraged to beactive and to participate in activities. In a res-idential care facility licensed for more thantwelve (12) residents, a method for informingthe residents in advance of what activities areavailable, where they will be held and at whattimes they will be held shall be developed,maintained and used. II/III
(62) The facility shall maintain a record inthe facility for each resident which shallinclude the following:
(A) Admission information including theresident’s name; admission date; confiden-tiality number; previous address; birth date;sex; marital status; Social Security number;Medicare and Medicaid numbers (if applica-ble); name, address and telephone number ofthe resident’s physician and alternate; diagno-sis; name, address and telephone number ofthe resident’s legally authorized representa-tive or designee to be notified in case of
18 CODE OF STATE REGULATIONS (4/30/09) ROBIN CARNAHAN
Secretary of State
19 CSR 30-86—DEPARTMENT OF HEALTH ANDSENIOR SERVICES Division 30—Division of Regulation and Licensure
emergency; and preferred dentist, pharmacistand funeral director; III
(B) A review monthly or more frequently,if indicated, of the resident’s general condi-tion and needs; a monthly review of medica-tion consumption of any resident controllinghis or her own medication, noting if pre-scription medications are being used inappropriate quantities; a daily record ofadministration of medication; a logging of themedication regimen review process; a month-ly weight; a record of each referral of a resi-dent for services from an outside service; anda record of any resident incidents includingbehaviors that present a reasonable likelihoodof serious harm to himself or herself or oth-ers and accidents that potentially could resultin injury or did result in injuries involving theresident; and III
(C) Any Physician’s Orders. Except asallowed by section (52) of this rule, the facil-ity shall submit to the physician written ver-sions of any oral or telephone orders withinfour (4) days of the giving of the oral or tele-phone order. III
(63) A record of the daily resident censusshall be retained in the facility. III
(64) Resident records shall be maintained bythe operator for at least five (5) years after aresident leaves the facility or after the resi-dent reaches the age of twenty-one (21),whichever is longer and must include reasonfor discharge or transfer from the facility andcause of death, if applicable. III
AUTHORITY: sections 198.005 and 198.006,RSMo Supp. 2006 and 198.076, RSMo2000.* This rule originally filed as 13 CSR15-15.042. Original rule filed July 13, 1983,effective Oct. 13, 1983. Emergency amend-ment filed Aug. 1, 1984, effective Aug. 13,1984, expired Dec. 10, 1984. Amended:Filed Sept. 12, 1984, effective Dec. 13,1984. Amended: Filed March 14, 1985,effective June 13, 1985. Amended: Filed May13, 1987, effective Aug. 13, 1987. Amended:Filed April 17, 1990, effective June 30, 1990.Amended: Filed Feb. 13, 1998, effective Sept.30, 1998. Moved to 19 CSR 30-86.042, effec-tive Aug. 28, 2001. Emergency amendmentfiled Sept. 12, 2003, effective Sept. 22, 2003,expired March 19, 2004. Amended: FiledSept. 12, 2003, effective Feb. 29, 2004.Amended: Filed Aug. 23, 2006, effectiveApril 30, 2007.
*Original authority: 198.005, RSMo 2006; 198.006,
RSMo 1979, amended 1984, 1987, 2003, 2006; and
198.076, RSMo 1979, amended 1984.
19 CSR 30-86.043 Administrative, Person-nel and Resident Care Requirements forFacilities Licensed as a Residential CareFacility II on August 27, 2006 that WillComply with Residential Care Facility IIStandards
PURPOSE: This rule establishes require-ments for administration, personnel and resi-dent care requirements for facilities licensedpursuant to section 198.005, RSMo that con-tinue to comply with residential care facilities(RCF) II standards in effect on August 27,2006.
Editor’s Note: All rules relating to long-termcare facilities licensed by the department arefollowed by a Roman Numeral notation whichrefers to the class (either Class I, II or III) ofstandard as designated in section 198.085.1,RSMo.
(1) This rule contains the administrative, per-sonnel and resident care standards in effecton August 27, 2006 for residential care facil-ity IIs (formerly published at 19 CSR 30-86.042 (effective 12/31/05)). These stan-dards apply to facilities that were licensed asresidential care facility IIs on August 27,2006 and that choose to be inspected underthese standards rather than the standards pub-lished at 19 CSR 30-86.047.
(2) A person shall be designated to be admin-istrator who is currently licensed as a nursinghome administrator under Chapter 344,RSMo. II
(3) By January 1, 1991, the administrator ofa facility shall have successfully completedthe state approved Level I Medication Aidecourse unless s/he is a physician, pharmacist,licensed nurse or a certified medication tech-nician, or if the facility is operating in con-junction with a skilled nursing facility orintermediate care facility on the same premis-es, or if the facility employs on a full-timebasis, a licensed nurse who is available seven(7) days per week. II/III
(4) The operator shall be responsible toassure compliance with all applicable lawsand regulations. The administrator shall befully authorized and empowered to makedecisions regarding the operation of the facil-ity and shall be held responsible for theactions of all employees. The administrator’sresponsibilities shall include oversight of res-idents to assure that they receive appropriatecare. II/III
(5) The administrator shall devote sufficienttime and attention to the management of thefacility as is necessary for the health, safetyand welfare of the residents. II
(6) The administrator cannot be listed orfunction in more than one (1) facility at thesame time unless s/he serves no more thanfour (4) facilities which are within a thirty(30)-mile radius and licensed to serve in totalno more than one hundred (100) residents.However, one (1) administrator may serve asthe administrator of more than one (1)licensed facility if all facilities are on thesame premises. II/III
(7) The administrator shall designate, in writ-ing, a staff person in charge in his/herabsence. If the administrator is absent formore than thirty (30) consecutive days, dur-ing which time s/he is not readily accessiblefor consultation by telephone with the personin charge or if the administrator is absentfrom the facility for more than sixty (60)working days during the course of a calendaryear the person designated to be in chargeshall be a licensed nursing home administra-tor. II/III
(8) The facility shall not care for more resi-dents than the number for which the facilityis licensed. II/III
(9) The facility’s current license shall beposted in a conspicuous place and noticesprovided to the facility by the Department ofHealth and Senior Services (the department)granting exception(s) to regulatory require-ments shall be posted alongside of the facili-ty’s license. III
(10) All personnel responsible for residentcare shall have access to the legal name ofeach resident, name and telephone number ofphysician and next of kin or responsible partyin the event of emergency. II/III
(11) All persons who have any contact withthe residents in the facility shall not know-ingly act or omit any duty in a manner whichwould materially and adversely affect thehealth, safety, welfare or property of resi-dents. No person who is listed on theEmployee Disqualification List maintained bythe department as required by section198.070, RSMo shall work or volunteer inthe facility in any capacity whether or notemployed by the operator. I/II
(12) Effective August 28, 1997, each facilityshall, not later than two (2) working days ofthe date an applicant for a position to have
CODE OF STATE REGULATIONS 19ROBIN CARNAHAN (4/30/09)Secretary of State
Chapter 86—Residential Care Facilities and Assisted Living Facilities 19 CSR 30-86
contact with residents is hired, request acriminal background check, as provided insections 43.530, 43.540 and 610.120,RSMo. Each facility must maintain in itsrecord documents verifying that the back-ground checks were requested and the natureof the response received for each suchrequest. The facility must ensure that anyapplicant who discloses prior to the check ofhis/her criminal records that he/she has beenconvicted of, plead guilty or nolo contendereto, or has been found guilty of any Class Aor B felony violation of Chapter 565, 566, or569, RSMo, or any violation of subsection 3of section 198.070, RSMo, or of section568.020, RSMo, will not be allowed to workin contact with patients or residents until andunless a check of the applicant’s criminalrecord shows that no such convictionoccurred. II/III
(13) The facility must develop and implementwritten policies and procedures which requirethat persons hired for any position which is tohave contact with any patient or resident havebeen informed of their responsibility to dis-close their prior criminal history to the facil-ity as required by section 660.317.5, RSMo.The facility must also develop and implementpolicies and procedures which ensure that thefacility does not knowingly hire, after August28, 1997, any person who has or may havecontact with a patient or resident, who hasbeen convicted of, plead guilty or nolo con-tendere to, in this state or any other state, orhas been found guilty of any Class A or Bfelony violation of Chapter 565, 566 or 569,RSMo, or any violation of subsection 3 ofsection 198.070, RSMo, or of section568.020, RSMo. II/III
(14) All persons who have or may have con-tact with residents shall at all times when onduty or delivering services wear an identifi-cation badge. The badge shall give theirname, title and, if applicable, the status oftheir license or certification as any kind ofhealth care professional. This rule shall applyto all personnel who provide services to anyresident directly or indirectly. III
(15) All personnel shall be able physicallyand emotionally to work in a long-term carefacility. I/II
(16) Personnel who have been diagnosed witha communicable disease may begin work orreturn to duty only with written approval by aphysician or physician’s designee which indi-cates any limitations. II
(17) The administrator shall be responsiblefor monitoring the health of the employees.II/III
(18) Prior to or on the first day that a newemployee works in the facility s/he shallreceive orientation of at least one (1) hourappropriate to his/her job function. This shallinclude, at a minimum, job responsibilities,how to handle emergency situations, theimportance of infection control and hand-washing, confidentiality of resident informa-tion, preservation of resident dignity, how toreport abuse/neglect to the department (1-800-392-0210), information regarding theEmployee Disqualification List and instruc-tion regarding the rights of residents and pro-tection of property. II/III
(19) The administrator shall maintain on thepremises an individual personnel record oneach employee of the facility which shallinclude: the employee’s name and address;Social Security number; date of birth; date ofemployment; experience and educationincluding documentation of specialized train-ing on medication and/or insulin administra-tion, or both; references, if available; theresults of background checks required by sec-tion 660.317, RSMo; position in the facility;written statement signed by a licensed physi-cian or physician’s designee indicating theperson can work in a long-term care facilityand indicating any limitations; record that theemployee was instructed on residents’ rights,facility’s policies, job duties and any otherorientation and reason for termination. Per-sonnel records shall be maintained for at leastone (1) year following termination of employ-ment. III
(20) There shall be written documentationmaintained in the facility showing actualhours worked by each employee. III
(21) No one individual shall be on duty withresponsibility for oversight of residents longerthan eighteen (18) hours per day. I/II
(22) Employees who are counted in meetingthe minimum staffing ratio and employeeswho provide direct care to the residents shallbe at least sixteen (16) years of age. III
(23) One (1) employee at least eighteen (18)years of age shall be on duty at all times. I/II
(24) Staffing. (A) The facility shall have an adequate
number and type of personnel for the propercare of residents and upkeep of the facility. Ata minimum, the staffing pattern for fire safe-
ty and care of residents shall be one (1) staffperson for every fifteen (15) residents ormajor fraction of fifteen (15) during the dayshift, one (1) person for every twenty (20)residents or major fraction of twenty (20)during the evening shift and one (1) personfor every twenty-five (25) residents or majorfraction of twenty-five (25) during the nightshift. I/II
Time Personnel Residents7 a.m. to 3 p.m.
(Day)* 1 3–153 p.m. to 9 p.m.
(Evening)* 1 3–209 p.m. to 7 a.m.
(Night)* 1 3–25
*If the shift hours vary from those indicated,the hours of the shifts shall show on the workschedules of the facility and shall not be lessthan six (6) hours. III
(B) The required staff shall be in the facil-ity awake, dressed and prepared to assist res-idents in case of emergency. I/II
(C) In a facility of more than one hundred(100) residents, the administrator shall not becounted when determining the personnelrequired. II
(D) If the facility is operated in conjunc-tion with and is immediately adjacent to andcontiguous to another licensed long-term carefacility and if the resident bedrooms of thefacility are on the same floor as at least a por-tion of a licensed intermediate care or skillednursing facility; there is an approved call sys-tem in each resident’s bedroom and bathroomor a patient-controlled call system; and thereis a complete fire alarm system in the facilitytied into the complete fire alarm system in theother licensed facility, then the followingminimum staffing for oversight and care ofresidents, for upkeep of the facility and forfire safety shall be one (1) staff person forevery eighteen (18) residents or major frac-tion of residents during the day shift, one (1)person for every twenty-five (25) residents ormajor fraction of residents during the eveningshift and one (1) person for every thirty (30)residents or major fraction of residents dur-ing the night shift. I/II
Time Personnel Residents7 a.m. to 3 p.m.
(Day)* 1 3–183 p.m. to 9 p.m.
(Evening)* 1 3–259 p.m. to 7 a.m.
(Night)* 1 3–30
*If the shift hours vary from those indicated,the hours of the shifts shall show on the workschedules of the facility and shall not be less
20 CODE OF STATE REGULATIONS (4/30/09) ROBIN CARNAHAN
Secretary of State
19 CSR 30-86—DEPARTMENT OF HEALTH ANDSENIOR SERVICES Division 30—Division of Regulation and Licensure
than six (6) hours. III(E) There shall be a licensed nurse
employed by the facility to work at least eight(8) hours per week at the facility for everythirty (30) residents or additional major frac-tion of thirty (30). The nurse’s duties shallinclude, but shall not be limited to, review ofresidents’ charts, medications and specialdiets or other orders, review of each resi-dent’s adjustment to the facility and observa-tion of each individual resident’s generalphysical and mental condition. The nurseshall inform the administrator of any prob-lems noted and these shall be brought to theattention of the resident’s physician. II/III
(25) All residents shall be physically andmentally capable of negotiating a normal pathto safety unassisted or with the use of assis-tive devices. I/II
(26) Residents suffering from short periods ofincapacity due to illness, injury or recupera-tion from surgery may be allowed to remainor be readmitted from a hospital if the periodof incapacity does not exceed forty-five (45)days and written approval of a physician isobtained for the resident to remain in or bereadmitted to the facility. II/III
(27) The facility shall not admit or continueto care for residents whose needs cannot bemet. If necessary services cannot be obtainedin or by the facility, the resident shall bepromptly referred to appropriate outsideresources or transferred to a facility providingthe appropriate level of care. I/II
(28) In the event a resident is transferredfrom the facility, a report of the resident’scurrent medical status shall accompanyhim/her. III
(29) Residents admitted to a facility on refer-ral by the Department of Mental Health shallhave an individual treatment plan or individ-ual habilitation plan on file prepared by theDepartment of Mental Health, updated annu-ally. III
(30) Residents under sixteen (16) years of ageshall not be admitted. III
(31) Placement of residents in the buildingshall be determined by their abilities. Thoseresidents who require the use of a walker orwho are blind shall be housed on a floorwhich has direct exits at grade, a ramp or nomore than two (2) steps to grade with ahandrail. Those residents who use awheelchair shall be able to demonstrate theability to transfer to and from the wheelchair
unassisted. They shall be housed near an exitand there shall be a direct exit at grade or aramp. II
(32) Residents admitted or readmitted to thefacility shall have an admission physicalexamination by a licensed physician. Docu-mentation should be obtained prior to admis-sion but shall be on file not later than ten (10)days after admission and shall contain infor-mation regarding the resident’s current medi-cal status and any special orders or proce-dures which should be followed. If theresident is admitted directly from a hospitalor another long-term care facility and isaccompanied on admission by a report whichreflects his/her current medical status, anadmission physical will not be required. II/III
(33) If at any time a resident or prospectiveresident is diagnosed with a communicabledisease, the department shall be notifiedwithin seven (7) days and if the facility canmeet the resident’s needs, the resident may beadmitted or does not need to be transferred.Appropriate infection control proceduresshall be followed if the resident remains in oris accepted by the facility. I/II
(34) Protective oversight shall be providedtwenty-four (24) hours a day. For residentsdeparting the premises on voluntary leave,the facility shall have, at a minimum, a pro-cedure to inquire of the resident or resident’sguardian of the resident’s departure, of theresident’s estimated length of absence fromthe facility, and of the resident’s whereaboutswhile on voluntary leave. I/II
(35) Residents shall receive proper care tomeet their needs. Physician orders shall befollowed. I/II
(36) In case of serious illness, accident ordeath, appropriate action shall be taken andthe person designated in the resident’s recordas the responsible party and, if applicable,the guardian shall be immediately notified.II/III
(37) Every resident shall be clean, dry andfree of offensive body and mouth odor. I/II
(38) Except in the case of emergency, the res-ident shall not be inhibited by chemicaland/or physical restraints that would limitself-care or ability to negotiate a path to safe-ty unassisted or with assistive devices. I/II
(39) A supply of clean linen shall be availablein the facility and provided to residents tomeet their daily needs. II/III
(40) Beds shall be made daily and linenchanged at least weekly or more often ifneeded to maintain a clean, dry bed. II/III
(41) The resident’s unit shall be thoroughlycleaned and disinfected following a resident’sdeath, discharge or transfer. II/III
(42) Commodes and urinals, if used, shall bekept at the bedside of the residents. Theyshall not be left open and the container shallbe emptied promptly and thoroughly cleanedafter each use. III
(43) Cuspidors shall be emptied and cleaneddaily or disposable cartons shall be provideddaily. III
(44) Self-control of prescription medicationby a resident may be allowed only if approvedin writing by the resident’s physician andallowed by facility policy. If a resident is nottaking any prescription medication, the resi-dent may be permitted to control the storageand use of nonprescription medication unlessthere is a physician’s written order or facilitypolicy to the contrary. If not permitted, allmedications for that resident, including over-the-counter medications, shall be controlledby the administrator unless the physicianspecifies otherwise. II/III
(45) Written approval for self-control of pre-scription medication shall be rewritten asneeded but at least annually and after anyperiod of hospitalization. III
(46) All medication shall be safely stored atproper temperature and shall be kept in asecured location behind at least one (1)locked door or cabinet. If access is controlledby the resident, a secured location shall meanin a locked container, a locked drawer in abedside table or dresser or in a resident’s pri-vate room if locked in his/her absence,although this does not preclude access by aresponsible employee of the facility. II/III
(47) All prescription medications shall besupplied as individual prescriptions. All med-ications, including over-the-counter medica-tions shall be packaged and labeled in accor-dance with applicable professional pharmacystandards, state and federal drug laws andregulations and the United States Pharma-copeia (USP). Labeling shall include acces-sory and cautionary instructions as well asthe expiration date, when applicable, and thename of the medication as specified in thephysician’s order. Over-the-counter medica-tions for individual residents shall be labeledwith at least the resident’s name. II/III
CODE OF STATE REGULATIONS 21ROBIN CARNAHAN (4/30/09)Secretary of State
Chapter 86—Residential Care Facilities and Assisted Living Facilities 19 CSR 30-86
(48) Injections shall be administered only bya physician or licensed nurse, except that res-idents who require insulin, upon writtenorder of their physician, may administer theirown insulin or the insulin may be adminis-tered by a person trained to do so by alicensed nurse or physician and the resident’scondition shall be monitored by his/her physi-cian. After December 31, 1990, unlessinsulin is self-administered or it is adminis-tered only by a physician or licensed nurse,it shall be administered by a certified medi-cation technician or a level I medication aidewho has successfully completed the state-approved course for insulin administration,taught by an approved instructor and who wasrecommended for training by an administra-tor or nurse with whom he or she works.Anyone trained prior to December 31, 1990,who completed the state-approved insulinadministration course taught by an approvedinstructor shall be considered qualified toadminister insulin in a facility. Anyonetrained prior to December 31, 1990, toadminister insulin by a licensed nurse orphysician not using the state-approved coursemay qualify by challenging the final examina-tion of the insulin administration course. I/II
(49) The administrator shall develop andimplement a safe and effective system ofmedication control and use which assures thatall residents’ medications are administered ordistributed by personnel at least eighteen (18)years of age, in accordance with physicians’instructions using acceptable nursing tech-niques. Until January 1, 1991, those facilitiesadministering medications shall utilize per-sonnel trained in medication administration(a licensed nurse, certified medication techni-cian or level I medication aide) and shallemploy a licensed nurse eight (8) hours perweek for every thirty (30) residents to moni-tor each resident’s condition. Distributionshall mean delivering to a resident his/herprescription medication either in the originalpharmacy container, or for internal medica-tion, removing an individual dose from thepharmacy container and placing it in a smallcontainer or liquid medium for the resident toremove from the container and self-adminis-ter. External prescription medication may beapplied by facility personnel if the resident isunable to do so and the resident’s physicianso authorizes. After December 31, 1990, allpersons who administer or distribute medica-tion shall be trained in medication adminis-tration and, if not a physician or a licensednurse, shall be a certified medication techni-cian or level I medication aide. I/II
(50) Medication Orders.
(A) Physician’s instructions, as evidencedby the prescription label or by signed order ofa physician, shall be accurately followed. Ifthe physician changes the order which is des-ignated on a prescription label, there shall beon file in the resident’s record a signed physi-cian’s order to that effect with the amendedinstructions for use or until the prescriptionlabel is changed by the pharmacy to reflectthe new order. II/III
(B) Physician’s written and signed ordersare not required, but if it is the facility’s orphysician’s policy to use the orders, they shallinclude: name of medication, dosage and fre-quency of administration and the orders shallbe renewed at least every three (3) months.II/III
(C) Verbal and telephone orders shall betaken only by a licensed nurse, medicationtechnician, level I medication aide or phar-macist and shall be immediately reduced towriting and signed by that individual. If atelephone order is given to a medication tech-nician or level I medication aide, an initialdosage of a new prescription shall not be ini-tiated until the order has been reviewed bytelephone or in person by a licensed nurse orpharmacist. II
(D) The review shall be documented by thenurse’s or pharmacist’s signature withinseven (7) days. III
(E) The physician shall sign all verbal andtelephone orders within seven (7) days. III
(F) The administration or distribution ofmedication shall be recorded on a medicationsheet or directly in the resident’s record and,if recorded on a medication sheet, shall bemade part of the resident’s record. Theadministration or distribution shall be record-ed by the same person who prepares the med-ication and who distributes or administers it.II/III
(51) A stock supply of prescription medica-tion may be kept in the facility. An emergen-cy drug supply as recommended by a phar-macist or physician may be kept if approvedby the department. Storage and use of medi-cations in the emergency drug supply shallassure accountability. II/III
(52) Stock supplies of nonprescription medi-cation may be kept for pro re nata (PRN) usein facilities as long as the particular medica-tions are approved in writing by a consultingphysician, a registered nurse or a pharmacist.II/III
(53) All controlled substances shall be han-dled according to state laws and regulationsas given in and required by 19 CSR 30-1 andChapter 195, RSMo. II/III
(54) A pharmacist or registered nurse shallreview the drug regimen of each resident.This shall be done at least every other monthin a facility. The review shall be performed inthe facility and shall include, but shall not belimited to, possible drug and food interac-tions, contraindications, adverse reactionsand a review of the medication system uti-lized by the facility. Irregularities and con-cerns shall be reported in writing to the resi-dent’s physician and to the administrator. Ifafter thirty (30) days, there is no action takenby a resident’s physician and significant con-cerns continue regarding a resident’s or resi-dents’ medication order(s), the administratorshall contact or recontact the physician todetermine if he or she received the informa-tion and if there are any new instructions.II/III
(55) Medications controlled by the facilityshall be disposed of either by destroying,returning to the pharmacy or sending withresidents on discharge. The following shall bedestroyed within the facility within ninety(90) days: discontinued medication notreturnable to the pharmacy, all discontinuedcontrolled substances, outdated or deteriorat-ed medication, medication of expired resi-dents not returnable to the pharmacy andmedications not sent with the resident on dis-charge. II/III
(56) Disposition of medication controlled bythe facility shall be recorded listing the resi-dent’s name, the date and the name, strengthand quantity of the drug and the signature(s)of the person(s) involved. Medicationdestruction shall involve two (2) persons, one(1) of whom shall be a pharmacist, a nurse ora state inspector. III
(57) Residents shall be encouraged to beactive and to participate in activities. In afacility licensed for more than twelve (12)residents, a method for informing the resi-dents in advance of what activities are avail-able, where they will be held and at whattimes they will be held shall be developed,maintained and used. II/III
(58) A record shall be maintained in the facil-ity for each resident which shall include:
(A) Admission information including theresident’s name; admission date; confiden-tiality number; previous address; birth date;sex; marital status; Social Security number;Medicare and Medicaid number; name,address and telephone number of physicianand alternate; name, address and telephonenumber of resident’s next of kin, legalguardian, designee or person to be notified in
22 CODE OF STATE REGULATIONS (4/30/09) ROBIN CARNAHAN
Secretary of State
19 CSR 30-86—DEPARTMENT OF HEALTH ANDSENIOR SERVICES Division 30—Division of Regulation and Licensure
case of emergency; and preferred dentist,pharmacist and funeral director; and III
(B) A resident’s record, including a reviewmonthly or more frequently, if indicated, ofthe resident’s general condition and needs; amonthly review of medication consumptionof any resident controlling his/her own medi-cation, noting if prescription medications arebeing used in appropriate quantities; a dailyrecord of distribution or administration ofmedication; any physician’s orders; a loggingof the drug regimen review process; a month-ly weight; a record of each referral of a resi-dent for services from an outside service; anda record of any patient incidents and acci-dents involving the resident. III
(59) A record of the resident census as wellas records regarding discharge, transfer ordeath of residents shall be kept in the facility.III
(60) Resident records shall be maintained bythe operator for at least five (5) years afterthe resident leaves the facility or after the res-ident reaches the age of twenty-one (21),whichever is longer. III
AUTHORITY: sections 198.005, 198.006 and198.073, RSMo Supp. 2006 and 198.076,RSMo 2000.* Original rule filed Aug. 23,2006, effective April 30, 2007.
*Original authority: 198.005, RSMo 2006; 198.006,RSMo 1979, amended 1984, 1987, 2003, 2006; and198.073, RSMo 1979, amended 1984, 1992, 1999, 2006.
19 CSR 30-86.045 Standards and Require-ments for Assisted Living Facilities WhichProvide Services to Residents with a Phys-ical, Cognitive, or Other Impairment thatPrevents the Individual from Safely Evacu-ating the Facility with Minimal Assistance
PURPOSE: This rule establishes the addi-tional standards for those assisted livingfacilities which provide services to residentswith a physical, cognitive, or other impair-ment that prevents the individual from safelyevacuating the facility with minimal assis-tance.
AGENCY NOTE: All rules relating tolong-term care facilities licensed by thedepartment are followed by a Roman Numer-al notation which refers to the class (eitherClass I, II or III) of standard as designated insection 198.085.1, RSMo.
(1) This rule contains the additional standardsfor those assisted living facilities licensedpursuant to sections 198.005 and 198.073,
RSMo (CCS HCS SCS SB 616, 93rd Gener-al Assembly, Second Regular Session (2006))and complying with sections 198.073.4 and198.073.6, RSMo (CCS HCS SCS SB 616,93rd General Assembly, Second Regular Ses-sion (2006)) and 19 CSR 30-86.047 thatchoose to admit or continue to care for anyindividual having a physical, cognitive orother impairment that prevents the individualfrom safely evacuating the facility with mini-mal assistance.
(2) Definitions. For the purposes of this rule,the following definitions shall apply:
(A) Area of refuge—A space located in orimmediately adjacent to a path of travel lead-ing to an exit that is protected from theeffects of fire, either by means of separationfrom other spaces in the same building or itslocation, permitting a delay in evacuation.An area of refuge may be temporarily used asa staging area that provides some relativesafety to its occupants while potential emer-gencies are assessed, decisions are made, andevacuation has begun;
(B) Evacuating the facility—The act of theresident going from one (1) smoke section toanother within the facility, going to an area ofrefuge within the facility, or going out of thefacility;
(C) Individualized evacuation plan—A planto remove the resident from the facility, to anarea of refuge within the facility or from one(1) smoke section to another within the facil-ity. The plan is specific to the resident’sneeds and abilities based on the current com-munity based assessment;
(D) Minimal assistance—1. Is the criterion which determines
whether or not staff must develop and includean individualized evacuation plan as part ofthe resident’s service plan;
2. Minimal assistance may be the verbalintervention that staff must provide for a res-ident to initiate evacuating the facility;
3. Minimal assistance may be the physi-cal intervention that staff must provide, suchas turning a resident in the correct direction,for a resident to initiate evacuating the facili-ty;
4. A resident needing minimal assis-tance is one who is able to prepare to leaveand then evacuate the facility within five (5)minutes of being alerted of the need to evac-uate and requires no more than one (1) phys-ical intervention and no more than three (3)verbal interventions of staff to complete evac-uation from the facility;
5. The following actions required ofstaff are considered to be more than minimalassistance:
A. Assistance to traverse down stair-
ways;B. Assistance to open a door; andC. Assistance to propel a wheelchair;
(E) Resident, only for the purpose of thisrule, means any individual having a physical,cognitive or other impairment that preventsthe individual from safely evacuating thefacility with minimal assistance who is admit-ted to or continues to be cared for in the facil-ity under the provisions of this rule; and
(F) Smoke section—A fire-rated separationof one (1) section of the building from therest of the building.
(3) General Requirements. I/II(A) If the facility admits or retains any
individual needing more than minimal assis-tance due to having a physical, cognitive orother impairment that prevents the individualfrom safely evacuating the facility, the facili-ty shall:
1. Meet the fire safety requirements of19 CSR 30-86.022(16); I/II
2. Take necessary measures to provideresidents with the opportunity to explore thefacility and, if appropriate, its grounds; II
3. Use a personal electronic monitoringdevice for any resident whose physician rec-ommends the use of such device; II
4. Have sufficient staff present andawake twenty-four (24) hours a day to assistin the evacuation of all residents; I/II
5. Include an individualized evacuationplan in the resident’s individual service plan;II
6. At a minimum the evacuation planshall include the following components:
A. The responsibilities of specificstaff positions in an emergency specific to theindividual; II
B. The fire protection interventionsneeded to ensure the safety of the resident;and II
C. The plan shall evaluate the residentfor his or her location within the facility andthe proximity to exits and areas of refuge.The plan shall evaluate the resident, as appli-cable, for his or her risk of resistance, mobil-ity, the need for additional staff support, con-sciousness, response to instructions, responseto alarms, and fire drills; II
7. The resident’s evacuation plan shallbe amended or revised based on the ongoingassessment of the needs of the resident; II
8. Those employees with specificresponsibilities shall be instructed andinformed regarding their duties and responsi-bilities under the resident’s evacuation plan atleast every six (6) months and upon any sig-nificant change in the plan; II
CODE OF STATE REGULATIONS 23ROBIN CARNAHAN (4/30/09)Secretary of State
Chapter 86—Residential Care Facilities and Assisted Living Facilities 19 CSR 30-86
9. A copy of the resident’s evacuationplan shall be readily available to all staff; andII
10. Comply with all requirements of thisrule. I/II
(4) Staffing Requirements.(A) The facility shall have an adequate
number and type of personnel for the propercare of residents and upkeep of the facility. Ata minimum, the staffing pattern for fire safe-ty and care of residents shall be one (1) staffperson for every fifteen (15) residents ormajor fraction of fifteen (15) during the dayshift, one (1) person for every fifteen (15)residents or major fraction of fifteen (15)during the evening shift, and one (1) personfor every twenty (20) residents or major frac-tion of twenty (20) during the night shift. I/II
Time Personnel Residents7 a.m. to 3 p.m.
(Day)* 1 3–153 p.m. to 9 p.m.
(Evening)* 1 3–159 p.m. to 7 a.m.
(Night)* 1 3–20
*If the shift hours vary from those indicated,the hours of the shifts shall show on the workschedules of the facility and shall not be lessthan six (6) hours. III
(B) The required staff shall be in the facil-ity awake, dressed, and prepared to assist res-idents in case of emergency. I/II
(C) The administrator shall count towardstaffing when physically present at the facili-ty. II
(D) These staffing requirements are appli-cable only when the facility actually has inresidence one (1) or more residents whorequire more than minimal assistance in evac-uating the facility. II
(E) At a minimum there shall be a licensednurse employed by the facility to work at leastthe following hours per week:
3–30 Residents—8 hours31–60 Residents—16 hours61–90 Residents—24 hours91 or more Residents—40 hours. II(F) The licensed nurse shall be available to
assess residents for pain and significant andacute changes in condition. The nurse’sduties shall include, but shall not be limitedto, review of residents’ records, medications,and special diets or other orders, review ofeach resident’s adjustment to the facility, andobservation of each individual resident’s gen-eral physical, psychosocial, and mental sta-tus. The nurse shall inform the administratorof any problems noted and these shall bebrought to the attention of the resident’s
physician and legally authorized representa-tive or designee. II/III
AUTHORITY: sections 198.073 and 198.076,RSMo Supp. 2007.* This rule originally filedas 13 CSR 15-15.045. Emergency rule filedDec. 14, 2000, effective Jan. 2, 2001, expiredJune 30, 2001. Original rule filed Dec. 14,2000, effective June 30, 2001. Moved to 19CSR 30-86.045, effective Aug. 28, 2001.Amended: Filed Aug. 23, 2006, effectiveApril 30, 2007. Amended: Filed March 13,2008, effective Oct. 30, 2008.
*Original authority: 198.073, RSMo 1979, amended1984, 1992, 1999, 2006, 2007 and 198.076, RSMo 1979,amended 1984, 2007.
19 CSR 30-86.047 Administrative, Person-nel and Resident Care Requirements forAssisted Living Facilities
PURPOSE: This rule establishes standardsfor all assisted living facilities licensed pur-suant to sections 198.005 and 198.073,RSMo (CCS HCS SCS SB 616, 93rd GeneralAssembly, Second Regular Session (2006))and required to meet assisted living facilitystandards pursuant to section 198.073.3,RSMo (CCS HCS SCS SB 616, 93rd GeneralAssembly, Second Regular Session (2006))and section 198.076, RSMo 2000.
PUBLISHER’S NOTE: The secretary of statehas determined that the publication of theentire text of the material which is incorpo-rated by reference as a portion of this rulewould be unduly cumbersome or expensive.This material as incorporated by reference inthis rule shall be maintained by the agency atits headquarters and shall be made availableto the public for inspection and copying at nomore than the actual cost of reproduction.This note applies only to the reference mate-rial. The entire text of the rule is printedhere.
AGENCY NOTE: All rules relating tolong-term care facilities licensed by thedepartment are followed by a Roman Numer-al notation which refers to the class (eitherClass I, II or III) of standard as designated insection 198.085.1, RSMo.
(1) Facilities licensed as assisted living facil-ities shall be inspected pursuant to the stan-dards outlined herein beginning April 1,2007. An assisted living facility may request,in writing to the department, to comply withthese standards prior to April 1, 2007. Uponreceipt of the request, the department shallconduct an inspection to determine compli-
ance with the standards outlined herein priorto issuing a license indicating such compli-ance.
(2) Consumer Education Requirements. Thefacility shall disclose to a prospective resi-dent, or legal representative of the resident,information regarding the services the facili-ty is able to provide or coordinate, the cost ofsuch services to the resident, and the groundsfor discharge or transfer as permitted orrequired by the Omnibus Nursing Home Act,Chapter 198, RSMo and the department’sregulations, including the provisions set forthin section (29) of this rule. II
(3) Nothing in this rule shall be construed toallow any facility that has not met the require-ments of 198.073(4) and (6), RSMo, (CCSHCS SCS SB 616, 93rd General Assembly,Second Regular Session (2006)) and 19 CSR30-86.045 to care for any individual with aphysical, cognitive or other impairment thatprevents the individual from safely evacuatingthe facility with minimal assistance. I/II
(4) Definitions. For the purpose of this rule,the following definitions shall apply:
(A) Appropriately trained and qualifiedindividual means an individual who islicensed or registered with the state of Mis-souri in a health care related field or an indi-vidual with a degree in a health care relatedfield or an individual with a degree in ahealth care, social services, or human ser-vices field or an individual licensed underChapter 344, RSMo, and who has receivedfacility orientation training under 19 CSR 30-86.042(18), and dementia training under sec-tion 660.050, RSMo, and twenty-four (24)hours of additional training, approved by thedepartment, consisting of definition andassessment of activities of daily living,assessment of cognitive ability, service plan-ning, and interview skills;
(B) Area of refuge—A space located in orimmediately adjacent to a path of travel lead-ing to an exit that is protected from theeffects of fire, either by means of separationfrom other spaces in the same building or itslocation, permitting a delay in evacuation.An area of refuge may be temporarily used asa staging area that provides relative safety toits occupants while potential emergencies areassessed, decisions are made, and evacuationis begun;
(C) Assisted living facility (ALF)—Is asdefined in 19 CSR 30-83.010;
(D) Chemical restraint—Is as defined in 19CSR 30-83.010;
24 CODE OF STATE REGULATIONS (4/30/09) ROBIN CARNAHAN
Secretary of State
19 CSR 30-86—DEPARTMENT OF HEALTH ANDSENIOR SERVICES Division 30—Division of Regulation and Licensure
(E) Community based assessment—Docu-mented basic information and analysis pro-vided by appropriately trained and qualifiedindividuals describing an individual’s abili-ties and needs in activities of daily living,instrumental activities of daily living,vision/hearing, nutrition, social participationand support, and cognitive functioning usingan assessment tool approved by the depart-ment, that is designed for community basedservices and that is not the nursing homeminimum data set. The assessment tool maybe one developed by the department or oneused by a facility which has been approved bythe department;
(F) Evacuating the facility—For the pur-pose of this rule, evacuating the facility shallmean moving to an area of refuge or from onesmoke section to another or exiting the facil-ity;
(G) Home-like—Means a self-containedlong-term care setting that integrates the psy-chosocial, organizational and environmentalqualities that are associated with being athome. Home-like may include, but is notlimited to the following:
1. A living room and common use areasfor social interactions and activities;
2. Kitchen and family style eating areafor use by the residents;
3. Laundry area for use by residents;4. A toilet room that contains a toilet,
lavatory and bathing unit in each resident’sroom;
5. Resident room preferences for resi-dents who wish to share a room, and for res-idents who wish to have private bedrooms;
6. Outdoor area for outdoor activitiesand recreation; and
7. A place where residents can give andreceive affection, explore their interests,exercise control over their environment,engage in interactions with others and haveprivacy, security, familiarity and a sense ofbelonging;
(H) Individualized service plan (ISP)—Shall mean the planning document preparedby an assisted living facility, which outlines aresident’s needs and preferences, services tobe provided, and the goals expected by theresident or the resident’s legal representativein partnership with the facility;
(I) Keeping residents in place—Meansmaintaining residents in place during a fire inlieu of evacuation where a building’s occu-pants are not capable of evacuation, whereevacuation has a low likelihood of success, orwhere it is recommended in writing by localfire officials as having a better likelihood ofsuccess and/or a lower risk of injury;
(J) Minimal assistance—
1. Is the criterion which determineswhether or not staff must develop and includean individualized evacuation plan as part ofthe resident’s service plan;
2. Minimal assistance may be the verbalintervention that staff must provide for a res-ident to initiate evacuating the facility;
3. Minimal assistance may be the physi-cal intervention that staff must provide, suchas turning a resident in the correct direction,for a resident to initiate evacuating the facili-ty;
4. A resident needing minimal assis-tance is one who is able to prepare to leaveand then evacuate the facility within five (5)minutes of being alerted of the need to evac-uate and requires no more than one (1) phys-ical intervention and no more than three (3)verbal interventions of staff to complete evac-uation from the facility;
5. The following actions required ofstaff are considered to be more than minimalassistance:
A. Assistance to traverse down stair-ways;
B. Assistance to open a door; andC. Assistance to propel a wheelchair;
(K) Physical restrain—Any manual methodor physical or mechanical device, material orequipment attached to or adjacent to the res-ident’s body that the individual cannotremove easily which restricts freedom ofmovement or normal access to one’s body.Physical restraints include, but are not limit-ed to leg restraints, arm restraints, handmitts, soft ties or vests, lap cushions and laptrays the resident cannot remove easily. Phys-ical restraints also include facility practicesthat meet the definition of a restraint, such asthe following:
1. Using side rails that keep a residentfrom voluntarily getting out of bed;
2. Tucking in or using Velcro to hold asheet, fabric or clothing tightly so that a res-ident’s movement is restricted;
3. Using devices in conjunction with achair, such as trays, tables, bars or belts, thatthe resident cannot remove easily, that pre-vent the resident from rising;
4. Placing the resident in a chair thatprevents a resident from rising; and
5. Placing a chair or bed so close to awall that the wall prevents the resident fromrising out of the chair or voluntarily gettingout of bed;
(L) Significant change—means any changein the resident’s physical, emotional or psy-chosocial condition or behavior that will notnormally resolve itself without further inter-vention by staff or by implementing standarddisease-related clinical interventions, that hasan impact on more than one (1) area of the
resident’s health status, and requires interdis-ciplinary review or revision of the individual-ized service plan, or both;
(M) Skilled nursing facility—Means anypremises, other than a residential care facili-ty, assisted living facility or an intermediatecare facility, which is utilized by its owner,operator or manager to provide for twenty-four (24) hour accommodation, board andskilled nursing care and treatment services toat least three (3) residents who are not relat-ed within the fourth degree of consanguinityor affinity to the owner, operator or managerof the facility. Skilled nursing care and treat-ment services are those services commonlyperformed by or under the supervision of aregistered professional nurse for individualsrequiring twenty-four (24)-hours-a-day careby licensed nursing personnel including actsof observation, care and counsel of the aged,ill, injured or infirm, the administration ofmedications and treatments as prescribed by alicensed physician or dentist, and other nurs-ing functions requiring substantial specializedjudgment and skill;
(N) Skilled nursing placement—Meansplacement in a skilled nursing facility asdefined in subsection (4)(M) of this rule; and
(O) Social model of care—Means long-term care services based on the abilities,desires, and functional needs of the individu-al delivered in a setting that is more home-like than institutional, that promote the digni-ty, individuality, privacy, independence andautonomy of the individual, that respects res-idents’ differences and promotes residents’choices.
(5) The operator shall designate an individu-al for administrator who is currently licensedas a nursing home administrator under Chap-ter 344, RSMo. II
(6) The operator shall be responsible toassure compliance with all applicable lawsand regulations. The administrator shall befully authorized and empowered to makedecisions regarding the operation of the facil-ity and shall be held responsible for theactions of all employees. The administrator’sresponsibilities shall include oversight of res-idents to assure that they receive care asdefined in the individualized service plan.II/III
(7) The administrator cannot be listed or func-tion in more than one (1) licensed facility atthe same time unless he or she serves no morethan five (5) facilities within a thirty (30)-mileradius and licensed to serve in total no morethan one hundred (100) residents, and theadministrator has an individual designated as
CODE OF STATE REGULATIONS 25ROBIN CARNAHAN (4/30/09)Secretary of State
Chapter 86—Residential Care Facilities and Assisted Living Facilities 19 CSR 30-86
the daily manager of each facility. However,the administrator may serve as the adminis-trator of more than one (1) licensed facility ifall facilities are on the same premises. II
(8) The administrator shall designate, in writ-ing, a staff member in charge in the adminis-trator’s absence. If the administrator is absentfor more than thirty (30) consecutive days,during which time he or she is not readilyaccessible for consultation by telephone withthe delegated individual, the individual desig-nated to be in charge shall be a currentlylicensed nursing home administrator. Suchthirty (30)-consecutive-day absences mayonly occur once within any consecutivetwelve (12)-month period. II/III
(9) The facility shall not care for more resi-dents than the number for which the facilityis licensed. However, if the facility operates anon-licensed adult day care program for four(4) or fewer participants within the licensedfacility, the day care participants shall not beincluded in the total facility census. Adultday care participants shall be counted instaffing determination during the hours theday care participants are in the facility. II/III
(10) The facility shall not admit or continueto care for residents whose needs cannot bemet. If necessary services cannot be obtainedin or by the facility, the resident shall bepromptly referred to appropriate outsideresources or discharged from the facility. I/II
(11) All personnel responsible for residentcare shall have access to the legal name ofeach resident, name and telephone number ofresident’s physician, resident’s designee orlegally authorized representative in the eventof emergency. II/III
(12) All persons who have any contact withthe residents in the facility shall not know-ingly act or omit any duty in a manner thatwould materially and adversely affect thehealth, safety, welfare or property of resi-dents. No person who is listed on the depart-ment’s Employee Disqualification List (EDL)shall work or volunteer in the facility in anycapacity whether or not employed by theoperator. For the purpose of this rule, a vol-unteer is an unpaid individual formally rec-ognized by the facility as providing a directcare service to residents. The facility isrequired to check the EDL for individualswho volunteer to perform a service for whichthe facility might otherwise have to hire anemployee. The facility is not required tocheck the EDL for individuals or groups suchas scout groups, bingo or sing-along leaders.
The facility is not required to check the EDLfor an individual such as a priest, minister orrabbi visiting a resident who is a member ofthe individual’s congregation. However, if aminister, priest or rabbi serves as a volunteerfacility chaplain, the facility is required tocheck to determine if the individual is listedon the EDL since the individual would havecontact with all residents. I/II
(13) Prior to allowing any person who hasbeen hired in a full-time, part-time, or tem-porary employee position to have contact withany residents, the facility shall, or in the caseof temporary employees hired through orcontracted from an employment agency, theemployment agency shall, prior to sending atemporary employee to a provider:
(A) Request a criminal background checkfor the person, as provided in section 43.540,RSMo. Each facility must maintain in itsrecord documents verifying that the back-ground checks were requested and the natureof the response received for each suchrequest.
1. The facility must ensure that anyapplicant or person hired or retained who dis-closes prior to the receipt of the criminalbackground check that he/she has been con-victed of, pled guilty or pled nolo contendereto in this state or any other state or has beenfound guilty of a crime, which if committedin Missouri would be a Class A or B felonyviolation of Chapter 565, 566, or 569, RSMoor any violation of subsection 198.070.3,RSMo or of section 568.020, RSMo, will nothave contact with residents. II/III
2. Upon receipt of the criminal back-ground check, the facility must ensure that ifthe criminal background check indicates thatthe person hired or retained by the facility hasbeen convicted of, pled guilty or pled nolocontendere to in this state or any other stateor has been found guilty of a crime, which ifcommitted in Missouri would be a Class A orB felony violation of Chapter 565, 566, or569, RSMo or any violation of subsection198.070.3, RSMo or of section 568.020,RSMo, the person will not have contact withresidents unless the facility obtains verifica-tion from the department that a good causewaiver has been granted and maintains a copyof the verification in the individual’s person-nel file. II/III
(B) Make an inquiry to the department,whether the person is listed on the employeedisqualification list as provided in section660.315, RSMo. The inquiry may be madevia Internet at www.dhss.mo.gov/EDL/.II/III
(C) If the person has registered with thedepartment’s Family Care Safety Registry
(FCSR), the facility may utilize the Registryin order to meet the requirements of subsec-tions (13)(A) and (13)(B) of this rule. TheFCSR is available via Internet atwww.dhss.mo.gov/FCSR/Background-Check.html. II/III
(D) For persons for whom the facility hascontracted for professional services (e.g.,plumbing or air conditioning repair) that willhave contact with any resident, the facilitymust either require a criminal backgroundcheck or ensure that the individual is suffi-ciently monitored by facility staff while in thefacility to reasonably ensure the safety of allresidents. I/II
(14) A facility shall not employ, as an agentor employee who has access to controlledsubstances, any person who has been foundguilty or entered a plea of guilty or nolo con-tendere in a criminal prosecution under thelaws of any state or of the United States forany offense related to controlled substances.II
(A) A facility may apply in writing to thedepartment for a waiver of this section of thisrule for a specific employee.
(B) The department may issue a writtenwaiver to a facility upon determination that awaiver would be consistent with the publichealth and safety. In making this determina-tion, the department shall consider the dutiesof the employee, the circumstances surround-ing the conviction, the length of time sincethe conviction was entered, whether a waiverhas been granted by the department’s Bureauof Narcotics and Dangerous Drugs pursuantto 19 CSR 30-1.034 when the facility is reg-istered with that agency, whether a waiver hasbeen granted by the federal Drug Enforce-ment Administration (DEA) pursuant to 21CFR 1301.76 when the facility is also regis-tered with that agency, the security measurestaken by the facility to prevent the theft anddiversion of controlled substances, and anyother factors consistent with public healthand safety. II
(15) The facility must develop and implementwritten policies and procedures which requirethat persons hired for any position which is tohave contact with any patient or resident havebeen informed of their responsibility to dis-close their prior criminal history to the facil-ity as required by section 660.317.5, RSMo.The facility must also develop and implementpolicies and procedures which ensure that thefacility does not knowingly hire, after August28, 1997, any person who has or may havecontact with a patient or resident, who hasbeen convicted of, plead guilty or nolo con-tendere to, in this state or any other state, or
26 CODE OF STATE REGULATIONS (4/30/09) ROBIN CARNAHAN
Secretary of State
19 CSR 30-86—DEPARTMENT OF HEALTH ANDSENIOR SERVICES Division 30—Division of Regulation and Licensure
has been found guilty of any Class A or Bfelony violation of Chapter 565, 566 or 569,RSMo, or any violation of subsection 3 ofsection 198.070, RSMo, or of section568.020, RSMo. II/III
(16) All persons who have or may have con-tact with residents shall at all times when onduty or delivering services wear an identifi-cation badge. The badge shall give theirname, title and, if applicable, the status oftheir license or certification as any kind ofhealth care professional. This rule shall applyto all personnel who provide services to anyresident directly or indirectly. III
(17) Personnel who have been diagnosed witha communicable disease may begin work orreturn to duty only with written approval by aphysician or physician’s designee, whichindicates any limitations. II
(18) The administrator shall be responsible toprevent an employee known to be diagnosedwith communicable disease from exposingresidents to such disease. The facility’s poli-cies and procedures must comply with thedepartment’s regulations pertaining to com-municable diseases, specifically 19 CSR 20-20.010 through 19 CSR 20-20.100. II /III
(19) The facility shall screen residents andstaff for tuberculosis as required for long-term care facilities by 19 CSR 20-20.100. II
(20) The administrator shall maintain on thepremises an individual personnel record oneach facility employee, which shall includethe following:
(A) The employee’s name and address;(B) Social Security number; (C) Date of birth;(D) Date of employment;(E) Documentation of experience and edu-
cation including for positions requiring licen-sure or certification, documentation evidenc-ing competency for the position held, whichincludes copies of current licenses, tran-scripts when applicable, or for those individ-uals requiring certification, such as certifiedmedication technicians, level I medicationaides and insulin administration aides; print-ing the Web Registry search results pageavailable at www.dhss.mo.gov/cnaregistryshall meet the requirements of the employer’scheck regarding valid certification;
(F) References, if available;(G) The results of background checks
required by section 660.317, RSMo; and acopy of any good cause waiver granted by thedepartment, if applicable;
(H) Position in the facility;(I) Written statement signed by a licensed
physician or physician’s designee indicatingthe person can work in a long-term care facil-ity and indicating any limitations;
(J) Documentation of the employee’s tuber-culin screening status;
(K) Documentation of what the employeewas instructed on during orientation training;and
(L) Reason for termination if the employeewas terminated due to abuse or neglect of aresident, residents’ rights issues or residentinjury. III
(21) Personnel records shall be maintainedfor at least two (2) years following termina-tion of employment. III
(22) There shall be written documentationmaintained in the facility showing actualhours worked by each employee. III
(23) No one individual shall be on duty withresponsibility for oversight of residents longerthan eighteen (18) hours per day. I/II
(24) Employees who are counted in meetingthe minimum staffing ratio and employeeswho provide direct care to the residents shallbe at least sixteen (16) years of age. Oneemployee at least eighteen (18) years of ageshall be on duty at all times. II
(25) Each facility resident shall be under themedical supervision of a physician licensed topractice in Missouri who has been informedof the facility’s emergency medical proce-dures and is kept informed of treatments ormedications prescribed by any other profes-sional lawfully authorized to prescribe medi-cations. III
(26) The facility shall ensure that each resi-dent being admitted or readmitted to the facil-ity receives an admission physical examina-tion by a licensed physician. The facilityshall request documentation of the physicalexamination prior to admission but must havedocumentation of the physical examination onfile no later than ten (10) days after admis-sion. The physical examination shall containdocumentation regarding the individual’s cur-rent medical status and any special orders orprocedures to be followed. If the resident isadmitted directly from an acute care oranother long-term care facility and is accom-panied on admission by a report that reflectshis or her current medical status, an admis-sion physical shall not be required. III
(27) Residents under sixteen (16) years of ageshall not be admitted. III
(28) The facility may admit or retain an indi-vidual for residency in an assisted living facil-ity only if the individual does not require hos-pitalization or skilled nursing placement asdefined in this rule, and only if the facility:
(A) Provides for or coordinates oversightand services to meet the needs, the social andrecreational preferences in accordance withthe individualized service plan of the residentas documented in a written contract signed bythe resident, or legal representative of theresident; II
(B) Has twenty-four (24) hour staff appro-priate in numbers and with appropriate skillsto provide such services; II
(C) Has a written plan for the protection ofall residents in the event of a disaster such astornado, fire, bomb threat or severe weather,including:
1. Keeping residents in place;2. Evacuating residents to areas of
refuge;3. Evacuating residents from the build-
ing if necessary; or4. Other methods of protection based on
the disaster and the individual buildingdesign; I/II
(D) Completes a premove-in screeningconducted as required by section 198.073.4(4), RSMo (CCS HCS SCS SB 616, 93rdGeneral Assembly, Second Regular Session(2006)). II
(E) The premove-in screening shall becompleted prior to admission with the partic-ipation of the prospective resident and bedesigned to determine if the individual is eli-gible for admission to the assisted livingfacility and shall be based on the admissionrestrictions listed at section (29) of this rule;II
(F) Completes a community based assess-ment conducted by an appropriately trainedand qualified individual as defined in section(4) of this rule:
1. Time frame requirements for assess-ment shall be:
A. Within five (5) calendar days ofadmission; II
B. At least semiannually; and IIC. Whenever a significant change has
occurred in the resident’s condition, whichmay require a change in services. II
2. The facility shall use form MO 580-2835, Assessment for Admission To Assist-ed Living Facilities, (9-06), incorporated byreference, provided by the Department ofHealth and Senior Services, PO Box 570, Jef-ferson City, MO 65102-0570 and which isavailable to long-term care facilities atwww.dhss.mo.gov or by telephone at (573)526-8548. This rule does not incorporate anysubsequent amendments or additions; or II
CODE OF STATE REGULATIONS 27ROBIN CARNAHAN (4/30/09)Secretary of State
Chapter 86—Residential Care Facilities and Assisted Living Facilities 19 CSR 30-86
3. The facility may use another assess-ment form if approved in advance by thedepartment; II
(G) Develops an individualized serviceplan (ISP), which means the planning docu-ment prepared by an assisted living facilitywhich outlines a resident’s needs and prefer-ences, services to be provided, and goalsexpected by the resident or the resident’slegal representative in partnership with thefacility; II
(H) Reviews the ISP with the resident, orlegal representative of the resident, at leastannually or when there is a significant changein the resident’s condition which may requirea change in services; II
(I) Includes the signatures of an authorizedrepresentative of the facility and the residentor the resident’s legal representative in theindividualized service plan to acknowledgethat the service plan has been reviewed andunderstood by the resident or legal represen-tative; II
(J) Develops and implements a plan to pro-tect the rights, privacy, and safety of all resi-dents and to protect against the financialexploitation of all residents; and II
(K) Complies with the dementia specifictraining requirements of subsection 8 of sec-tion 660.050, RSMo. II
(29) The facility shall not admit or continueto care for a resident who:
(A) Has exhibited behaviors that present areasonable likelihood of serious harm to him-self or herself or others; I/II
(B) Requires physical restraint as definedin this rule; II
(C) Requires chemical restraint as definedin this rule; II
(D) Requires skilled nursing services asdefined in section 198.073.4, RSMo forwhich the facility is not licensed or able toprovide; II
(E) Requires more than one (1) person tosimultaneously physically assist the residentwith any activity of daily living, with theexception of bathing and transferring; orII/III
(F) Is bed-bound or similarly immobilizeddue to a debilitating or chronic condition. II
(30) The requirements of subsections(29)(D), (E) and (F) shall not apply to a res-ident receiving hospice care, provided theresident, his or her legally authorized repre-sentative or designee, or both, and the facili-ty, physician and licensed hospice provider allagree that such program of care is appropri-ate for the resident. II
(31) Programs and Services Requirements forResidents.
(A) The facility shall designate a staffmember to be responsible for leisure activitycoordination and for promoting the socialmodel, multiple staff role directing all staff toprovide routine care in a manner that empha-sizes the opportunity for the resident and thestaff member to enjoy a visit rather than sim-ply perform a procedure. II/III
(B) The facility shall make available andimplement self-care, productive and leisureactivity programs which maximize andencourage the resident’s optimal functionalability for residents. The facility shall pro-vide person-centered activities appropriate tothe resident’s individual needs, preferences,background and culture. Individual or groupactivity programs may consist of the follow-ing:
1. Gross motor activities, such as exer-cise, dancing, gardening, cooking and otherroutine tasks;
2. Self-care activities, such as dressing,grooming and personal hygiene;
3. Social and leisure activities, such asgames, music and reminiscing;
4. Sensory enhancement activities, suchas auditory, olfactory, visual and tactile stim-ulation;
5. Outdoor activities, such as walkingand field trips;
6. Creative arts; or 7. Other social, leisure or therapeutic
activities that encourage mental and physicalstimulation or enhance the resident’s well-being. II/III
(C) Staff shall inform residents in advanceof any organized group activity including thetime and place of the activity. II/III
(32) Requirements for Facilities ProvidingCare to Residents Having Mental Illness orMental Retardation Diagnosis.
(A) Each resident who exhibits mental andpsychosocial adjustment difficulty(ies) shallreceive treatment and services to address theresident’s needs and behaviors as stated in theindividualized service plan. I/II
(B) If specialized rehabilitative services formental illness or mental retardation arerequired to enable a resident to reach and tocomply with the individualized service plan,the facility shall ensure the required servicesare provided. II
(C) The facility shall maintain in the resi-dent’s record the most recent progress notesand personal plan developed and provided bythe Department of Mental Health or desig-nated administrative agent for each residentwhose care is funded by the Department of
Mental Health or designated administrativeagent. III
(33) No facility shall accept any individualwith a physical, cognitive, or other impair-ment that prevents the individual from safelyevacuating the facility with minimal assis-tance unless the facility meets all require-ments of section 198.073, RSMo (CCS HCSSCS SB 616, 93rd General Assembly, Sec-ond Regular Session (2006)) and those stan-dards set forth in 19 CSR 30-86.045. I/II
(34) The facility shall follow appropriateinfection control procedures. The administra-tor or his or her designee shall make a reportto the local health authority or the departmentof the presence or suspected presence of anydiseases or findings listed in 19 CSR 20-20.020, sections (1)–(3) according to thespecified time frames as follows:
(A) Category I diseases or findings shall bereported to the local health authority or to thedepartment within twenty-four (24) hours offirst knowledge or suspicion by telephone,facsimile, or other rapid communication;
(B) Category II diseases or findings shallbe reported to the local health authority orthe department within three (3) days of firstknowledge or suspicion;
(C) Category III—The occurrence of anoutbreak or epidemic of any illness, diseaseor condition which may be of public healthconcern, including any illness in a food han-dler that is potentially transmissible throughfood. This also includes public health threatssuch as clusters of unusual diseases or mani-festations of illness and clusters of unex-plained deaths. Such incidents shall bereported to the local authority or to thedepartment by telephone, facsimile, or otherrapid communication within twenty-four (24)hours of first knowledge or suspicion. I/II
(35) Protective oversight shall be providedtwenty-four (24) hours a day. For residentsdeparting the premises on voluntary leave,the facility shall have, at a minimum, a pro-cedure to inquire of the resident or resident’sguardian of the resident’s departure, of theresident’s estimated length of absence fromthe facility, and of the resident’s whereaboutswhile on voluntary leave. I/II
(36) Residents shall receive proper care asdefined in the individualized service plan.I/II
(37) In case of behaviors that present a rea-sonable likelihood of serious harm to himselfor herself or others, serious illness, signifi-cant change in condition, injury or death,
28 CODE OF STATE REGULATIONS (4/30/09) ROBIN CARNAHAN
Secretary of State
19 CSR 30-86—DEPARTMENT OF HEALTH ANDSENIOR SERVICES Division 30—Division of Regulation and Licensure
staff shall take appropriate action and shallpromptly attempt to contact the person listedin the resident’s record as the legally autho-rized representative, designee or placementauthority. The facility shall contact theattending physician or designee and notify thelocal coroner or medical examiner immedi-ately upon the death of any resident of thefacility prior to transferring the deceased res-ident to a funeral home. I/II
(38) The facility shall encourage and assisteach resident based on his or her individualpreferences and needs to be clean and free ofbody and mouth odor. II
(39) If the resident brings unsealed medica-tions to the facility, the medications shall notbe used unless a pharmacist, physician ornurse examines, identifies and determines thecontents to be suitable for use. The personperforming the identification shall documenthis or her review. II/III
(40) Self-control of prescription medicationby a resident may be allowed only if approvedin writing by the resident’s physician andincluded in the resident’s individualized ser-vice plan. A resident may be permitted tocontrol the storage and use of nonprescriptionmedication unless there is a physician’s writ-ten order or facility policy to the contrary.Written approval for self-control of prescrip-tion medication shall be rewritten as neededbut at least annually and after any period ofhospitalization. II/III
(41) All medication shall be safely stored atproper temperature and shall be kept in asecured location behind at least one (1)locked door or cabinet. Medication shall beaccessible only to persons authorized toadminister medications. II/III
(A) If access is controlled by the resident,a secured location shall mean in a lockedcontainer, a locked drawer in a bedside tableor dresser or in a resident’s private room iflocked in his or her absence, although thisdoes not preclude access by a responsibleemployee of the facility.
(B) Schedule II controlled substances shallbe stored in locked compartments separatefrom non-controlled medications, except thatsingle doses of Schedule II controlled sub-stances may be controlled by a resident incompliance with the requirements for self-control of medication of this rule.
(C) Medication that is not in current useand is not destroyed shall be stored separate-ly from medication that is in current use.II/III
(42) All prescription medications shall besupplied as individual prescriptions exceptwhere an emergency medication supply isallowed. All medications, including over-the-counter medications, shall be packaged andlabeled in accordance with applicable profes-sional pharmacy standards, and state and fed-eral drug laws. Labeling shall include acces-sory and cautionary instructions as well asthe expiration date, when applicable, and thename of the medication as specified in thephysician’s order. Medication labels shall notbe altered by facility staff and medicationsshall not be repackaged by facility staff exceptas allowed by section (43) of this rule. Over-the-counter medications for individual resi-dents shall be labeled with at least the resi-dent’s name. II/III
(43) Controlled substances and other pre-scription and non-prescription medicationsfor administration when a resident temporar-ily leaves a facility shall be provided as fol-lows:
(A) Separate containers of medications forthe leave period may be prepared by the phar-macy. The facility shall have a policy andprocedure for families to provide adequateadvance notice so that medications can beobtained from the pharmacy.
(B) Prescription medication cards or othermultiple-dose prescription containers current-ly in use in the facility may be provided byany authorized facility medication staff mem-ber if the containers are labeled by the phar-macy with complete pharmacy prescriptionlabeling for use. Original manufacturer con-tainers of non-prescription medications,along with instructions for administration,may be provided by any authorized facilitymedication staff member.
(C) When medications are supplied by thepharmacy in customized patient medicationpackages that allow separation of individualdose containers, the required number of con-tainers may be provided by any authorizedfacility medication staff member. The indi-vidual dose containers shall be placed in anouter container that is labeled with the nameand address of the facility and the date.
(D) When multiple doses of a medicationare required and it is not reasonably possibleto obtain prescription medication labeled bythe pharmacy, and it is not appropriate tosend a container of medication currently inuse in the facility, up to a twenty-four (24)-hour supply of each prescription or non-pre-scription medication may be provided by alicensed nurse in United States Pharmacopeia(USP) approved containers labeled with thefacility name and address, resident’s name,medication name and strength, quantity,
instructions for use, date, initials of individu-al providing, and other appropriate informa-tion.
(E) When no more than a single dose of amedication is required, any authorized facili-ty medication staff member may prepare thedose as for in-facility administration in a USPapproved container labeled with the facilityname and address, resident’s name, medica-tion name and strength, quantity, instructionsfor use, date, initials of person providing, andother appropriate information.
(F) The facility may have a policy that lim-its the quantity of medication sent with a res-ident without prior approval of the prescriber.
(G) Returned containers shall be identifiedas having been sent with the resident, andshall not later be returned to the pharmacy forreuse.
(H) The facility shall maintain accuraterecords of medications provided to andreturned by the resident. II/III
(44) Upon discharge or transfer of a resident,the facility shall release prescription medica-tions, including controlled substances, heldby the facility for the resident when the physi-cian writes an order for each medication to bereleased. Medications shall be labeled by thepharmacy with current instructions for use.Prescription medication cards or other con-tainers may be released if the containers arelabeled by the pharmacy with complete phar-macy prescription labeling. II/III
(45) Injections shall be administered only bya physician or licensed nurse, except thatinsulin injections may also be administeredby a certified medication technician or level Imedication aide who has successfully com-pleted the state-approved course for insulinadministration, taught by a department-approved instructor. Anyone trained prior toDecember 31, 1990, who completed thestate-approved insulin administration coursetaught by an approved instructor shall be con-sidered qualified to administer insulin in anassisted living facility. A resident whorequires insulin, may administer his or herown insulin if approved in writing by the res-ident’s physician and trained to do so by alicensed nurse or physician. The facility shallmonitor the resident’s condition and ability tocontinue self-administration. I/II
(46) The administrator shall develop andimplement a safe and effective system of med-ication control and use, which assures that allresidents’ medications are administered bypersonnel at least eighteen (18) years of age,in accordance with physicians’ instructionsusing acceptable nursing techniques. The
CODE OF STATE REGULATIONS 29ROBIN CARNAHAN (4/30/09)Secretary of State
Chapter 86—Residential Care Facilities and Assisted Living Facilities 19 CSR 30-86
facility shall employ a licensed nurse eight (8)hours per week for every thirty (30) residentsto monitor each resident’s condition and med-ication. Administration of medication shallmean delivering to a resident his or her pre-scription medication either in the originalpharmacy container, or for internal medica-tion, removing an individual dose from thepharmacy container and placing it in a smallcup container or liquid medium for the resi-dent to remove from the container and self-administer. External prescription medicationmay be applied by facility personnel if theresident is unable to do so and the resident’sphysician so authorizes. All individuals whoadminister medication shall be trained inmedication administration and, if not a physi-cian or a licensed nurse, shall be a certifiedmedication technician or level I medicationaide. I/II
(47) Medication Orders.(A) No medication, treatment or diet shall
be administered without an order from anindividual lawfully authorized to prescribesuch and the order shall be followed. II/III
(B) Physician’s written and signed ordersshall include: name of medication, dosage,frequency and route of administration and theorders shall be renewed at least every three(3) months. Computer generated signaturesmay be used if safeguards are in place to pre-vent their misuse. Computer identificationcodes shall be accessible to and used by onlythe individuals whose signatures they repre-sent. Orders that include optional doses orinclude pro re nata (PRN) administration fre-quencies shall specify a maximum frequencyand the reason for administration. II/III
(C) Telephone and other verbal ordersshall be received only by a licensed nurse,certified medication technician, level I medi-cation aide or pharmacist, and shall be imme-diately reduced to writing and signed by thatindividual. A certified medication technicianor level I medication aide may receive a tele-phone or other verbal order only for a medi-cation or treatment that the technician or levelI medication aide is authorized to administer.If a telephone or other verbal order is givento a medication technician or level I medica-tion aide, an initial dosage shall not beadministered until the order has beenreviewed by telephone, facsimile or in personby a licensed nurse or pharmacist. Thereview shall be documented by the reviewerco-signing the telephone or other verbalorder. II
(D) The review shall be documented by thelicensed nurse’s or pharmacist’s signaturewithin seven (7) days. III
(E) The facility shall submit to the physi-cian written versions of any oral or telephoneorders within four (4) days of the giving ofthe oral or telephone order. III
(F) Influenza and pneumococcal polysac-charide immunizations may be administeredper physician-approved facility policy afterassessment for contraindications—
1. The facility shall develop a policy thatprovides recommendations and assessmentparameters for the administration of suchimmunizations. The policy shall be approvedby the facility medical director for facilitieshaving a medical director, or by each resi-dent’s attending physician for facilities thatdo not have a medical director, and shallinclude the requirements to:
A. Provide education to each residentor the resident’s designee or legally autho-rized representative regarding the potentialbenefits and side effects of the immunization;II/III
B. Offer the immunization to the res-ident or obtain permission from the resident’sdesignee or legally authorized representativewhen the immunization is medically indicat-ed unless the resident has already beenimmunized as recommended by the policy;II/III
C. Provide the opportunity to refusethe immunization; and II/III
D. Perform an assessment for con-traindications; II/III
2. The assessment for contraindicationsand documentation of the education andopportunity to refuse the immunization shallbe dated and signed by the nurse performingthe assessment and placed in the medicalrecord; or
3. The facility shall with the approval ofeach resident’s physician, access screeningand immunization through outside sourcessuch as county or city health departments.II/III
(G) The administration of medication shallbe recorded on a medication sheet or directlyin the resident’s record and, if recorded on amedication sheet, shall be made part of theresident’s record. The administration shall berecorded by the same individual who pre-pares the medication and administers it.II/III
(48) The facility may keep an emergencymedication supply if approved by a pharma-cist or physician. Storage and use of medica-tions in the emergency medication supplyshall assure accountability. When the emer-gency medication supply contains controlledsubstances, the facility shall be registeredwith the Bureau of Narcotics and DangerousDrugs (BNDD) and shall be in compliance
with 19 CSR 30-1.052 and other applicablestate and federal controlled substance lawsand regulations. II/III
(49) Automated dispensing systems may becontrolled by the facility or may be controlledon-site or remotely by a pharmacy.
(A) Automated dispensing systems may beused for an emergency medication supply.
(B) Automated dispensing systems that arecontrolled by a pharmacy may be used forcontinuing doses of controlled substance andnon-controlled substance medications. Whencontinuing doses are administered from anautomated dispensing system that is con-trolled by a pharmacy, a pharmacist shallreview and approve each new medicationorder prior to releasing the medication fromthe system. The pharmacy and the facilitymay have a policy and procedure to allow therelease of initial doses of approved medica-tions when a pharmacist is not available inlieu of a separate emergency medication sup-ply. When initial doses are used when apharmacist is not available, a pharmacist shallreview and approve the order within twenty-four (24) hours of administration of the firstdose.
(C) Automated dispensing systems shall beused in compliance with state and federallaws and regulations. When an automateddispensing system controlled by the facilitycontains controlled substances for an emer-gency medication supply, the facility shall beregistered with the BNDD. When an auto-mated dispensing system is controlled by apharmacy, the facility shall use it in compli-ance with 20 CSR 2220-2.900. II/III
(50) Stock supplies of nonprescription medi-cation may be kept when specific medicationsare approved in writing by a consulting physi-cian, a registered nurse or a pharmacist. II/III
(51) Records shall be maintained upon receiptand disposition of all controlled substancesand shall be maintained separately from otherrecords, for two (2) years.
(A) Inventories of controlled substancesshall be reconciled as follows:
1. Controlled Substance Schedule IImedications shall be reconciled each shift;and II
2. Controlled Substance Schedule III–Vmedications shall be reconciled at least week-ly and as needed to ensure accountability. II
(B) Inventories of controlled substancesshall be reconciled by the following:
1. Two (2) medication personnel, one ofwhom is a licensed nurse; or
2. Two (2) medication personnel, whoare certified medication technicians or level I
30 CODE OF STATE REGULATIONS (4/30/09) ROBIN CARNAHAN
Secretary of State
19 CSR 30-86—DEPARTMENT OF HEALTH ANDSENIOR SERVICES Division 30—Division of Regulation and Licensure
CODE OF STATE REGULATIONS 31ROBIN CARNAHAN (4/30/09)Secretary of State
Chapter 86—Residential Care Facilities and Assisted Living Facilities 19 CSR 30-86
medication aides, when a licensed nurse isnot available. II
(C) Receipt records shall include the date,source of supply, resident name and prescrip-tion number when applicable, medicationname and strength, quantity and signature ofthe supplier and receiver. Administrationrecords shall include the date, time, residentname, medication name, dose administeredand the initials of the individual administer-ing. The signature and initials of each medi-cation staff documenting on the medicationadministration record must be signed in thesignature area of the medication record. II
(D) When self-control of medication isapproved a record shall be made of all con-trolled substances transferred to and adminis-tered from the resident’s room. Inventoryreconciliation shall include controlled sub-stances transferred to the resident’s room. II
(52) Documentation of waste of controlledsubstances at the time of administration shallinclude the reason for the waste and the sig-nature of another facility medication staffmember who witnesses the waste. If a sec-ond medication staff member is not availableat the time of administration, the controlledsubstance shall be properly labeled, clearlyidentified as unusable, stored in a lockedarea, and destroyed as soon as a medicationstaff member is available to witness thewaste. When a second medication staff mem-ber is not available and the controlled sub-stance is contaminated by patient body fluids,the controlled substance shall be destroyedimmediately and the circumstances docu-mented. II/III
(53) At least every other month, a pharmacistor registered nurse shall review the controlledsubstance record keeping including reconcil-ing the inventories of controlled substances.This shall be done at the time of the drug reg-imen review of each resident. All discrepan-cies in controlled substance records shall bereported to the administrator for review andinvestigation. The theft or loss of controlledsubstances shall be reported as follows:
(A) The facility shall notify the depart-ment’s Section for Long Term Care (SLTC)and other appropriate authorities of any theftor significant loss of any controlled substancemedication written as an individual prescrip-tion for a specific resident upon the discoveryof the theft or loss. The facility shall consid-er at least the following factors in determin-ing if a loss is significant:
1. The actual quantity lost in relation tothe total quantity;
2. The specific controlled substancelost;
3. Whether the loss can be associatedwith access by specific individuals;
4. Whether there is a pattern of losses,and if the losses appear to be random or not;
5. Whether the controlled substance is alikely candidate for diversion; and
6. Local trends and other indicators ofdiversion potential;
(B) If an insignificant amount of such con-trolled substance is lost during lawful activi-ties, which includes but are not limited toreceiving, record keeping, access auditing,administration, destruction and returning tothe pharmacy, a description of the occurrenceshall be documented in writing and main-tained with the facility’s controlled substancerecords. The documentation shall include thereason for determining that the loss wasinsignificant; and
(C) When the facility is registered with theBNDD, the facility shall report to or docu-ment for the BNDD any loss of any stocksupply controlled substance in compliancewith 19 CSR 30-1.034. II/III
(54) A physician, pharmacist or registerednurse shall review the medication regimen ofeach resident. This shall be done at leastevery other month. The review shall be per-formed in the facility and shall include, butshall not be limited to, indication for use,dose, possible medication interactions andmedication/food interactions, contraindica-tions, adverse reactions and a review of themedication system utilized by the facility.Irregularities and concerns shall be reportedin writing to the resident’s physician and tothe administrator/manager. If after thirty (30)days, there is no action taken by a resident’sphysician and significant concerns continueregarding a resident’s or residents’ medica-tion order(s), the administrator shall contactor recontact the physician to determine if heor she received the information and if thereare any new instructions. II/III
(55) All medication errors and adverse reac-tions shall be promptly documented andreported to the administrator and the resi-dent’s physician. If the pharmacy made a dis-pensing error, it shall also be reported to theissuing pharmacy. II/III
(56) Medications that are not in current useshall be disposed of as follows:
(A) Single doses of contaminated, refused,or otherwise unusable non-controlled sub-stance medications may be destroyed by anyauthorized medication staff member at thetime of administration. Single doses of unus-able controlled substance medications may be
destroyed according to section (52) of thisrule;
(B) Discontinued medications may beretained up to one hundred twenty (120) daysprior to other disposition if there is reason tobelieve, based on clinical assessment of theresident, that the medication might bereordered;
(C) Medications may be released to theresident or family upon discharge accordingto section (44) of this rule;
(D) After a resident has expired, medica-tions, except for controlled substances, maybe released to the resident’s legal representa-tive upon written request of the legal repre-sentative that includes the name of the medi-cation and the reason for the request;
(E) Medications may be returned to thepharmacy that dispensed the medications pur-suant to 20 CSR 2220-3.040 or returned pur-suant to the Prescription Drug RepositoryProgram, 19 CSR 20-50.020. All other med-ications, including all controlled substancesand all expired or otherwise unusable medi-cations, shall be destroyed within thirty (30)days as follows:
1. Medications shall be destroyed withinthe facility by a pharmacist and a licensednurse or by two (2) licensed nurses or whentwo (2) licensed nurses are not available onstaff by two (2) individuals who have author-ity to administer medications, one (1) ofwhom shall be a licensed nurse or a pharma-cist; and
2. A record of medication destroyedshall be maintained and shall include the res-ident’s name, date, medication name andstrength, quantity, prescription number, andsignatures of the individuals destroying themedications; and
(F) A record of medication released orreturned to the pharmacy shall be maintainedand shall include the resident’s name, date,medication name and strength, quantity, pre-scription number, and signatures of the indi-viduals releasing and receiving the medica-tions. II/III
(57) Residents experiencing short periods ofincapacity due to illness or injury or recuper-ation from surgery may be allowed to remainor be readmitted from a hospital if the periodof incapacity does not exceed forty-five (45)days and written approval of a physician isobtained for the resident to remain in or bereadmitted to the facility. II
(58) The facility shall maintain a record inthe facility for each resident, which shallinclude the following:
(A) Admission information including theresident’s name; admission date; confiden-tiality number; previous address; birth date;sex; marital status; Social Security number;Medicare and Medicaid numbers (if applica-ble); name, address and telephone number ofthe resident’s physician and alternate; diagno-sis, name, address and telephone number ofthe resident’s legally authorized representa-tive or designee to be notified in case ofemergency; and preferred dentist, pharmacistand funeral director; III
(B) A review monthly or more frequently,if indicated, of the resident’s general condi-tion and needs; a monthly review of medica-tion consumption of any resident controllinghis or her own medication, noting if pre-scription medications are being used inappropriate quantities; a daily record ofadministration of medication; a logging of themedication regimen review process; a month-ly weight; a record of each referral of a resi-dent for services from an outside service; anda record of any resident incidents includingbehaviors that present a reasonable likelihoodof serious harm to himself or herself or oth-ers and accidents that potentially could resultin injury or did result in injuries involving theresident; and
(C) Any physician’s orders. The facilityshall submit to the physician written versionsof any oral or telephone orders within four(4) days of the giving of the oral or telephoneorder. III
(59) A record of the resident census shall beretained in the facility. III
(60) Resident records shall be maintained bythe operator for at least five (5) years after aresident leaves the facility or after the resi-dent reaches the age of twenty-one (21),whichever is longer and must include reasonfor discharge or transfer from the facility andcause of death, as applicable. III
(61) Staffing Requirements.(A) The facility shall have an adequate
number and type of personnel for the propercare of residents, the residents’ social wellbeing, protective oversight of residents andupkeep of the facility. At a minimum, thestaffing pattern for fire safety and care of res-idents shall be one (1) staff person for everyfifteen (15) residents or major fraction of fif-teen (15) during the day shift, one (1) personfor every twenty (20) residents or major frac-tion of twenty (20) during the evening shiftand one (1) person for every twenty-five (25)residents or major fraction of twenty-five(25) during the night shift. I/II
Time Personnel Residents7 a.m. to 3 p.m.
(Day)* 1 3–153 p.m. to 9 p.m.
(Evening)* 1 3–209 p.m. to 7 a.m.
(Night)* 1 3–25
*If the shift hours vary from those indicated,the hours of the shifts shall show on the workschedules of the facility and shall not be lessthan six (6) hours. III
(B) The administrator shall count towardstaffing when physically present in the facili-ty. II
(C) The required staff shall be in the facil-ity awake, dressed and prepared to assist res-idents in case of emergency. I/II
(D) Meeting these minimal staffingrequirements may not meet the needs of resi-dents as outlined in the residents’ assess-ments and individualized service plans. I/II
(E) There shall be a licensed nurseemployed by the facility to work at least eight(8) hours per week at the facility for everythirty (30) residents or additional major frac-tion of thirty (30). The nurse’s duties shallinclude, but shall not be limited to, review ofresidents’ charts, medications, and specialdiets or other orders, review of each resi-dent’s adjustment to the facility, and observa-tion of each individual resident’s generalphysical and mental condition. The nurseshall inform the administrator of any prob-lems noted, and these shall be brought to theattention of the resident’s physician. II/III
(62) Prior to or on the first day that a newemployee works in the facility he or she shallreceive orientation of at least two (2) hoursappropriate to his or her job function. Thisshall include at least the following:
(A) Job responsibilities;(B) Emergency response procedures;(C) Infection control and handwashing pro-
cedures and requirements;(D) Confidentiality of resident informa-
tion;(E) Preservation of resident dignity;(F) Information regarding what constitutes
abuse/neglect and how to reportabuse/neglect to the department (1-800-392-0210);
(G) Information regarding the EmployeeDisqualification List;
(H) Instruction regarding the rights of res-idents and protection of property;
(I) Instruction regarding working with res-idents with mental illness; and
(J) Instruction regarding person-centeredcare and the concept of a social model ofcare, and techniques that are effective in
enhancing resident choice and control overhis or her own environment. II/III
(63) In addition to the orientation trainingrequired in section (62) of this rule any facil-ity that provides care to any resident havingAlzheimer’s disease or related dementia shallprovide orientation training regarding mental-ly confused residents such as those withAlzheimer’s disease and related dementias asfollows:
(A) For employees providing direct care tosuch persons, the orientation training shallinclude at least three (3) hours of trainingincluding at a minimum an overview of men-tally confused residents such as those havingAlzheimer’s disease and related dementias,communicating with persons with dementia,behavior management, promoting indepen-dence in activities of daily living, techniquesfor creating a safe, secure and socially ori-ented environment, provision of structure,stability and a sense of routine for residentsbased on their needs, and understanding anddealing with family issues; and II/III
(B) For other employees who do not pro-vide direct care for, but may have daily con-tact with, such persons, the orientation train-ing shall include at least one (1) hour oftraining including at a minimum an overviewof mentally confused residents such as thosehaving dementias as well as communicatingwith persons with dementia; and II/III
(C) For all employees involved in the careof persons with dementia, dementia-specifictraining shall be incorporated into ongoing in-service curricula. II/III
(64) All in-service or orientation trainingrelating to the special needs, care and safetyof residents with Alzheimer’s disease andother dementia shall be conducted, presentedor provided by an individual who is qualifiedby education, experience or knowledge in thecare of individuals with Alzheimer’s diseaseor other dementia. II/III
(65) Requirements for training related tosafely transferring residents.
(A) The facility shall ensure that all staffresponsible for transferring residents areappropriately trained to transfer residentssafely. Individuals authorized to provide thistraining include a licensed nurse, a physicaltherapist, a physical therapy assistant, anoccupational therapist or a certified occupa-tional therapy assistant. The individual whoprovides the transfer training shall observethe caregiver’s skills when checking compe-tency in completing safe transfers, shall doc-ument the date(s) of training and competency
32 CODE OF STATE REGULATIONS (4/30/09) ROBIN CARNAHAN
Secretary of State
19 CSR 30-86—DEPARTMENT OF HEALTH ANDSENIOR SERVICES Division 30—Division of Regulation and Licensure
CODE OF STATE REGULATIONS 33ROBIN CARNAHAN (4/30/09)Secretary of State
Chapter 86—Residential Care Facilities and Assisted Living Facilities 19 CSR 30-86
and shall sign and maintain training docu-mentation. Initial training shall include aminimum of two (2) classroom instructionhours in addition to the on-the-job trainingrelated to safely transferring residents whoneed assistance with transfers. II/III
(B) The facility shall ensure that a mini-mum of one (1) hour of transfer training isprovided by a licensed nurse annually regard-ing safe transfer skills. II/III
AUTHORITY: sections 198.073 and 198.076,RSMo Supp. 2007.* Original rule filed Aug.23, 2006, effective April 30, 2007. Amended:Filed March 13, 2008, effective Oct. 30,2008.
*Original authority: 198.073, RSMo 1979, amended1984, 1992, 1999, 2006, 2007 and 198.076, RSMo 1979,amended 1984, 2007.
19 CSR 30-86.052 Dietary Requirementsfor Residential Care Facilities and Assist-ed Living Facilities
PURPOSE: This rule establishes standardsfor meeting dietary needs of residents in res-idential care facilities I and II.
Editor’s Note: All rules relating to long-termcare facilities licensed by the department arefollowed by a Roman Numeral notation whichrefers to the class (either class I, II or III) ofstandard as designated in section 198.085.1,RSMo 1986.
(1) Each resident shall be served food pre-pared and served under safe, sanitary condi-tions that is prepared consistent with the pref-erences of the resident and in accordancewith attending physician’s orders. The nutri-tional needs of the residents shall be met.Balanced nutritious meals using a variety offoods shall be served. Consideration shall begiven to the food habits, preferences, medicalneeds and physical abilities of the residents.II/III
(2) Each resident shall receive and the facili-ty shall provide at least three (3) meals daily,at regular times comparable to normal meal-times in the community. At least two (2)meals daily shall be hot. II/III
(3) There shall be no more than fourteen (14)hours between a substantial evening meal andbreakfast the following day, except when anourishing snack is provided at bedtime. Upto sixteen (16) hours may elapse between asubstantial evening meal and breakfast thefollowing day if a resident group agrees tothis meal span, and a nourishing snack isserved. III
(4) Fresh water shall be available to the resi-dent at all times. II/III
(5) Dining room service for residents shall beattractive and each resident shall receiveappropriate table service. III
(6) Menus shall be planned in advance andshall be readily available for personnelinvolved in food purchase and preparation.Food shall be served as planned althoughsubstitutes of equal nutritional value andcomplementary to the remainder of the mealcan be made if recorded. III
(7) A three (3)-day supply of food shall bemaintained in the facility. III
(8) If a physician prescribes in writing a mod-ified diet for a resident, the resident may beaccepted or remain in the facility if—
(A) The physician monitors the resident’scondition on a regular periodic basis and atleast quarterly; II
(B) The diet, food preparation and servingis reviewed at least quarterly by a consultingnutritionist, dietitian, registered nurse orphysician and there is written documentationof the review; II/III
(C) The modified diet menu is posted inthe kitchen and includes portions to beserved; III and
(D) The facility has entered into a writtenagreement for dietary consultation with anutritionist, dietitian registered nurse orphysician. III
(9) Nothing in this rule shall be construed astaking precedence over the resident’s right tomake decisions regarding his or her eatingand dining preferences.
(A) In assisted living facilities, informationabout the resident’s eating and dining prefer-ences shall be incorporated in his or her indi-vidualized service plan based on an assess-ment that includes the resident’s culture,life-long routines, habits, patterns and prefer-ences. III
(B) In assisted living facilities, if the resi-dent’s eating and dining preferences have apotential health risk, staff shall inform theresident or his or her legally authorized rep-resentative of the potential health risks anddocument this in his or her individualizedservice plan. III
AUTHORITY: sections 198.076, RSMo 2000and 198.005 and 198.073, RSMo Supp.2006.* This rule originally filed as 13 CSR15-15.052. Original rule filed July 13, 1983,effective Oct. 13, 1983. Emergency amend-ment filed Aug. 1, 1984, effective Aug. 13,
1984, expired Dec. 10, 1984. Amended:Filed Sept. 12, 1984, effective Dec. 13, 1984.Amended: Filed Aug. 1, 1988, effective Nov.10, 1988. Moved to 19 CSR 30-86.052, effec-tive Aug. 28, 2001. Amended: Aug. 23, 2006,effective April 30, 2007.
*Original authority: 198.005, RSMo 2006; 198.073,RSMo 1979, amended 1984, 1992, 1999, 2006; and198.076, RSMo 1979, amended 1984.
Related Documents