TRAFIP2 in adverse cardiac remodeling 1 Cardiac-Restricted Overexpression of TRAF3 Interacting Protein 2 (TRAF3IP2) Results in Spontaneous Development of Myocardial Hypertrophy, Fibrosis and Dysfunction Manjunath Yariswamy 1,2 *, Tadashi Yoshida 1 *, Anthony J. Valente 3 *, Hemanth Kumar Kandikattu 1# , Siva S.V.P. Sakamuri 4 , Jalahalli M. Siddesha 4 , Sergiy Sukhanov 1 , Zubaida Saifudeen 5 , Lixin Ma 2,6 , Ulrich Siebenlist 7 , Jason D. Gardner 8 , Bysani Chandrasekar 1# 1 Department of Medicine, University of Missouri, Columbia, MO 65211; 2 Harry S Truman Memorial Veterans’ Hospital, Columbia, MO 65201; 3 University of Texas Health Science Center at San Antonio, TX 78229; 4 Department of Medicine, Tulane University School of Medicine, New Orleans, LA 70112; 5 Department of Pediatric Nephrology, Tulane University School of Medicine, New Orleans, LA 70112; 6 Department of Radiology, University of Missouri, Columbia, MO 65211; 7 Laboratory of Molecular Immunology, NIAID, NIH, Bethesda, MD 20892; 8 Department of Physiology, Louisiana State University Health Sciences Center, New Orleans, LA 70112. Running title: TRAFIP2 in adverse cardiac remodeling *Equal contribution To whom correspondence should be addressed: Bysani Chandrasekar, DVM. Ph.D., Medicine/Cardiology, University of Missouri School of Medicine, 1 Hospital Drive, Columbia, MO 65212, Phone: 573-882-8450, Fax: 573-884-7743, E-mail: [email protected] Keywords: Adverse cardiac remodeling, myocardial hypertrophy, contractile dysfunction, cardiac fibrosis, CIKS, cardiac signaling, inflammation ABSTRACT TRAF3IP2 (TRAF3 Interacting Protein 2; also known as CIKS or Act1) is a key intermediate in the normal inflammatory response and the pathogenesis of various autoimmune and inflammatory diseases. Induction of TRAF3IP2 activates IKK/NF-κB, JNK/AP-1, and c/EBPβ, and stimulates the expression of various inflammatory mediators with negative myocardial inotropic effects. To investigate the role of TRAF3IP2 in heart disease, we generated a transgenic mouse with cardiomyocyte-specific TRAF3IP2 overexpression (TRAF3IP2-Tg). Echocardiography, magnetic resonance imaging and pressure-volume conductance catheterization revealed impaired cardiac function in 2 month-old male Tg mice, as evidenced by decreased ejection fraction, stroke volume, cardiac output and peak ejection rate. Moreover, the male Tg mice spontaneously developed myocardial hypertrophy (increased heart/body weight ratio, cardiomyocyte cross-sectional area, GATA4 induction, and fetal gene re-expression). Further, TRAF3IP2 overexpression resulted in the activation of IKK/NF-κB, JNK/AP-1, c/EBPβ and p38 MAPK, and induction of pro-inflammatory cytokines, chemokines, and extracellular matrix proteins in the heart. Although myocardial hypertrophy decreased with age, cardiac fibrosis (increased number of myofibroblasts, and enhanced expression and deposition of fibrillar collagens) increased progressively. Despite these adverse changes, TRAF3IP2 overexpression did not result in cell death at any time period. Interestingly, despite increased mRNA expression, TRAF3IP2 protein levels and activation of its downstream signaling intermediates remained unchanged in the hearts of female Tg mice. The female Tg mice also failed to develop myocardial hypertrophy. In summary, these results demonstrate that overexpression of TRAF3IP2 in male mice is sufficient to induce myocardial hypertrophy, cardiac fibrosis and contractile dysfunction. Cardiac failure is a multifactorial terminal condition resulting from pathological events that http://www.jbc.org/cgi/doi/10.1074/jbc.M116.724138 The latest version is at JBC Papers in Press. Published on July 27, 2016 as Manuscript M116.724138 Copyright 2016 by The American Society for Biochemistry and Molecular Biology, Inc. by guest on October 28, 2020 http://www.jbc.org/ Downloaded from

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

TRAFIP2 in adverse cardiac remodeling
1
Cardiac-Restricted Overexpression of TRAF3 Interacting Protein 2 (TRAF3IP2) Results in Spontaneous Development of Myocardial Hypertrophy, Fibrosis and Dysfunction
Manjunath Yariswamy1,2*, Tadashi Yoshida1*, Anthony J. Valente3*, Hemanth Kumar Kandikattu1#, Siva S.V.P. Sakamuri4, Jalahalli M. Siddesha4, Sergiy Sukhanov1, Zubaida Saifudeen5, Lixin Ma2,6, Ulrich Siebenlist7, Jason D. Gardner8, Bysani Chandrasekar1#
1Department of Medicine, University of Missouri, Columbia, MO 65211; 2 Harry S Truman Memorial Veterans’ Hospital, Columbia, MO 65201; 3University of Texas Health Science Center at San Antonio, TX 78229; 4Department of Medicine, Tulane University School of Medicine, New Orleans, LA 70112; 5Department of Pediatric Nephrology, Tulane University School of Medicine, New Orleans, LA 70112;
6Department of Radiology, University of Missouri, Columbia, MO 65211; 7Laboratory of Molecular Immunology, NIAID, NIH, Bethesda, MD 20892; 8Department of Physiology, Louisiana State University
Health Sciences Center, New Orleans, LA 70112.
Running title: TRAFIP2 in adverse cardiac remodeling
*Equal contribution
To whom correspondence should be addressed: Bysani Chandrasekar, DVM. Ph.D., Medicine/Cardiology, University of Missouri School of Medicine, 1 Hospital Drive, Columbia, MO 65212, Phone: 573-882-8450, Fax: 573-884-7743, E-mail: [email protected]
Keywords: Adverse cardiac remodeling, myocardial hypertrophy, contractile dysfunction, cardiac fibrosis, CIKS, cardiac signaling, inflammation
ABSTRACT TRAF3IP2 (TRAF3 Interacting Protein 2; also known as CIKS or Act1) is a key intermediate in the normal inflammatory response and the pathogenesis of various autoimmune and inflammatory diseases. Induction of TRAF3IP2 activates IKK/NF-κB, JNK/AP-1, and c/EBPβ, and stimulates the expression of various inflammatory mediators with negative myocardial inotropic effects. To investigate the role of TRAF3IP2 in heart disease, we generated a transgenic mouse with cardiomyocyte-specific TRAF3IP2 overexpression (TRAF3IP2-Tg). Echocardiography, magnetic resonance imaging and pressure-volume conductance catheterization revealed impaired cardiac function in 2 month-old male Tg mice, as evidenced by decreased ejection fraction, stroke volume, cardiac output and peak ejection rate. Moreover, the male Tg mice spontaneously developed myocardial hypertrophy (increased heart/body weight ratio, cardiomyocyte cross-sectional area, GATA4 induction, and fetal gene re-expression). Further, TRAF3IP2
overexpression resulted in the activation of IKK/NF-κB, JNK/AP-1, c/EBPβ and p38 MAPK, and induction of pro-inflammatory cytokines, chemokines, and extracellular matrix proteins in the heart. Although myocardial hypertrophy decreased with age, cardiac fibrosis (increased number of myofibroblasts, and enhanced expression and deposition of fibrillar collagens) increased progressively. Despite these adverse changes, TRAF3IP2 overexpression did not result in cell death at any time period. Interestingly, despite increased mRNA expression, TRAF3IP2 protein levels and activation of its downstream signaling intermediates remained unchanged in the hearts of female Tg mice. The female Tg mice also failed to develop myocardial hypertrophy. In summary, these results demonstrate that overexpression of TRAF3IP2 in male mice is sufficient to induce myocardial hypertrophy, cardiac fibrosis and contractile dysfunction.
Cardiac failure is a multifactorial terminal condition resulting from pathological events that
http://www.jbc.org/cgi/doi/10.1074/jbc.M116.724138The latest version is at JBC Papers in Press. Published on July 27, 2016 as Manuscript M116.724138
Copyright 2016 by The American Society for Biochemistry and Molecular Biology, Inc.
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
2
include pressure/volume overload, myocardial ischemia/infarction and cardiomyopathies (1). A key component in these predisposing events is sustained inflammation, which contributes to the onset and progression of the critical determinants of cardiac failure - myocardial hypertrophy, cardiac fibrosis, and contractile dysfunction (2-4). Both nuclear factor κB (NF-κB) and activator protein 1 (AP-1) pathways have been shown to play critical roles in the development and progression of hypertrophy and fibrosis, with the activation of IκB kinase (IKK) and c-Jun N-terminal kinase (JNK) being the key intermediate steps (3). For example, mice with cardiac restricted overexpression of constitutively active IKK spontaneously developed reversible inflammatory cardiomyopathy and heart failure (5). In concordance, overexpression of IκB-α super-repressor in the heart led to reduced hypertrophic response following pressure overload following angiotensin (Ang)-II/isoproterenol infusion (6). Furthermore, sustained activation of p50 and p65, the major subunits of NF-κB, play a causal role in the onset and progression of cytokine- and myocardial infarction-induced heart failure (7,8), demonstrating the critical role of sustained NF-κB activation in pathological cardiac hypertrophy and development of heart failure.
Contrary to IKK and NF-κB signaling, JNK, and the components of its downstream target AP-1 (fra1 and JunD) exhibit differential effects in the heart. Though AP-1 is upregulated during early stages of the hypertrophic response, FOSL1 (fra-1) gene deletion failed to affect the hypertrophic response to chronic pressure overload or sustained β-adrenergic stimulation (9). In contrast, fra-1 overexpression resulted in premature decompensation. Similarly, transgenic mice with JunD overexpression in a cardiomyocyte-specific manner spontaneously developed ventricular dilation and contractile dysfunction (9). Notably, fra-1 transgenic mice simultaneously lacking JunD spontaneously developed dilated cardiomyopathy due to increased cardiomyocyte death (9). These data suggest that AP-1 activation can be either protective or detrimental to the heart. In addition to NF-κB and AP-1, the nuclear transcription factor CCAAT/enhancer-binding protein beta (c/EBPβ) has been shown to contribute to physiological hypertrophy (10), indicating that
activation of NF-κB, AP-1 and c/EBPβ contribute to development of myocardial hypertrophy, and possible transition to failure.
One of the upstream regulators of these classic regulators of inflammation is the cytoplasmic adapter molecule TRAF3 Interacting Protein 2 (TRAF3IP2; also known as CIKS or Act1) (11,12). Using loss-of-function (knockout) mouse models, a number of publications have described its causal role in the pathogenesis of various autoimmune and inflammatory diseases (13-17). However, no reports are available yet describing the consequences of its overexpression in vivo. In an in vitro study, Leonardi et al., have demonstrated that ectopic overexpression of TRAF3IP2, by itself, was sufficient to induce NF-κB activation through TRAF3IP2/IKK physical association (11). We have previously demonstrated activation of JNK via TRAF3IP2/IKKγ interaction (18), implying that TRAF3IP2 overexpression could result in IKK, JNK and c/EBPβ activation in vivo with subsequent induction of inflammatory mediators, resulting in pathological changes. Therefore, we have generated a gain-of-function (transgenic) mouse model that overexpresses TRAF3IP2 in a cardiomyocyte-specific manner (TRAF3IP2-Tg), and investigated the consequences of its overexpression. RESULTS
Characterization of TRAF3IP2-Tg mice – We have generated a transgenic mouse model that overexpresses TRAF3IP2 in a cardiomyocyte-specific manner using the alpha myosin heavy chain (α-MyHC) promoter (TRAF3IP2-Tg, Fig. 1). RT-qPCR revealed markedly increased (~200 fold) TRAF3IP2 mRNA expression in the hearts of male Tg mice as compared to control NTg littermates (Fig. 2A). Its protein levels were also increased significantly in hearts by 3.48-fold, similar to those seen after Ang-II infusion in wild type mice (18) (Fig. 2B). However, its protein levels were not altered in lung, liver, small intestine, and kidneys of the Tg mice (Fig. 2C and 2D). Increased expression of TRAF3IP2 in the heart was detected specifically in cardiomyocytes (Fig. 2E), but not other myocardial constituent cells (fibroblasts, endothelial and smooth muscle
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
3
cells), confirming the generation of a Tg mouse that constitutively overexpresses TRAF3IP2 specifically in hearts (Fig. 2).
Cardiac-restricted TRAF3IP2
Overexpression Results in IKK/NF-κB, JNK/AP-1, c/EBPβ and p38 MAPK activation—Since TRAF3IP2 is an upstream regulator of IKK/NF-κB, JNK/AP-1 and c/EBPβ (11,12,19), we investigated whether TRAF3IP2 overexpression results in their spontaneous activation. The results show that phosphorylated levels of IKKβ and its downstream target p65, JNK and its downstream target c-Jun, and c/EBPβ were all increased significantly in hearts of the male Tg compared to control NTg littermates (Fig. 2F). In addition, TRAF3IP2 overexpression resulted in the activation of p38 MAPK, a stress regulated kinase (Fig. 2F), indicating that the constitutive overexpression of TRAF3IP2 results in the spontaneous activation of multiple transcription factors and stress-activated kinases that are known to induce inflammation and hypertrophic response. However, the protein levels of TRAF3IP2, phospho-p65, and phospho-p38 MAPK remained unaltered in the hearts of female Tg mice (Fig. 2G).
Cardiac restricted TRAF3IP2-Tg
Overexpression Results in Spontaneous Development of Myocardial Hypertrophy and Contractile Dysfunction—Since activation of NF-κB, AP-1, c/EBPβ and p38 MAPK has been shown to contribute to hypertrophy development (5,7-10,20,21), we next investigated whether TRAF3IP2 overexpression results in myocardial hypertrophy. At 2 months of age, both Tg and control NTg littermates underwent transthoracic echocardiography. M-mode analysis revealed a hypertrophic response only in male Tg mice as evidenced by increased LV wall thickness (22%; 1.220 ± 0.037 vs. 0.9983 ± 0.076 mm; p < 0.02) and decreased LV volume (19%; 17.61 ± 0.994 vs. 21.89 ± 2.006 µl; p < 0.02; (Fig. 3A, Table 1). B-mode tracings confirmed a decrease in chamber volume at both systole and diastole (Fig. 3B). The male Tg mice also exhibited cardiac dysfunction. The ejection fraction (EF) was decreased by 17% (51.32 ± 2.21 vs. 61.64 ± 2.95%; p < 0.02) and fractional shortening (FS) by 21% (25.75 ± 1.37%
vs. 32.78 ± 2.18%; p < 0.03 (Fig. 3C; Table 1). However, these changes were not seen in the female Tg mice, which appeared to be normal (Table 2).
Supporting the echocardiographic data, cine-MRI revealed significantly thickened LV septal wall (S, mid-ventricular short axis at end-diastole) in the male Tg mice at 2 months of age (~27%; 1.18 ± 0.04 vs. 0.928 ± 0.03 mm; p < 0.002; Fig. 3D). Furthermore, the EF was decreased by 16.5% (45.50 ± 0.7 vs. 54.5 ± 2.6%; p < 0.02), the stroke volume by ~20% (21.7 ± 0.3 vs. 27.0 ± 0.9 µl; p < 0.001), cardiac output by ~24% (8.0 ± 0.02 vs. 10.5 ± 0.4 ml/min; p < 0.002), and peak ejection rate by ~18% (0.49 ± 0.02 vs. 0.6 ± 0.03 µl/min; p < 0.03). However, end diastolic volumes were similar in both Tg and control NTg littermates. In addition, the diastolic function, peak filling rate, initial filling rate, and diastolic relaxation time were all similar in both groups (Table 1).
The findings from the pressure-volume conductance catheterization confirmed cardiac dysfunction in the male Tg mice as evidenced by decreased EF (10.5%; 56.17 ± 0.83 vs. 62.73 ± 1.42%; p < 0.006), stroke volume (22%; 43.81 ± 2.314 vs. 56.15 ± 3.02 µl; p < 0.007), and cardiac output (~21%; 22.67 ± 0.67 vs. 28.54 ± 1.35 ml/min; p < 0.0009; Table 1). However, end diastolic pressure, end systolic pressure, end diastolic volume, and end systolic volume did not vary between the two groups (Table 1). Together, these data demonstrate that male Tg mice with constitutive overexpression of TRAF3IP2 in a cardiomyocyte-specific manner spontaneously develop myocardial hypertrophy and contractile dysfunction.
Confirming the echocardiography and cine-MRI data, gross morphology showed increased heart size in the male Tg mice at 2 months of age (Fig. 4A, upper panel). Furthermore, the heart to body weight ratios (~18%; 5.038 ± 0.09 vs. 4.287 ± 0.06 mg/g; p < 0.001; Fig. 4A, lower panel), cardiomyocyte cross-sectional area (WGA staining; 451.1 ± 24.0 vs. 303.0 ± 17.45 µm2; p < 0.0005; Fig. 4B), and expression of fetal genes ANP, BNP and β-MyHC (Fig. 4C, mRNA, 16-, 9- and 6-fold, respectively; and protein, Fig. 4D), and GATA4 (Fig. 4D) were all increased in the Tg mice. However, the temporal studies showed that the hypertrophic
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
4
response continued for up to 4 months of age, but improved at later time periods (Fig. 4E).
In contrast to the males, the female Tg mice did not develop myocardial hypertrophy (HW/BW ratios, 4%; Tg, 4.61 ± 0.04 vs. NTg littermates, 4.43 ± 0.19 mg/g, n=5-7/group). Furthermore, ANP and GATA4 levels remained low, essentially at control levels (Fig. 4F), suggesting a gender-dependent effect of TRAF3IP2 in the hypertrophic response.
TRAF3IP2 Overexpression Results in
Cardiac Fibrosis—Myocardial hypertrophy is associated with a fibrotic response (22), with remodeling of the extracellular matrix (ECM) playing a key role in its development and progression. The key structural proteins involved in cardiac fibrosis are collagens type 1α1 (ColIα1) and type IIIα1 (ColIIIα1). The expression levels of these matrix genes were increased markedly in the hearts of male Tg mice at 2 months of age (mRNA, Fig. 5A; protein, Fig. 5B). Furthermore, the mRNA expression of lysyl oxidase (LOX), a key regulator of collagen cross-linking and deposition of insoluble collagens (23), was also increased in the Tg heart, as was LOX enzyme activity (Fig. 5B). The mRNA levels of the growth factor CTGF, a positive regulator of collagen expression (24), were also increased in the Tg hearts (Fig. 5A, 5B). Together, these data demonstrate that TRAF3IP2 overexpression leads to increased expression of the fibrillar collagens (Iα1 and IIIα1) and their positive regulator CTGF, and activation of LOX in Tg hearts, changes that might have contributed to cardiac fibrosis.
Supporting the mRNA and protein data, immunofluorescence studies revealed increased deposition and co-localization of ColIα1 and IIIα1 in the Tg heart (Fig. 5C). However, unlike myocardial hypertrophy, which improved after 4 months of age (Fig. 4E), fibrosis continued to increase with age in the Tg hearts, with even higher collagen levels detectable at 8 months of age (Fig. 5D).
Activated fibroblasts are the predominant cell type responsible for increased expression and deposition of collagens (25,26). Inflammatory and hypertrophic stimuli trigger the differentiation of resident cardiac fibroblasts into a more contractile and synthetic phenotype, called myofibroblasts
(25). To determine whether, TRAF3IP2 overexpression promotes differentiation of fibroblasts to myofibroblasts in the hypertrophied myocardium, we analyzed various markers of tissue components of the heart. The results show that whereas the expression of CD-31, a surface marker expressed predominantly on endothelial cells (27), remained unchanged (Fig. 6A). α-SMA, one of the markers of myofibroblasts (25,28), was greatly increased in vascular smooth muscle cells and myofibroblasts of Tg hearts (Fig. 6A). Furthermore, tensin, which is expressed in myofibroblasts (29), was detected only in the Tg hearts (Fig. 6B). Paxillin, expressed in both vasculature and myofibroblasts (29), also increased in the Tg hearts (Fig. 6C). Thus, TRAF3IP2 overexpression resulted in increased myofibroblasts in the hypertrophied Tg heart. Supporting these observations, the Quantibody® Mouse Cytokine Antibody Array also showed a 2.4-fold increase in the expression of periostin (Table 3), another marker of myofibroblasts (29).
TRAF3IP2 Overexpression Results in
Enhanced Expression of Pro-inflammatory Mediators in the Heart—Inflammation is a major risk factor associated with cardiac pathologies, including hypertrophy, fibrosis, dysfunction and failure (2-4). Potent pro-inflammatory cytokines such as IL-6, IL-17, IL-18, and TNF-α mediate both hypertrophic and fibrotic responses in the heart, and contribute to contractile dysfunction and heart failure development (30). The chemokine fractalkine also inhibits cardiomyocyte contractility (31). In the Tg mouse hearts there was an increase in the expression of IL-6 and IL-18 at both mRNA (Fig. 7A) and protein levels (Fig. 7B). Further, antibody array analysis showed a significant increase in cytokines (IL-6, TWEAK, TWEAKR, β-FGF, IL-17, TNF-α, G-CSF, and M-CSF), chemokines (fractalkine), and adhesion molecules (E-selectin, P-selectin, ICAM-1, VCAM-1) in Tg mouse hearts (Table 3). In addition, MMP-3 and MMP-10 levels were also higher in the Tg mice (Table 3). Interestingly, although expression levels of the pro-hypertensive mediators angiotensin converting enzyme (ACE), angiotensin III (Ang-III) and renin-3 were elevated in Tg mice (Table 3), no significant changes in blood pressure were detected (tail cuff plethysmography; data not shown). Unlike in
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
5
male Tg mice, the levels of most of these pro-inflammatory, pro-hypertrophic, and pro-fibrotic mediators remained low or unchanged in the hearts of female Tg mice (Table 3).
Macrophage infiltration is a common feature of cardiac inflammation (32), and Mac3 serves as a general marker for macrophages. Immunofluorescent studies showed an increased number of Mac3+ cells in the Tg hearts (Fig. 7C). Of note, macrophages contribute to adverse cardiac remodeling by expressing various pro-inflammatory, pro-hypertrophic and pro-fibrotic mediators (32). Together, these results indicate that constitutive overexpression of TRAF3IP2 results in the upregulation of various inflammatory mediators and infiltration of inflammatory cells into the heart, possibly promoting hypertrophy, fibrosis and dysfunction, in the male Tg mice.
DISCUSSION
The results of this study show for the first time that cardiac-restricted TRAF3IP2 overexpression (TRAF3IP2-Tg) results in the spontaneous development of myocardial hypertrophy, cardiac fibrosis and contractile dysfunction. While hypertrophy resolved with age, fibrosis progressed in the Tg mice. These adverse cardiac changes occurred only in the male Tg mice. Overexpression of TRAF3IP2 did not appear to induce cell death, despite progressive fibrosis, and the Tg mice failed to develop heart failure during the 8 month-study period (data not shown). These results indicate that persistently elevated TRAF3IP2 plays a causal role in adverse cardiac remodeling, at least in male mice.
The overexpression of TRAF3IP2 resulted in the activation of IKK/NF-κB, JNK/AP-1, c/EBPβ, and p38 MAPK, all of which have been shown to contribute to the development of myocardial hypertrophy, fibrosis, contractile dysfunction, and heart failure (3,5,7-10,20,21), suggesting that TRAF3IP2 overexpression may elicit hypertrophic response. In fact, its overexpression resulted in myocardial hypertrophy, which was evident as early as 2 months of age, but this resolved by 6 months of age. In contrast, these mice showed progressive fibrosis, which did not resolve with age. Since cardiac fibrosis leads to diastolic dysfunction and
heart failure development (33), we will continue to monitor these Tg mice until moribund.
In addition to activation of multiple transcription factors and p38 MAPK, TRAF3IP2 overexpression also resulted in increased levels of GATA4, a member of the highly conserved zinc finger-containing transcription factors that regulates cardiomyocyte hypertrophy and induction of fetal gene program (34). In fact, the Tg mice showed increased levels of ANP, BNP, and β-MyHC, all of which are GATA4-responsive genes (34). Surprisingly, in a recent study, GATA4 has been shown to activate NF-κB in TRAF3IP2-dependent manner (35), suggesting that TRAF3IP2 may activate NF-κB by multiple pathways, including IKK and GATA4, both of which are increased in the Tg mice.
Adverse/maladaptive cardiac remodeling is an important predictor of heart failure development, and is associated with persistently elevated levels of multiple pro-inflammatory cytokines with negative myocardial inotropic effects (30). In fact, increased levels of IL-6, IL-17, IL-18 and TNF-α were detected in the Tg mouse hearts. While significantly affecting myocardial fibrosis, each of these cytokines also exert pro-hypertrophic effects on cardiomyocytes through activation of intracellular stress-activated kinases, including p38 MAPK. TRAF6, which physically associates with TRAF3IP2 (36), is a well-known inducer of p38 MAPK activation (37), and plays a role in the induction of multiple pro-inflammatory mediators known to induce myocardial hypertrophy and cardiac fibrosis. Of note, p38 MAPK is also involved in GATA4 activation in cardiomyocytes (38).
IL-6, a pro-inflammatory and pro-hypertrophic cytokine, promotes fibrosis by stimulating increased deposition of collagens by myofibroblasts, resulting in a stiffened heart with contractile dysfunction (39). Similarly, the pro-inflammatory cytokine IL-18 exerts pro-hypertrophic effects via a PI3K-Akt-GATA4-dependent signaling (40). IL-18 also exerts pro-fibrotic and pro-apoptotic effects in cardiac fibroblasts and endothelial cells, respectively (41,42). Increased levels of TNF-α induce cardiac dysfunction, cardiomyopathy, adverse LV remodeling, apoptosis and cachexia (43). In addition to increased levels of IL-6, IL-18 and TNF-α, TRAF3IP2 overexpression also resulted in
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
6
increased expression of TWEAK and its receptor - TWEAKR, both of which are known to contribute to the onset of hypertrophy, fibrosis and dysfunction. In fact, transgenic mice overexpressing soluble TWEAK, specifically in cardiomyocytes, showed increased mortality (44,45), suggesting that its sustained induction promotes heart failure development. TWEAK also induces elongation of cardiomyocytes, fibroblast proliferation, collagen synthesis, and perivascular fibrosis in the Tg mice overexpressing full-length TWEAK (44).
In addition to the hypertrophic and fibrotic responses by the classical pro-inflammatory cytokines, IL-17 also induces cardiac inflammation, hypertrophy and fibrosis (46,47). TRAF3IP2 is a critical intermediate in IL-17 signaling (11,12). Here we have shown that TRAF3IP2 overexpression in male mice resulted in a 5.8-fold increase in IL-17A expression in the heart (Table 3). Thus, increased expression of IL-17A and its signaling intermediate TRAF3IP2 may cooperatively enhance the inflammatory response in the heart. IL-17A also exerts pro-fibrotic effects. It induces cardiac fibroblast proliferation and migration via p38 MAPK and ERK1/2 activation and MKP-1 inactivation (48). On the other hand, its gene deletion inhibits the onset of myocarditis and progression to inflammatory dilated cardiomyopathy (47). Further, macrophage/monocyte-derived IL-17A may induce TNF-α, IL-1β, MCP-1, and MMPs that play a role in adverse cardiac remodeling (49).
In addition to myocardial hypertrophy, the male Tg mice also developed cardiac fibrosis. Cardiac fibrosis is a critical component in cardiac remodeling and an important predictor of heart failure development (33). It is a progressive disease, and results from an excess accumulation of ECM components, including collagens, secreted predominantly by myofibroblasts. Myofibroblasts also express LOX, the collagen cross-linking enzyme. Increased expression of LOX results in the deposition of insoluble collagens that adversely affect cardiac contractility (23). Of note, LOX activation is increased during adverse cardiac remodeling and heart failure development (23). Our results showed that the male Tg hearts expressed higher levels of activated LOX. Of note, both collagens and LOX are NF-κB and AP-1 responsive genes (50,51). Thus, TRAF3IP2
overexpression results in the spontaneous induction of various pro-fibrotic mediators and the development of cardiac fibrosis in the male Tg mice.
Interestingly, the expression levels of these remodeling-associated inflammatory mediators remained either unaltered or downregulated in the hearts of female Tg mice, suggesting that female sex hormones may negatively regulate TRAF3IP2 expression or its downstream signaling intermediates. In fact, in a recent study, we have observed reduced atherosclerotic plaque burden in female Apoe/TRAF3IP2 double knockout mice fed a Western diet (52). In another study, TRAF3IP2 was shown to mediate estrogen-deficient osteoporosis (53), further supporting the hypothesis that female sex hormones may negatively regulate TRAF3IP2 expression via mechanisms yet to be investigated.
In conclusion, this is the first study using a ‘gain-of-function’ approach to investigate the causal role of TRAF3IP2 in adverse cardiac remodeling. Cardiac-restricted constitutive overexpression of TRAF3IP2 spontaneously resulted in inflammation, myocardial hypertrophy, cardiac fibrosis and contractile dysfunction.
Future perspectives: (i) Since the female Tg mice failed to develop myocardial hypertrophy, we will determine whether ovariectomy elicits a hypertrophic response. (ii) The female Tg mice showed increased TRAF3IP2 mRNA, but not protein expression, suggesting its post-transcriptional or post-translational regulation by female sex hormones. Therefore, we will analyze changes in miRNA and LncRNA profiles in hearts from male and female Tg mice, identify the ones that are differentially expressed, investigate their effects on TRAF3IP2 expression, and determine their therapeutic potential. (iii) Despite myocardial hypertrophy and cardiac fibrosis, the male Tg mice failed to develop heart failure. Therefore, we will determine whether additional stressors such as myocardial infarction will result in earlier decompensation and heart failure development or death. (iv) Since pharmacological inhibitors of TRAF3IP2 are not available yet, we will determine whether silencing TRAF3IP2 in the Tg mice with an AAV9-based gene therapeutic approach using a truncated cardiac troponin T promoter that provides cardiomyocyte specificity
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
7
will blunt development of hypertrophy, fibrosis and contractile dysfunction. (v) Like cardiomyocytes, cardiac fibroblasts are critical in adverse cardiac remodeling. Therefore, we will determine whether transgenic overexpression of TRAF3IP2 in a cardiac fibroblast-specific manner develops cardiac fibrosis earlier and progress to heart failure faster. Our long-term goal is to develop small molecule or pharmacological TRAF3IP2 inhibitors, and investigate their translational potential in cardiac diseases.
EXPERIMENTAL PROCEDURES
Animal studies— All animal studies were approved by the Institutional Animal Care and Use Committees at Tulane University, New Orleans, LA and the Harry S Truman VA Memorial Hospital/University of Missouri, Columbia, MO, and conformed to the Guide for the Care and Use of Laboratory Animals published by the NIH. Wild type FVB mice were purchased from The Jackson Laboratory (Ann Harbor, ME).
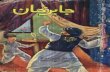
Generation of TRAF3IP2-Tg Mice and
Copy Number Determination— Mus musculus TRAF3IP2 cDNA was amplified by RT-PCR using heart RNA isolated from C57BL/6 mice as the starting template. The PCR product was cloned into α-MyHC promoter vector (Fig. 1A; a kind gift from Jeffrey Robbins, Cincinnati, Ohio; α-MyHC promoter GenBank accession #U71441), and the nucleotide sequence was confirmed. The resultant construct of ~7.8kb (Fig. 1B) was used to generate Tg mice. PCR screening was used to identify the founder animals, and three Tg lines (lines 1, 2 and 3) were generated by breeding the founder mice with wild type FVB mice (The Jackson Labs). Line 1 was used in the present study. Transgene copy number was determined by Southern blot analysis using genomic DNA isolated from tail snips and digested with EcoRV and NotI (Fig. 1C). Genotyping was performed by PCR using genomic DNA isolated from tail snips and the following primers: forward, 5’-TGT CTG ATT CAT GGC CAG TGT CAG GAG-3’ and reverse: 5’-CGG CAC TCT TAG CAA ACC TCA GGC AC-3’ (Fig. 1D).
Temporal studies—TRAF3IP2-Tg mice
(hereafter referred to as Tg) were bred with wild
type FVB mice. The offspring were screened for the transgene by PCR. Naïve Tg mice along with the littermates were investigated for up to 8 months of age. Blood pressure was recorded between 9-11am using tail-cuff plethysmography (BP 2000 Blood Pressure Analysis System, Visitech).
Echocardiography —Both male Tg and
age-matched littermates (n=6 in each group) were subjected to transthoracic echocardiography under isoflurane anesthesia using a Vevo 770 high-resolution ultrasound system (FUJIFILM VisualSonics, Toronto, ON) with a 30-MHz frequency real-time microvisualization scan head (RMV707). Motion (M)-mode and bi-dimensional (B)-mode tracings were taken and the parameters for anatomical alterations in left ventricle (LV anterior and posterior wall thickness, internal diameters at systole and diastole) and function (EF and FS) were evaluated. FS was calculated using the following equation: %FS= LVEDD-LVESD/LVEDDx100.
In Vivo High Resolution Cine-MRI—
Non-invasive MRI was performed on anesthetized mice (1.8–2.7% isoflurane) using a small bore 7 Tesla Bruker BioSpec MRI scanner equipped with a phased array mouse heart coil combined with an 86 mm volume coil (Bruker Biospin Inc., Bellaraca, MA) (54). Body temperature was maintained with warm air and respiration rate was monitored using a small animal monitoring system (SA Instruments, Inc., Stony Brook, NY). A retrospective FLASH cine pulse sequence was applied with the following parameters: 1-mm slice thickness and 30 × 30-mm2 field of views for LV in short-axis images. LV functional parameters were determined using a series of cine images of the LV in short-axis view acquired at 20 equally spaced time points throughout the entire cardiac cycle with a frame rate of 7–9 ms/frame. Five to six short-axis slices were acquired over the whole LV. At each time point, the endocardial borders were traced to measure the LV chamber area for each short-axis slice using Segment version 1.8 R0736 (http://segment.heiberg.se) software (14). LV volumes at each phase were calculated as the sum of chamber areas of all slices multiplied by 1 mm of the slice thickness. The systolic and
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
8
diastolic functions were calculated using a previously established protocol (15).
LV Chamber Volume and Contractile
Function—Mice anesthetized with isoflurane were subjected to in vivo LV chamber volume and function analysis using a Scisense ADVantage™ Pressure Volume conductance catheter (FTS-1912B; Scisense Inc.) inserted into the LV via the right carotid artery (55). Data were analyzed using iWorx© Labscribe Instrument software (Dover, NH, USA) (16).
Cardiac Hypertrophy—In addition to
echocardiography and cine-MRI, myocardial hypertrophy was determined by (i) heart to body weight ratios, (ii) cardiomyocyte cross-sectional area by wheat germ agglutinin (WGA) staining, and (iii) fetal gene (ANP, BNP, β-MyHC) re-expression. Cardiomyocyte size was determined as the mean area of 10-15 randomly selected cells/field from a total of 8-10 fields per section.
Cardiac Fibrosis—Fibrosis was
characterized by (i) immunofluorescence for ColIα1 and ColIIIα1, and (ii) Masson Trichrome staining.
Immunofluorescence—A thin midsection
of heart was fixed overnight in 4% buffered paraformaldehyde, embedded in paraffin, cut into 4 µM-thick sections and used for immunofluorescence. The following targets were analyzed: (i) TRAF3IP2 using anti-TRAF3IP2 antibody (1:25; #sc-100647, Santa Cruz Biotechnology, Inc.) and Alexa Fluor® 488-tagged donkey anti-mouse secondary antibody (1:400; # A-21202; Thermo Fisher Scientific). Hoechst (1:400; #H-3570, Thermo Fisher Scientific) was used to visualize nuclei. To identify and quantify cardiomyocyte cell size, tissue sections were permeabilized with 0.4% TBST following antigen retrieval (citrate buffer; 45 min in a steamer) and incubated with Alexa Fluor® 594-tagged wheat germ agglutinin (WGA, 20 µg/ml; #H3570, Thermo Fisher Scientific). α-SMA, tensin, paxillin, and CD-31 were used to identify myofibroblasts. α-SMA was detected using anti-α-SMA antibody (1:400; #CBL171, EMD Millipore). Alexa Fluor® 555-tagged donkey anti-mouse was used as a secondary
antibody (1:400; #A-31570, Thermo Fisher Scientific). Similarly, Tensin (1:50, #sc-8888, Santa Cruz Biotechnology, Inc.), paxillin (1:100, #ab32084, abcam), and CD-31 (1:50, #ab28364, abcam) were localized. To identify macrophages, heart sections were incubated with anti-Mac3 antibody (1:100, #553322, BD Pharmingen). Alexa Fluor®-555-tagged donkey anti-mouse antibody was used as the secondary antibody. For collagen immunofluorescence, 10 µm-thick cryosections were initially incubated with anti-ColIIIα1 antibody (1:50; #600-401-105, Rockland Immunochemicals) followed by Alexa Fluor®-488-tagged donkey anti-rabbit antibody. After washing, the sections were incubated with biotinylated anti-ColIα1 antibody (1:50; #600-401-103, Rockland Immunochemicals) and streptavidin, Alexa Fluor® 594 conjugate (1:400; #S32356; Thermo Fisher Scientific). Photomicrographs were obtained using a Nikon Eclipse 80i microscope and a Spot RT digital camera, and analyzed by SPOT Advanced Software (Sterling Heights, MI).
mRNA Expression—Total RNA was isolated from frozen LV tissue using Trizol reagent (Sigma) and 0.5 µg of RNA was reverse transcribed into cDNA using a reverse transcription kit (Agilent Technologies). mRNA expression was quantified by RT-qPCR using the following Applied Biosystems™ TaqMan™ probes: ANP (Assay ID: Mm01255748), BNP (Assay ID: Mm01255770_g1), β-MyHC (Myh7; Assay ID: Mm01319006_g1), ColIα1 (Assay ID: Mm00801666), ColIIIα1 (Assay ID: Mm1254476), CTGF (Assay ID: Mm01192932_g1), IL-6 (Assay ID: Mm00446191), IL-18 (Assay ID: Mm00434226), LOX (Assay ID: Mm00495386), and TRAF3IP2 (Assay ID: Mm00506094_m1). 18S rRNA (Assay ID: Hs99999901) served a loading control. All data were normalized to corresponding 18S levels and analyzed using 2−ΔΔCt method.
Protein Quantibody Array—A
Quantibody® Mouse Cytokine Antibody Array 4000 (#QAM-CAA-4000; RayBiotech) was used to analyze changes in protein expression in LV homogenates. The assay is a multiplexed sandwich ELISA-based quantitative array platform that simultaneously detects and quantifies 200
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
9
cytokines. Results are expressed as fold change compared to corresponding NTg littermates of similar age and gender. A fold change of 1.5 was used as a reference standard.
Immunoblotting—Preparation of LV
homogenates, electrophoresis and immunoblotting were described previously (18,40-42). The following antibodies were used: TRAF3IP2 (1:500; #NB100-56740, Novus), ANP (1:400; #NBP2-14873, Novus), α-tubulin (1:1000; #2144, Cell Signaling Technology or CST), phospho-p65 (Ser536; 1:1000; #3031, CST), p65 (1:1000; #8242, CST), phospho-c-Jun (Ser63, 1:1000; #9261, CST), c-Jun (1:1000; #9165, CST), JNK (1:1000; #9252, CST), phospho-JNK (Thr183/Tyr185; 1: 1000, #4668, CST), IKKβ (1:1000; #2678, CST), and phospho-IKKα/β (Ser176/180; 1:1000; #2694, CST), LOX (1:500; #sc-373995, Santa Cruz Biotechnology or SCB), BNP (1:400, #sc-67455,
SCB), ColIα1 (1:2000; #ab34170, abcam), ColIIIα1 (1:2000; #ab7778, abcam), CTGF (1:500; #210303, US Biological) and β-MyHC (1:400, #M9850-11C, US Biological).
Statistical analysis— Data were analyzed using Microsoft Excel, Clampfit (Molecular Device, Sunnyvale, CA), and Origin 7 (OriginLab Corp., Northampton, MA) programs. Normality criteria were evaluated to select the correct parametric or non-parametric test using the Shapiro-Wilk estimator. Since the sample size was small (n=4-8/group), the test determined that non-parametric approach should be used to avoid type II errors. Since two groups were used (Tg and NTg), pairwise comparisons were made using the Tukey adjustment. The statistical tests were performed using the software SPSS 23.0.0.1 (Chicago, IL). The overall significance level was set at 0.05. The results are presented as the mean ± SEM.
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
10
Acknowledgements: We thank Jiao Liu and Van Ninh for assistance with immunofluorescence and echocardiography, respectively. We gratefully acknowledge the support of the Biomolecular Imaging Center at the Harry S Truman Memorial Veterans’ Hospital and the University of Missouri-Columbia. Conflict of Interest: The authors declare that they have no conflicts of interest with the contents of this article. Author contributions: BC designed the experimental strategy and interpreted the data. YM, AJV, TY, HK, SS and SZ performed experiments. TY, SSVP, JMS and US contributed to vector generation, sequencing, restriction digestion, purification, southern blots, characterization, and breeding of the transgenic mouse model. YM, TY and AJV analyzed the data. YM, TY, AJV and BC wrote the manuscript. JDG performed echocardiography and pressure-volume conductance catheterization. LM performed cardiac MRI.
REFERENCES 1. Lorell, B. H., and Carabello, B. A. (2000) Left ventricular hypertrophy: pathogenesis, detection,
and prognosis. Circulation 102, 470-479 2. Lloyd-Jones, D. M., Larson, M. G., Leip, E. P., Beiser, A., D'Agostino, R. B., Kannel, W. B.,
Murabito, J. M., Vasan, R. S., Benjamin, E. J., Levy, D., and Framingham Heart, S. (2002) Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation 106, 3068-3072
3. Liu, Q., Chen, Y., Auger-Messier, M., and Molkentin, J. D. (2012) Interaction between NFkappaB and NFAT coordinates cardiac hypertrophy and pathological remodeling. Circ Res 110, 1077-1086
4. Heymans, S., Hirsch, E., Anker, S. D., Aukrust, P., Balligand, J. L., Cohen-Tervaert, J. W., Drexler, H., Filippatos, G., Felix, S. B., Gullestad, L., Hilfiker-Kleiner, D., Janssens, S., Latini, R., Neubauer, G., Paulus, W. J., Pieske, B., Ponikowski, P., Schroen, B., Schultheiss, H. P., Tschope, C., Van Bilsen, M., Zannad, F., McMurray, J., and Shah, A. M. (2009) Inflammation as a therapeutic target in heart failure? A scientific statement from the Translational Research Committee of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 11, 119-129
5. Maier, H. J., Schips, T. G., Wietelmann, A., Kruger, M., Brunner, C., Sauter, M., Klingel, K., Bottger, T., Braun, T., and Wirth, T. (2012) Cardiomyocyte-specific IkappaB kinase (IKK)/NF-kappaB activation induces reversible inflammatory cardiomyopathy and heart failure. Proc Natl Acad Sci U S A 109, 11794-11799
6. Freund, C., Schmidt-Ullrich, R., Baurand, A., Dunger, S., Schneider, W., Loser, P., El-Jamali, A., Dietz, R., Scheidereit, C., and Bergmann, M. W. (2005) Requirement of nuclear factor-kappaB in angiotensin II- and isoproterenol-induced cardiac hypertrophy in vivo. Circulation 111, 2319-2325
7. Kawamura, N., Kubota, T., Kawano, S., Monden, Y., Feldman, A. M., Tsutsui, H., Takeshita, A., and Sunagawa, K. (2005) Blockade of NF-kappaB improves cardiac function and survival without affecting inflammation in TNF-alpha-induced cardiomyopathy. Cardiovasc Res 66, 520-529
8. Hamid, T., Guo, S. Z., Kingery, J. R., Xiang, X., Dawn, B., and Prabhu, S. D. (2011) Cardiomyocyte NF-kappaB p65 promotes adverse remodelling, apoptosis, and endoplasmic reticulum stress in heart failure. Cardiovasc Res 89, 129-138
9. Ricci, R., Eriksson, U., Oudit, G. Y., Eferl, R., Akhmedov, A., Sumara, I., Sumara, G., Kassiri, Z., David, J. P., Bakiri, L., Sasse, B., Idarraga, M. H., Rath, M., Kurz, D., Theussl, H. C., Perriard, J. C., Backx, P., Penninger, J. M., and Wagner, E. F. (2005) Distinct functions of junD in cardiac hypertrophy and heart failure. Genes Dev 19, 208-213
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
11
10. Molkentin, J. D. (2011) The transcription factor C/EBPbeta serves as a master regulator of physiologic cardiac hypertrophy. Circ Res 108, 277-278
11. Leonardi, A., Chariot, A., Claudio, E., Cunningham, K., and Siebenlist, U. (2000) CIKS, a connection to Ikappa B kinase and stress-activated protein kinase. Proc Natl Acad Sci U S A 97, 10494-10499
12. Li, X., Commane, M., Nie, H., Hua, X., Chatterjee-Kishore, M., Wald, D., Haag, M., and Stark, G. R. (2000) Act1, an NF-kappa B-activating protein. Proc Natl Acad Sci U S A 97, 10489-10493
13. Qian, Y., Liu, C., Hartupee, J., Altuntas, C. Z., Gulen, M. F., Jane-Wit, D., Xiao, J., Lu, Y., Giltiay, N., Liu, J., Kordula, T., Zhang, Q. W., Vallance, B., Swaidani, S., Aronica, M., Tuohy, V. K., Hamilton, T., and Li, X. (2007) The adaptor Act1 is required for interleukin 17-dependent signaling associated with autoimmune and inflammatory disease. Nat Immunol 8, 247-256
14. Pisitkun, P., Claudio, E., Ren, N., Wang, H., and Siebenlist, U. (2010) The adaptor protein CIKS/ACT1 is necessary for collagen-induced arthritis, and it contributes to the production of collagen-specific antibody. Arthritis Rheum 62, 3334-3344
15. Sonder, S. U., Paun, A., Ha, H. L., Johnson, P. F., and Siebenlist, U. (2012) CIKS/Act1-mediated signaling by IL-17 cytokines in context: implications for how a CIKS gene variant may predispose to psoriasis. J Immunol 188, 5906-5914
16. Kang, Z., Wang, C., Zepp, J., Wu, L., Sun, K., Zhao, J., Chandrasekharan, U., DiCorleto, P. E., Trapp, B. D., Ransohoff, R. M., and Li, X. (2013) Act1 mediates IL-17-induced EAE pathogenesis selectively in NG2+ glial cells. Nat Neurosci 16, 1401-1408
17. Wu, L., Zepp, J., and Li, X. (2012) Function of Act1 in IL-17 family signaling and autoimmunity. Adv Exp Med Biol 946, 223-235
18. Valente, A. J., Clark, R. A., Siddesha, J. M., Siebenlist, U., and Chandrasekar, B. (2012) CIKS (Act1 or TRAF3IP2) mediates Angiotensin-II-induced Interleukin-18 expression, and Nox2-dependent cardiomyocyte hypertrophy. J Mol Cell Cardiol 53, 113-124
19. Ruddy, M. J., Wong, G. C., Liu, X. K., Yamamoto, H., Kasayama, S., Kirkwood, K. L., and Gaffen, S. L. (2004) Functional cooperation between interleukin-17 and tumor necrosis factor-alpha is mediated by CCAAT/enhancer-binding protein family members. J Biol Chem 279, 2559-2567
20. Frantz, S., Hu, K., Bayer, B., Gerondakis, S., Strotmann, J., Adamek, A., Ertl, G., and Bauersachs, J. (2006) Absence of NF-kappaB subunit p50 improves heart failure after myocardial infarction. FASEB J 20, 1918-1920
21. Auger-Messier, M., Accornero, F., Goonasekera, S. A., Bueno, O. F., Lorenz, J. N., van Berlo, J. H., Willette, R. N., and Molkentin, J. D. (2013) Unrestrained p38 MAPK activation in Dusp1/4 double-null mice induces cardiomyopathy. Circ Res 112, 48-56
22. Hou, J., and Kang, Y. J. (2012) Regression of pathological cardiac hypertrophy: signaling pathways and therapeutic targets. Pharmacol Ther 135, 337-354
23. Lopez, B., Querejeta, R., Gonzalez, A., Larman, M., and Diez, J. (2012) Collagen cross-linking but not collagen amount associates with elevated filling pressures in hypertensive patients with stage C heart failure: potential role of lysyl oxidase. Hypertension 60, 677-683
24. Koitabashi, N., Arai, M., Kogure, S., Niwano, K., Watanabe, A., Aoki, Y., Maeno, T., Nishida, T., Kubota, S., Takigawa, M., and Kurabayashi, M. (2007) Increased connective tissue growth factor relative to brain natriuretic peptide as a determinant of myocardial fibrosis. Hypertension 49, 1120-1127
25. Fan, D., Takawale, A., Lee, J., and Kassiri, Z. (2012) Cardiac fibroblasts, fibrosis and extracellular matrix remodeling in heart disease. Fibrogenesis Tissue Repair 5, 15
26. Prabhu, S. D., and Frangogiannis, N. G. (2016) The Biological Basis for Cardiac Repair After Myocardial Infarction: From Inflammation to Fibrosis. Circ Res 119, 91-112
27. van Mourik, J. A., Leeksma, O. C., Reinders, J. H., de Groot, P. G., and Zandbergen-Spaargaren, J. (1985) Vascular endothelial cells synthesize a plasma membrane protein indistinguishable from the platelet membrane glycoprotein IIa. J Biol Chem 260, 11300-11306
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
12
28. Baum, J., and Duffy, H. S. (2011) Fibroblasts and myofibroblasts: what are we talking about? J Cardiovasc Pharmacol 57, 376-379
29. Lajiness, J. D., and Conway, S. J. (2012) The dynamic role of cardiac fibroblasts in development and disease. J Cardiovasc Transl Res 5, 739-748
30. Mann, D. L. (2015) Innate immunity and the failing heart: the cytokine hypothesis revisited. Circ Res 116, 1254-1268
31. Taube, D., Xu, J., Yang, X. P., Undrovinas, A., Peterson, E., and Harding, P. (2013) Fractalkine depresses cardiomyocyte contractility. PLoS One 8, e69832
32. Barin, J. G., Rose, N. R., and Cihakova, D. (2012) Macrophage diversity in cardiac inflammation: a review. Immunobiology 217, 468-475
33. Kong, P., Christia, P., and Frangogiannis, N. G. (2014) The pathogenesis of cardiac fibrosis. Cell Mol Life Sci 71, 549-574
34. Molkentin, J. D. (2000) The zinc finger-containing transcription factors GATA-4, -5, and -6. Ubiquitously expressed regulators of tissue-specific gene expression. J Biol Chem 275, 38949-38952
35. Kang, C., Xu, Q., Martin, T. D., Li, M. Z., Demaria, M., Aron, L., Lu, T., Yankner, B. A., Campisi, J., and Elledge, S. J. (2015) The DNA damage response induces inflammation and senescence by inhibiting autophagy of GATA4. Science 349, aaa5612
36. Kanamori, M., Kai, C., Hayashizaki, Y., and Suzuki, H. (2002) NF-kappaB activator Act1 associates with IL-1/Toll pathway adaptor molecule TRAF6. FEBS Lett 532, 241-246
37. Cuadrado, A., and Nebreda, A. R. (2010) Mechanisms and functions of p38 MAPK signalling. Biochem J 429, 403-417
38. Charron, F., Tsimiklis, G., Arcand, M., Robitaille, L., Liang, Q., Molkentin, J. D., Meloche, S., and Nemer, M. (2001) Tissue-specific GATA factors are transcriptional effectors of the small GTPase RhoA. Genes Dev 15, 2702-2719
39. Melendez, G. C., McLarty, J. L., Levick, S. P., Du, Y., Janicki, J. S., and Brower, G. L. (2010) Interleukin 6 mediates myocardial fibrosis, concentric hypertrophy, and diastolic dysfunction in rats. Hypertension 56, 225-231
40. Chandrasekar, B., Mummidi, S., Claycomb, W. C., Mestril, R., and Nemer, M. (2005) Interleukin-18 is a pro-hypertrophic cytokine that acts through a phosphatidylinositol 3-kinase-phosphoinositide-dependent kinase-1-Akt-GATA4 signaling pathway in cardiomyocytes. J Biol Chem 280, 4553-4567
41. Chandrasekar, B., Boylston, W. H., Venkatachalam, K., Webster, N. J., Prabhu, S. D., and Valente, A. J. (2008) Adiponectin blocks interleukin-18-mediated endothelial cell death via APPL1-dependent AMP-activated protein kinase (AMPK) activation and IKK/NF-kappaB/PTEN suppression. J Biol Chem 283, 24889-24898
42. Valente, A. J., Sakamuri, S. S., Siddesha, J. M., Yoshida, T., Gardner, J. D., Prabhu, R., Siebenlist, U., and Chandrasekar, B. (2013) TRAF3IP2 mediates interleukin-18-induced cardiac fibroblast migration and differentiation. Cell Signal 25, 2176-2184
43. Mann, D. L. (2002) Tumor necrosis factor-induced signal transduction and left ventricular remodeling. J Card Fail 8, S379-386
44. Jain, M., Jakubowski, A., Cui, L., Shi, J., Su, L., Bauer, M., Guan, J., Lim, C. C., Naito, Y., Thompson, J. S., Sam, F., Ambrose, C., Parr, M., Crowell, T., Lincecum, J. M., Wang, M. Z., Hsu, Y. M., Zheng, T. S., Michaelson, J. S., Liao, R., and Burkly, L. C. (2009) A novel role for tumor necrosis factor-like weak inducer of apoptosis (TWEAK) in the development of cardiac dysfunction and failure. Circulation 119, 2058-2068
45. Chorianopoulos, E., Heger, T., Lutz, M., Frank, D., Bea, F., Katus, H. A., and Frey, N. (2010) FGF-inducible 14-kDa protein (Fn14) is regulated via the RhoA/ROCK kinase pathway in cardiomyocytes and mediates nuclear factor-kappaB activation by TWEAK. Basic Res Cardiol 105, 301-313
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
13
46. Fu, X. X., Zhao, N., Dong, Q., Du, L. L., Chen, X. J., Wu, Q. F., Cheng, X., Du, Y. M., and Liao, Y. H. (2015) Interleukin-17A contributes to the development of post-operative atrial fibrillation by regulating inflammation and fibrosis in rats with sterile pericarditis. Int J Mol Med 36, 83-92
47. Liu, Y., Zhu, H., Su, Z., Sun, C., Yin, J., Yuan, H., Sandoghchian, S., Jiao, Z., Wang, S., and Xu, H. (2012) IL-17 contributes to cardiac fibrosis following experimental autoimmune myocarditis by a PKCbeta/Erk1/2/NF-kappaB-dependent signaling pathway. Int Immunol 24, 605-612
48. Valente, A. J., Yoshida, T., Gardner, J. D., Somanna, N., Delafontaine, P., and Chandrasekar, B. (2012) Interleukin-17A stimulates cardiac fibroblast proliferation and migration via negative regulation of the dual-specificity phosphatase MKP-1/DUSP-1. Cell Signal 24, 560-568
49. Weaver, C. T., Hatton, R. D., Mangan, P. R., and Harrington, L. E. (2007) IL-17 family cytokines and the expanding diversity of effector T cell lineages. Annu Rev Immunol 25, 821-852
50. Papachroni, K. K., Piperi, C., Levidou, G., Korkolopoulou, P., Pawelczyk, L., Diamanti-Kandarakis, E., and Papavassiliou, A. G. (2010) Lysyl oxidase interacts with AGE signalling to modulate collagen synthesis in polycystic ovarian tissue. J Cell Mol Med 14, 2460-2469
51. Chung, K. Y., Agarwal, A., Uitto, J., and Mauviel, A. (1996) An AP-1 binding sequence is essential for regulation of the human alpha2(I) collagen (COL1A2) promoter activity by transforming growth factor-beta. J Biol Chem 271, 3272-3278
52. Sakamuri, S. S., Higashi, Y., Sukhanov, S., Siddesha, J. M., Delafontaine, P., Siebenlist, U., and Chandrasekar, B. (2016) TRAF3IP2 mediates atherosclerotic plaque development and vulnerability in ApoE-/- mice. Atherosclerosis
53. DeSelm, C. J., Takahata, Y., Warren, J., Chappel, J. C., Khan, T., Li, X., Liu, C., Choi, Y., Kim, Y. F., Zou, W., and Teitelbaum, S. L. (2012) IL-17 mediates estrogen-deficient osteoporosis in an Act1-dependent manner. J Cell Biochem 113, 2895-2902
54. Jia, G., Habibi, J., DeMarco, V. G., Martinez-Lemus, L. A., Ma, L., Whaley-Connell, A. T., Aroor, A. R., Domeier, T. L., Zhu, Y., Meininger, G. A., Barrett Mueller, K., Jaffe, I. Z., and Sowers, J. R. (2015) Endothelial Mineralocorticoid Receptor Deletion Prevents Diet-Induced Cardiac Diastolic Dysfunction in Females. Hypertension 66, 1159-1167
55. Nagalla, K. T., Gole, M., Claudino, M. A., Gardner, J. D., and Murray, D. B. (2012) Alteration in myocardial prostaglandin D synthase expression in pressure overload-induced left ventricular remodeling in rats. Exp Biol Med (Maywood) 237, 24-30
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
14
FOOTNOTES
BC is a recipient of the Department of Veterans Affairs Research Career Scientist award, and the work was supported by the U.S. Department of Veterans Affairs, Office of Research and Development-Biomedical Laboratory Research and Development (ORD-BLRD) Service Award I01-BX002255. TY is funded by the American Heart Association Scientist Development grant (15SDG25240022) and the University of Missouri, Department of Medicine Research Council R&D Award. US is supported by the Intramural Research Program of the NIH/NIAID. The contents of this report do not represent the views of the Department of Veterans Affairs or the United States government.
The abbreviations used are: ANP, atrial natriuretic peptide; BNP, brain natriuretic peptide; CTGF, connective tissue growth factor; FS, fractional shortening; LOX, lysyl oxidase; LVESD, LV end systolic diameter; LVEDD, LV end diastolic diameter; MKP-1, mitogen-activated protein kinase phosphatase-1; MRI, magnetic resonance imaging; α-SMA, α-smooth muscle actin; TRA3IP2, TRAF3 Interacting Protein 2; WGA, wheat germ agglutinin.
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
15
TABLES Table 1: Anatomic and functional parameters in 2 month-old TRAF3IP2-Tg and control non-transgenic (NTg) littermates. n, number of mice; LVID;d, left ventricular (LV) internal diameter in diastole; LVIDs, LV internal diameter in systole; LVAWd, LV anterior wall diameter in diastole; LVPWd, LV posterior wall diameter at diastole; EF, ejection fraction; FS, fractional shortening; LVEDV, LV end diastolic volume; LVESV, LV end systolic volume; EDP, end diastolic pressure; ESP, end systolic pressure; CO, cardiac output; IFR, initial filling rate; RT, retention time; PER, peak ejection rate; PFR, peak filling rate; SV, stroke volume; Results represent the mean ± SEM, and are considered statistically significant if p < 0.05.
NTg TRAF3IP2-Tg P value Anatomic data n 6 6 Body weight (g) 25.45 ± 0.75 26.10 ± 0.9 0.7 Heart weight (mg) 109.10 ± 3.56 131.5 ± 3.95 0.001 Heart weight/body weight (mg/g) 4.287 ± 0.06 5.038 ± 0.09 0.001 Cardiomyocyte Cross-sectional area (µm2) 303.0 ± 17.45 451.1 ± 24.0 0.0005
Functional data Echocardiography n 5 5 LVID;d (mm) 3.24 ± 0.06 3.14±0.12 0.5 LVIDs (mm) 2.730 ± 0.044 2.455 ± 0.08 0.01 LVAWd (mm) 1.043 ± 0.01 1.178±0.06 0.06 LVPWd (mm) 0.9983 ± 0.07 1.22 ± 0.03 0.01 EF (%) 61.64 ± 2.95 51.32 ± 2.21 0.02 FS (%) 32.78 ± 2.18 25.75 ± 1.37 0.03 Cine-MRI n 6 4 Septal wall thickness (mm) 0.928 ± 0.03 1.18 ± 0.01 0.002 LVEDV (µl) 50.1 ± 2.6 48.2 ± 1.4 0.59 LVESV (µl) 23.1 ± 2.4 26.5 ± 1.1 0.31 SV (µl) 27.0 ± 0.9 21.7 ± 0.3 0.001 CO (ml/min) 10.5 ± 0.4 8.0 ± 0.02 0.002 EF (%) 54.5 ± 2.6 45.0 ± 0.7 0.02 PER (µl/ms) 0.6 ± 0.03 0.49 ± 0.02 0.02 PFR (µl/ms) 0.79 ± 0.06 0.77 ± 0.08 0.90 IFR (µl/ms) 0.27 ± 0.05 0.19 ± 0.04 0.29 RT (ms) 28.15 ± 3.71 34.42 ± 2.32 0.24 Pressure volume conductance catheter n 4 4 ESP (mmHg) 55.37 ± 1.12 52.15 ± 1.08 0.08 EDP (mmHg) 2.604 ± 0.19 1.939 ± 0.34 0.14 ESV (µl) 25.56 ± 0.65 28.24 ± 1.22 0.001 EDV (µl) 40.67 ± 3.27 34.93 ± 2.90 0.21 SV (µl) 56.15 ± 3.02 43.81 ± 2.31 0.007 CO (ml/min) 28.54 ± 1.35 22.67 ± 0.67 0.0009 EF (%) 62.73 ± 1.42 56.17 ± 0.83 0.006 Heart rate (beats/min) 481.1 ± 14.77 573.0 ± 22.68 0.07
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
16
Table 2: Functional parameters by echocardiography in 2 month-old female TRAF3IP2-Tg and NTg mice. Results represent the mean ± SEM (n=5/group), and are considered statistically significant if p < 0.05.
Parameters Female NTg Female TRAF3IP2-Tg
P value
LVID;d (mm) 3.238 ± 0.068 3.14±0.12 0.49 LVID;s (mm) 2.367±0.109 2.243±0.06
0.35 LVAW;d (mm) 1.043±0.017 1.178±0.06
0.06 LVPW;d (mm) 1.152±0.035 1.250±0.04 0.10 LVAW;s (mm) 1.312±0.034 1.338±0.04 0.63 EF (%) 56.51±1.026 57.26±4.6 0.87 FS (%) 28.61±0.644 29.41±3.2 0.81
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
17
Table 3: Protein Quantibody Array data showing changes in protein levels of various proinflammatory mediators in LV homogenates from 2 month-old male and female TRAF3IP2-Tg mice. Results are expressed as a fold change in the Tg compared to corresponding NTg littermates. Proteins that showed a 1.5 fold change or more are depicted. é and ê indicate up- or down-regulation, respectively. G-CSF, granulocyte-colony stimulating factor; MCSF, macrophage-colony stimulating factor; TWEAK, TNF related weak inducer of apoptosis; TWEAKR, TWEAK receptor; BLC, B-lymphocyte chemoattractant; MAdCAM-1, mucosal vascular addressin cell adhesion molecule 1; VCAM-1, vascular cell adhesion molecule 1; β-FGF, basic fibroblast growth factor; ACE, angiotensin converting enzyme.
Protein Male Tg (n=4/group) Female Tg (n=4/group) Inflammation Fold change P value Fold change P value Cytokines G-CSF 2.5é 0.0086 1.0 0.5528 IL-6 2,0é 0.0019 1.2 0.1424 IL-17A 5.6é 0.0260 1.2 0.7651 IL-17B 3.0é 0.0009 2.0é 0.2817 IFN-γ 1.8é 0.2533 1.0 0.9083 Lipocalin-2 5.0é 0.0017 1.4ê 0.0301 MCSF 2.5é 0.0421 2.0ê 0.0328 Meteorin 6.7é 0.0016 2.3ê 0.0016 TNF-α 3.5é 0.0046 4.0ê 0.0024 TWEAK 2.7é 0.1273 1.2 0.6184 TWEAKR 3.0é 0.0225 3.0é 0.0418 P-selectin 1.5é 0.0872 1.7ê 0.0750 Chemokines BLC 7.0é 0.0055 1.0 0.7327 CCL5 3.0é 0.0235 1.0 0.1933 Fractalkine 2.0é 0.0426 2.0ê 0.1591 6Ckine 8.0é 0.0360 2.0é 0.0228 Adhesion molecules E-selectin 1.8é 0.1116 1.0 0.3592 ICAM-1 2.0é 0.0248 1.0 0.9876 MAdCAM-1 2.5é 0.0468 1.0 0.8883 P-cadherin 4.0é 0.0004 1.5ê 0.0513 Periostin 2.4é 0.0118 1.1 0.2924 VCAM-1 2.7é 0.0009 2.5é 0.0124 Fibrosis Cytokines β-FGF 1.6é 0.0039 1.8é 0.0015 ECM modulating proteins Testican 8.0é 0.0001 1.0 0.7526 Galectin-7 3.3ê 0.0277 1.4 0.6985 MMP-3 1.6é 0.2659 2.0é 0.0546 MMP-10 2.5é 0.2119 1.0 0.3743 Hypertension ACE 1.7é 0.0062 1.1 0.4594 Ang-III 2.4é 0.0026 1.2 0.6125 Renin-3 5.0é 0.0019 4.0é 0.0040
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
18
FIGURE LEGENDS
FIGURE 1. Generation of transgenic mice with cardiomyocyte-specific overexpression of TRAF3IP2 (TRAF3IP2-Tg). A, The vector map of α-MyHC-mTRAF3IP2. N: NotI; B: BamHI; S: SalI. F and R indicate the binding region of forward and reverse PCR primers that detect an overlapping region of 600 bp. B, Electrophoresis of a purified Not1 digested fragment of α-MyHC-mTRAF3IP2-hGH poly A (7.8 kbp). C, Southern blot analysis of wild type (WT) and TRAF3IP2-Tg mice. Genomic DNA of WT and Tg mice were digested with EcoRV and KpnI, and probed with TRAF3IP2 ORF. The predicted band sizes of TRAF3IP2 WT allele are 13.8 and 14.3 kbp after EcoRV and KpnI digestion, respectively (black arrowheads). Tg mice showed two bands after digestion (red arrowheads), indicating that two copies of the transgene were inserted into the Tg mouse genome. D, Genotyping was carried out using genomic DNA isolated from tail snips from male and female Tg and control non-transgenic (NTg) littermates. ‘*’ denotes transgene with an amplicon size of ~600bp.
FIGURE 2. Characterization of TRAF3IP2-Tg mice. A, B, TRAF3IP2 mRNA (A) and protein expression (B) in LV tissues of 2 month-old male Tg and NTg mice analyzed by RT-qPCR and immunoblotting. Each lane in panel B represents an individual animal. Densitometric analysis of immunoreactive bands in panel B is summarized on the right. C, D, Tissue specificity of transgene-derived TRAF3IP2 overexpression was analyzed by immunoblotting (N: NTg, T: Tg). Densitometric analysis of immunoreactive bands is summarized in D. E, Immunofluorescence analysis of TRAF3IP2 overexpression in the heart co-localized with wheat germ agglutinin (WGA). Scale: 50 µm. TRAF3IP2 overexpression is localized predominantly to cardiomyocytes (CM), but not endothelial or smooth muscle cells of blood vessels (BV). Intensity of TRAF3IP2 immunofluorescence signals were quantified and summarized on the right. F, G, TRAF3IP2 overexpression induces activation of IKKβ, p65, JNK, c-Jun, c/EBPβ and p38 MAPK in LV tissues from male (F, Densitometric analysis of immune-reactive bands is summarized on the right), but not female Tg (G) as analyzed by immunoblotting using activation-specific antibodies. n=4/group, Error bars represent SEM. * p < at least 0.05 vs. corresponding NTg.
FIGURE 3. Evaluation of cardiac function in TRAF3IP2-Tg and NTg mice at 2 months of age by transthoracic echocardiography and cine-MRI. A, A representative M-mode tracing showing anterior wall (AW), internal diameter (ID) and posterior wall (PW). B, B-mode tracings showing epicardium (Ep), endocardium (En) and LV chamber (c). C, Structural and functional parameters derived from M- and B-mode tracings (n=6/group). D, Representative mid-ventricle short-axis cine-MRI images corresponding to the end-diastole and end-systole cardiac phases are shown (n=4-6/group). S, septal wall. Error bars represent SEM. *p < 0.05 vs. NTg littermates.
FIGURE 4. Transgenic overexpression of TRAF3IP2 results in spontaneous development of myocardial hypertrophy. A, Gross morphology of the heart (upper panel) and heart weight (HW) to body weight (BW) ratios (lower panel) in 2 month-old NTg and Tg mice. B, Cardiomyocyte cross-sectional area was analyzed using WGA-stained heart sections. Scale: 50 µM. The mean area of cardiomyocytes was quantified and summarized on the right. C, mRNA expression of fetal genes (ANP, BNP and β-MyHC) in LV tissues as analyzed by RT-qPCR. 18S served as an internal control. D, Protein expression of fetal genes and GATA4 was analyzed by immunoblotting. Densitometric analysis of immunoreactive bands is summarized on the right. E, Temporal changes in HW/BW ratios. F, ANP and GATA4 expression in female Tg hearts (n=4/group). Error bars represent SEM. *p < 0.05, **p < 0.01, ***p < 0.001 vs. NTg littermates.
FIGURE 5. Transgenic overexpression of TRAF3IP2 results in spontaneous development of cardiac fibrosis. A, mRNA expression of ColIα1, ColIIIα1 and CTGF in LV tissues of 2 month-old Tg and NTg mice as analyzed by RT-qPCR (18S served as an internal control). B, Protein levels of ColIα1, ColIIIα1, LOX, and CTGF in LV tissues from Tg and NTg mice as analyzed by immunoblotting. Densitometric analysis of immunoreactive bands is summarized on the right. C, Deposition and co-localization of
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
19
ColIα1 and ColIIIα1 were analyzed in LV tissues from Tg and NTg mice by immunofluorescence. Relative fluorescent signals were quantified and summarized on the right. D, Temporal changes in cardiac fibrosis as analyzed by Masson trichrome staining. Mean collagen positive area is summarized on the right (n=4/group). Error bars represent SEM. *p < at least 0.05 vs. NTg littermates.
FIGURE 6. Transgenic overexpression of TRAF3IP2 results in cardiac fibroblast activation. A, Co-localization of CD-31 and α-SMA in hearts of 2 month-old male NTg and Tg mice. Mean fluorescent intensities were quantified and summarized on the right. B, Co-localization of tensin and α-SMA. Mean fluorescent intensities were quantified and summarized on the right. C, Co-localization of paxillin and α-SMA. Mean fluorescent intensities were quantified and summarized on the right. BV, blood vessels, n=4/group. Error bars represent SEM. *p < 0.05, **p < 0.005 vs. NTg littermates.
FIGURE 7. Transgenic overexpression of TRAF3IP2 results in spontaneous induction of pro-inflammatory cytokines and macrophage infiltration. A, mRNA and B, protein expression of IL-6 and IL-18 as analyzed by RT-qPCR and immunoblotting, respectively. The immunoreactive bands in B were semiquantified and summarized on the right. C, Macrophage infiltration into heart tissues was analyzed by Mac3 staining and the fluorescence signals are summarized on the right. Scale: 100 µM. Inset shows a 60X magnification. n=4/group. Error bars represent SEM. *p < at least 0.05 vs. NTg littermates.
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
20
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
21
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
22
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
23
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
24
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
25
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

TRAFIP2 in adverse cardiac remodeling
26
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from

Ma, Ulrich Siebenlist, Jason D. Gardner and Bysani ChandrasekarSiva S. V. P. Sakamuri, Jalahalli M. Siddesha, Sergiy Sukhanov, Zubaida Saifudeen, Lixin Manjunath Yariswamy, Tadashi Yoshida, Anthony J. Valente, Hemanth Kumar Kandikattu,
DysfunctionResults in Spontaneous Development of Myocardial Hypertrophy, Fibrosis and
Cardiac-Restricted Overexpression of TRAF3 Interacting Protein 2 (TRAF3IP2)
published online July 27, 2016J. Biol. Chem.
10.1074/jbc.M116.724138Access the most updated version of this article at doi:
Alerts:
When a correction for this article is posted•
When this article is cited•
to choose from all of JBC's e-mail alertsClick here
by guest on October 28, 2020
http://ww
w.jbc.org/
Dow
nloaded from
Related Documents