Article 1 Formulation and Evaluation of Minoxidil Gel for 2 Alopecia areata 3 Pawan kumar 1 , Shailendra Kumar Singh 1* , Deepak Kumar Jindal 1 , Vandana Handa 2 4 5 1 Department of Pharmaceutical sciences, Guru Jambheshwar University of science & Technology, Hisar 6 125001, India 7 2 School of Pharmacy, Krishna Institute of Engineering and Technology, Ghaziabad, India 201206 8 * Correspondence: [email protected]; Tel.: +919416473355; Fax: +911662276240. 9 10 11 Abstract: Alopecia areata is a common, chronic inflammatory disease, characterized by patchy hair 12 loss on the scalp, affecting about 2.1% of world population. Minoxidilhas been used for treatment 13 of alopecia as topical lotion. However, this dosage form has been associated with many drawbacks 14 like systemic side effects and low contact time to skin. Therefore, in the present work, minoxidil gel 15 was prepared using a novel copolymer, Sepineo P 600 to overcome these drawbacks. In the present 16 work, minoxidil gel was cahararecterised for pH, drug content, viscosity, spreadability, skin 17 adhesivity, occlusivity, in vitro drug release, ex vivo skin permeation, stability and finally for skin 18 corrosivity. The drug content of the finalized gel was found to be 99.80±0.82%. The formulation 19 showed good spreadability, occlusivity, adhesiveness and viscosity. In vitro release studies showed 20 that the drug release from prepared gel followed matrix release pattern as compared to lotion. 21 Mathematical modeling of the drug release data suggested that it followed Higuchi model. The 22 formulated minoxidil gel was found to be non-corrosive and stable when subjected to accelerated 23 as well as real time stability studies. Overall, it the minoxidil gel formulation was suitable for skin 24 application and can be an effective dosage form for the treatment of Alopecia areata. 25 Keywords: Minoxidil; Skin permeation; Sepineo gel 26 27 1. Introduction 28 Alopecia areata (AA) is a recurrent, genetic, immune mediated disease that affects 2.1% of 29 population including children and adults, characterized as patches of hair loss to total hair loss of 30 scalp hair (alopecia totalis) or loss of entire scalp and body hair (alopecia universalis) [1]. Although 31 the etiology of AA is poorly understood, but the number of factors such as genetics, stress, 32 hormones, diet, infectious agents, vaccination, etc. determine the physical and biochemical status of 33 the immune system and hair follicles. It is also known that T- lymphocytes play an important role in 34 AA infiltrating against the hair follicles leading to abrupt conversion from anagen to telogen phase 35 [2]. Minoxidil (MXD), an antihypertensive drug, appears to be effective in the treatment of AA by 36 prolonging the anagen phase and increasing the size of smaller hair follicles [3]. Presently, MXD is 37 available as 2%w/v and 5%w/v topical solution in market. But commercial MXD formulations 38 contain high percentage of ethanol and propylene glycol and their repeated application leads to 39 severe adverse effects such as scalp dryness, irritation, burning sensation, redness and allergic 40 contact dermatitis [4,5]. Other drawbacks associated with topical MXD solutions includes less 41 contact time with the application area and high systemic absorption of drug resulting cardiovascular 42 side effects [6,7]. Therefore, to resolve these drawbacks, new formulation was required to develop in 43 the form of gel which can provide sufficient contact time and capable of sustain drug delivery. Gels 44 are transparent or translucent semisolid dosage form produced by entrapment of large amounts of 45 Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 25 September 2017 doi:10.20944/preprints201709.0123.v1 © 2017 by the author(s). Distributed under a Creative Commons CC BY license.

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

Article 1
Formulation and Evaluation of Minoxidil Gel for 2
Alopecia areata 3
Pawan kumar1, Shailendra Kumar Singh1*, Deepak Kumar Jindal1, Vandana Handa2 4 5 1 Department of Pharmaceutical sciences, Guru Jambheshwar University of science & Technology, Hisar 6
125001, India 7 2 School of Pharmacy, Krishna Institute of Engineering and Technology, Ghaziabad, India 201206 8 * Correspondence: [email protected]; Tel.: +919416473355; Fax: +911662276240. 9 10 11
Abstract: Alopecia areata is a common, chronic inflammatory disease, characterized by patchy hair 12 loss on the scalp, affecting about 2.1% of world population. Minoxidilhas been used for treatment 13 of alopecia as topical lotion. However, this dosage form has been associated with many drawbacks 14 like systemic side effects and low contact time to skin. Therefore, in the present work, minoxidil gel 15 was prepared using a novel copolymer, Sepineo P 600 to overcome these drawbacks. In the present 16 work, minoxidil gel was cahararecterised for pH, drug content, viscosity, spreadability, skin 17 adhesivity, occlusivity, in vitro drug release, ex vivo skin permeation, stability and finally for skin 18 corrosivity. The drug content of the finalized gel was found to be 99.80±0.82%. The formulation 19 showed good spreadability, occlusivity, adhesiveness and viscosity. In vitro release studies showed 20 that the drug release from prepared gel followed matrix release pattern as compared to lotion. 21 Mathematical modeling of the drug release data suggested that it followed Higuchi model. The 22 formulated minoxidil gel was found to be non-corrosive and stable when subjected to accelerated 23 as well as real time stability studies. Overall, it the minoxidil gel formulation was suitable for skin 24 application and can be an effective dosage form for the treatment of Alopecia areata. 25
Keywords: Minoxidil; Skin permeation; Sepineo gel 26 27
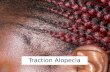
1. Introduction 28 Alopecia areata (AA) is a recurrent, genetic, immune mediated disease that affects 2.1% of 29
population including children and adults, characterized as patches of hair loss to total hair loss of 30 scalp hair (alopecia totalis) or loss of entire scalp and body hair (alopecia universalis) [1]. Although 31 the etiology of AA is poorly understood, but the number of factors such as genetics, stress, 32 hormones, diet, infectious agents, vaccination, etc. determine the physical and biochemical status of 33 the immune system and hair follicles. It is also known that T- lymphocytes play an important role in 34 AA infiltrating against the hair follicles leading to abrupt conversion from anagen to telogen phase 35 [2]. Minoxidil (MXD), an antihypertensive drug, appears to be effective in the treatment of AA by 36 prolonging the anagen phase and increasing the size of smaller hair follicles [3]. Presently, MXD is 37 available as 2%w/v and 5%w/v topical solution in market. But commercial MXD formulations 38 contain high percentage of ethanol and propylene glycol and their repeated application leads to 39 severe adverse effects such as scalp dryness, irritation, burning sensation, redness and allergic 40 contact dermatitis [4,5]. Other drawbacks associated with topical MXD solutions includes less 41 contact time with the application area and high systemic absorption of drug resulting cardiovascular 42 side effects [6,7]. Therefore, to resolve these drawbacks, new formulation was required to develop in 43 the form of gel which can provide sufficient contact time and capable of sustain drug delivery. Gels 44 are transparent or translucent semisolid dosage form produced by entrapment of large amounts of 45
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 25 September 2017 doi:10.20944/preprints201709.0123.v1
© 2017 by the author(s). Distributed under a Creative Commons CC BY license.

2 of 10
aqueous or hydro-alcoholic liquid in a three dimensional colloidal network that are often employed 46 in topical delivery to prolong contact time of drug and to facilitate application on the skin [8]. In 47 recent years, there has been great interest in the use of Sepineo P 600, a novel polymers with complex 48 functions [9]. 49
Therefore, in the present study, an attempt has been made to prepare and evaluate the hydrogel 50 containing MXD at the same therapeutic concentration used in commercial product (2% w/v) by 51 using self gelling agent Sepineo P 600. The rheology, spreadability, in vitrodrug release, bioadhesion 52 strength, ex vivo skin permeation and skin corrosivity of the prepared gel were also evaluated. 53
54
2. Materials and Methods 55
2.1. Materials 56 Minoxidil was received as a gift sample from Zee laboratories Ltd., Baddi, India. Sepineo P 600 57
(concentrated dispersion of acrylamide/sodium acryloyldimethyltaurate copolymer in 58 isohexadecane) was received as a kind gift sample from Seppic (India). Propylene glycol was 59 purchased from Sigma-Aldrich, Mumbai, India. Dialysis membrane (Molecular weight cut off 14000 60 Da) was purchased from Hi-Media, Mumbai, India. All other chemicals were of the analytical grade. 61
2.2. Preparation of gel formulations 62 For the preparation of gel (MXD-Gel), the drug was dissolved in small amount of propylene 63
glycol then gelled by adding a self-gelling and thickening agent Sepineo P 600 (1%, 2% and 3% w/v) 64 using a high speed stirrer at 1000 rpm for 5 min. Similarly, blank gel (B-Gel) was formulated without 65 adding drug. Three different concentration of gelling agent wereused to optimize the 66 formulationviscosity . The formulated gel wereleft for equilibratinon for 24 h at room temperature 67 (25±1 ºC) to remove entrapped air. For MXD lotion (MXD-Lotion), drug was added and dissolved to 68 a solvent mixture (ethanol: propylene glycol: water in the ratio of 50:30:20). 69
2.3. Drug content and pH 70 To quantify the amount of drug in the formulation, 500 mg MXD-Gel was dissolved in 50 ml of 71
phosphate buffer (pH 7.4) in a 100 ml volumetric flask with continuous shaking. Later, it was 72 analyzed after appropriate dilution using UV-visible spectrophotometer (Varian Cary-5000, 73 Netherlands) at λmax 231 nm. The digital pH meter (pH Tutor Bench Meter, EUTECH Instruments, 74 Singapore) was used to measure the pH of the gel [10]. 75
2.4. Occlusion factor 76 For the determination of occlusive properties of MXD-Lotion, B-Gel and MXD-Gel, previously 77
reported method was used [11]. In brief, 50 ml water was added into a beaker (capacity 100 ml) and 78 covered with a filter paper (Whatman number 6). 200 mg of test formulations were applied on the 79 surface (area 12.56 cm2) of filter paper (test) and compared with the similar beaker having filter 80 paper without formulation (control) by storing at 32 ± 0.5 °C for 24 h. Weight of water remaining in 81 the beakers was measured after 24 h to calculate the occlusion factor. Following equation was used 82 to calculate the occlusion factor (F) 83
= (A 100 84 Where A = water loss with blank (control) and B = water loss with sample. 85 If, F = 0 means no occlusive effect, F = 100 maximum occlusion factor 86
2.5. Rheological measurements 87 The viscosity of the B-Gel and MXD-Gel samples were measured by Brookfield viscometer 88
(RVT, Brookfield Engineering Laboratories, Inc., USA) using spindle ≠2 at rotational speed of 0.5, 1.0, 89
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 25 September 2017 doi:10.20944/preprints201709.0123.v1

3 of 10
2.0, 5, 10, 25, 50 and 100 rpm. The flow property of the gels weremeasured by recording the variation 90 in shear stress (τ) by increasing and then decreasing the shear rate (rpm) from 0 to 100 rpm at 91 temperature of 25 ± 1ºC [12]. 92
2.6. Spreadability study 93 The spreadability of the gels were used to measure the extent of area of application to which 94
formulation readily spreads to skin. To assess spreading ability, weighed cellulose acetate filter 95 paper (W1) was placed in the center of the aluminum foil sheet. 20 drops of test formulation was 96 added over the defined area of the cellulose acetate filter paper using 5 ml syringe (Becton Dickinson 97 & Co., USA). After 10 min, saturated portion of the filter paper was cut away from the unsaturated 98 portion. Unsaturated portion of the filter paper (W2) was weighed and spreadability was calculated 99 using the following equation . 100 ℎ = ( ) × 100 101
2.7. Skin Adhesion Test 102 The modified Patel et al (2007) [13] method was used to measure the bioadhesive strength of 103
prepared gel with excised pig ear skin. Two arm balance was used in which left arm was tied with 104 one glass slide having the skin and other glass slide with skin was fixed on the wooden block. The 105 right and left pans were balanced by adding extra weight to the right pan. 1 gm of the prepared gel 106 was sandwiched between these two slides by the application of small pressure to remove air bubbles 107 and kept for 5 minutes. Weight was added to the right pan slowly at 50 mg/ min till the patch 108 detached from the skin surface. Bioadhesive strength was measured as the weight (gram force) 109 required detaching the gel from the skin surface [14] and calculated using the formula. 110 − ℎ ℎ = ℎ ( ) / ( 2) 111
2.8. In vitro drug release 112 The in vitro release of drug from MXD-gel was performed on Franz Diffusion Cell using dialysis 113
membrane. The membrane was mounted between the donor and receptor compartments of a locally 114 fabricated Franz diffusion cells (diffusion area of 0.785 cm2; receptor volume of 5.5 ml). Mixture of 115 phosphate buffer solution pH 7.4 and ethanol (60:40 v/v) was used as receptor medium maintained 116 at 37 ± 0.5 °C. Defined amount of formulation was then placed on the surface of the membrane in the 117 donor compartment. The aliquots from the receptor compartment were withdrawn at 118 predetermined time interval (0.5, 1, 2, 3, 6, 12 and 24 h) and replaced with an equal volume of fresh 119 medium. The samples were analyzed for drug content by UV-visible spectrophotometer (Varian 120 Cary-5000, Netherlands) at λmax 231 nm. To study the mechanism of MXD release from gel 121 formulation, the data obtained from in vitro release studies was fitted to different kinetic models 122 (Zero order, First order, Higuchi and KorsmeyerPeppas). The criterion for selecting the most 123 appropriate model was based on a goodness- of-fit test [15]. 124
2.9. Ex vivo skin permeation study 125 Franz diffusion cell (diffusion area 0.785 cm2) was used for permeation study. Fresh hairless full 126
thickness pig ear skin from dorsal region was obtained from local slaughterhouse. The skin was 127 washed under tap water followed by drying with tissue paper. Skin specimen was mounted on 128 Franz diffusion insuch a way that stratum corneumdonor while dermal side facingthe receiver 129 compartments[16]. The receptor compartment was filled with 6.0 ml phosphate buffer pH7.4and 130 maintained at 37 ± 1°C throughout the experiment under continuous stirring. After equilibrium, 131 specified amount (how much?) of MXD-Gel was added to donor compartment. Aliquots (1.0 ml) 132 were withdrawn from the receptor compartment at an interval 0.5, 1, 2, 3, 6, 12 and 24 h and 133 analyzed for drug content uisingUV-Visible spectrophotometer at 231 nm [17]. The receptor phase 134 was immediately replenished with equal volume of fresh buffer after each sample withdrawal. 135
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 25 September 2017 doi:10.20944/preprints201709.0123.v1

4 of 10
2.10. Stability Studies 136 MXD-Gel was subjected to two different conditions 30 ± 2 °C, 65 ± 5?%relative humidity (RH) 137
and 40 ± 2°C, 75 ± 5 ?%RH for 3 months as per ICH guidelines (Q1AR2) of stability testing 138 using stability chamber (NewtronicLifecare Equipment Pvt. Ltd, Mumbai, India). The sampling was 139 done at the end 1st, 2nd and 3rd month to measure the pH, drug content and viscosity [18,19]. 140
2.11. Ex vivo skin corrosion studies 141 Corrositex® test was performed to determine the corrosive potential of gel containing MXD. The 142
corrosive product act by irreversibly damaging epidermal proteins and show color shift in an 143 underlying chemical detection liquid. Pig ears skin was used for this study obtained from a local 144 slaughter house. The skin was washed under tap water and the full thickness skin was carefully 145 removed from the dorsal/external region of the pig ears. The prepared pig ear skin was clamped on 146 Franz- diffusion cells. 37% nitric acid solution (positive control) and 0.9% NaCl solution (negative 147 control) was used for the experiment. 200 µl of test formulation and both positive and negative 148 control was applied on pig ear skin. After 15 min, these formulations were removed followed by 149 washing with 2×1 ml of distilled water to remove the residual sample from the epidermis. Then, 1ml 150 of sulforhodamine B was applied on the epidermis of above used skin to detect the protein 151 destruction. The applied dye was removed after another 15 min and washed the epidermis with 1 ml 152 of distilled water. Analyze this washed water using UV-visible spectrophotometer (Varian 153 Cary-5000, Netherlands) at λmax 265.5 nm [20]. The study was performed six times and the value of 154 corrosive factor F was measure by given equation, when, F >0 (non corrosive) and F < 0 (corrosive 155 sample). 156 F = Absorbance of sample − Absorbance of 0.9%NaclAbsorbance of 0.9%Nacl 157
2.12. Statistical analysis 158 All the results were statistically evaluated using one way analysis of variance with post-hoc 159
Tukey'stest ; pvalue less than 0.05 was considered as statistically significant. 160
3. Results 161
3.1. Preparation of MXD-Gel 162 MXD-Gel containing 1.0 % of Sepineo P 600 form a very thin gel that liquefies within 6 h of 163
preparation, while 3.0 % of gel formulation was very thick and more sticky that could not be 164 properly spread out. Gel containing 2.0% of Sepineo P 600 formed uniform and smooth gel that does 165 not liquefy upon keeping. Thus, 2.0% concentration of gelling agent was selected as the optimized 166 concentration. 167
3.2. Drug content and pH 168 The amount of drug present in MXD-Gel was found to be 99.80± 0.82% and pH was found to be 169
6.29± 0.18. 170
3.3. Occlusion studies 171 The value of occlusion factor [Figure 1(A)] of MXD-Lotion, B-Gel and MXD-Gel after 24 h was 172
found to be 31.40, 49.88 and 50.92, respectively. MXD-Gel and B-Gel cannot exhibits any significant 173 difference in occlusivity (p> 0.05). 174
175 176
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 25 September 2017 doi:10.20944/preprints201709.0123.v1

5 of 10
177
178 179 Figure 1 Occlusion factor (A) and Adhesion strength (B) of MXD-Lotion, blank gel (B-Gel), 180
minoxidil loaded gel (MXD-Gel); Flow curves of blank gel (C) and minoxidil loaded gel (D). 181 (ab,acp<0.05, bcp>0.05) 182
183
184 Figure 2 Stability study on accelerated condition (A) and Real time (B) for final gel. 185 186
3.4. Rheological behavior 187
A B
A B
DC
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 25 September 2017 doi:10.20944/preprints201709.0123.v1

6 of 10
The viscosity of gel formulations reflects the spreadability and adherence of transdermal 188 formulations to the skin surface [21]. The viscosity of blank gel and final gel [189
190 Figure 2] increased with increasing rate of shear with superimposed ascending and descending 191
flow curves of the rheogram showed Newtonian flow behavior. The flow curves were unaffected 192 (p>0.5) by the presence of drug. 193
3.5. Spreadability 194 The finalized formulation has approximately equal spread by weight 61.11± 1.18% compared to 195
blank gel 61.47±1.12%. The presence of drug in gel had not affected the spreadability of the 196 formulation (p>0.5). 197
3.6. Skin Adhesion Test 198 The value of adhesiveness for MXD-Lotion is 12.73, B-Gel is 70.06 and MXD-Gel was 82.80. The 199
adhesiveness of MXD-Gel was found to be greater than MXD-Lotion as shown in Figure 1, which 200 may be due to reduction in the solvent and increased coiling of the polymer chain. 201
3.7. In vitro drug release 202 In the present study, the gel formulation released MXD over a prolonged period of 24 h across 203
dialysis membrane compared to topical lotion as reference [Figure 1]Error! Reference source not 204 found.. The regression coefficient (R2) of MXD-Gel for different release kinetics equations are shown 205 in 206
Table 1. 207 208 Table 1Regression coefficient (R2) obtained from various kinetics models 209 210
Formulation Zero Order
Kinetics Higuchi Kinetics
Korsmeyer Peppas Kinetics
First Order Kinetics
MXD-Gel 0.896 0.994 0.953 0.786
211
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 25 September 2017 doi:10.20944/preprints201709.0123.v1

7 of 10
212 Figure 3 In vitro drug release study (A) and ex vivo permeation study (B) after 24 h. Data 213 presented as mean ± SEM. 214
3.8. Ex vivo skin permeation study 215 Figure 1 (D) shows permeation of MXD from MXD-Lotion and MXD-Gel across the pig skin 216
barrier. Significant difference was found between cumulative MXD flux of lotion (34.50 ± 2.22 217 mcg/cm2/h) and gel (7.60 ± 1.55 mcg/cm2/h) formulation. 218
3.9. Stability studies 219 There were no significant changes in the viscosity, drug content and pH of the final gel 220
formulation after storing at 30 ± 2°C and 40 ± 2°C at 65 ± 5 and 75 ± 5 RH for 3 months as shown in 221 Figure 2 and Figure 2 respectively. 222
3.10. Ex vivo skin corrosion studies 223 The MXD-Gel was found to be non-corrosive (F= 0.546) while the MXD-Lotion (F= -0.345) 224
exhibited a corrosive potential. 225
4. Discussion 226 The aim of the present work was to develop a suitable MXD formulation for the treatment of 227
hair loss and therefore it was necessary to achieve sufficient drug permeation and viscosity using 228 new polymers in order to obtain an adequate concentration for desired drug. In the present 229 investigation, the self-gelling properties of acrylamide/sodium acryloyldimethyltaurate copolymer 230 (Sepineo P 600) was used at three different concentrations to achieve desired rheological behavior of 231 the formed gel. Low concentration of polymer will lead to simple solution, while high concentration 232 may lead to formation of gel with high viscosity leading to non-uniform distribution of drug and 233 problems like handling and spreading [22]. 2% w/v gelling agent concentration was found to be 234 suitable for desirable viscosity. Also, greater penetration achieved for the drug may be due to 235 improved hydration of the skin as evidenced by higher occlusivity of MXD-Gel as compared to 236 MXD-Lotion [23]. Moreover, the efficacy of the topical semisolid formulation depends on even 237 spreading of the formulation on the skin. MXD-Gel had approximately similar spreadability as B-gel 238 which indicates that presence of the drug does not affect the spreadability. The adhesiveness of the 239 MXD-Lotion was less than the MXD-Gel due to the presence of gelling agent responsible for 240 adhesiveness [24]. For in vitro release study of MXD, two sets of formulations: one made from 241 Sepieno P 600 and other made from solvent system (Ethanol: Propylene glycol: water) was prepared. 242 From in vitro release study, it is can be concluded that MXD-Gel exhibits slower release in 243 comparison to the MXD-Lotion which is attributed to the presence of gelling agent influencing drug 244
BA
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 25 September 2017 doi:10.20944/preprints201709.0123.v1

8 of 10
diffusion from the gel [25]. Release kinetics study for the prepared gel suggest that Higuchi model is 245 best fit in comparison to other models due to highest regression coefficient (R2= 0.994). Higuchi 246 model describes the drug release form the matrix system, where drug release is a diffusion process 247 based on Fick,s law[26]. The cumulative percent of the drug permeated through pig ear skin showed 248 significant difference for MXD-Lotion and MXD-Gel. The presence of ethanol and propylene glycol 249 in MXD-lotion leads to higher permeation as they are established permeation enhancers; high 250 alcohol content may disrupt SC lipid barrier facilitating drug permeation [27]. Also, viscosity of the 251 prepared gel was unaffected by the presence of the drug as indicated by superimposed up and down 252 flow curve of both B-Gel and MXD-Gel. No significant changes were observed in the pH, drug 253 content and viscosity of the MXD-Gel when subjected to accelerated and real time stability studies. 254 The ideal topical formulation should not produce dermal corrosion which is the production of 255 irreversible damage of the skin. Formulations having pH extremes like less than 2 and more than 256 11.5 may produce dermal effects [28]. Repeated application of such types of formulation results in 257 typical adverse effects. Therefore, it is important to investigate the corrosive factor of formulations 258 available for topical application. The MXD-Gel was found to be non-corrosive as compared to the 259 MXD-Lotion representing an ideal formulation for topical application. 260
5. Conclusion 261 MXD was successfully formulated as gel using Sepineo P 600 as a novel gelling agent. MXD-Gel 262
showed acceptable pH, drug content, viscosity, spreadability and stability along with non 263 corrosivity to skin. Therefore, the present gel formulation could be very promising alternative for 264 lotions available commercially. 265
266 Acknowledgments: The authors would like to thank Zee laboratories Ltd., Baddi (India) for providing the gift 267 sample of Minoxidil and Seppic (India) for the gift sample of Sepineo P 600. 268 Author Contributions: Pawan kumar planned and performed the experiment under the supervision of 269 Shailendra kumar singh. The manuscript was written by Pawan Kumar and Deepak Jindal. Vandana Handa 270 edited the manuscripts writing and English. All authors participated in discussion and correction of 271 manuscript. 272 Conflicts of Interest:The authors declare no conflicts of interest. 273
6. References 274
1. Mirzoyev, S.A.; Schrum, A.G.; Davis, M.D.P.; Torgerson, R.R. Lifetime incidence risk of alopecia areata 275 estimated at 2.1% by rochester epidemiology project, 1990-2009. J Invest Dermatol 2014, 134, 1141-1142, 276 doi: 10.1038/jid.2013.464. 277
2. McElwee, K.J.; Gilhar, A.; Tobin, D.J.; Ramot, Y.; Sundberg, J.P.; Nakamura, M.; Bertolini, M.; Inui, S.; 278 Tokura, Y.; King, L.E., Jr., et al. What causes alopecia areata? Exp Dermatol 2013, 22, 609-626, doi: 279 10.1111/exd.12209. 280
3. Messenger, A.G.; Rundegren, J. Minoxidil: Mechanisms of action on hair growth. Br J Dermatol 2004, 281 150, 186-194, doi: 10.1111/j.1365-2133.2004.05785.x. 282
4. Wagner, L.; Kenreigh, C. Minoxidil. In Xpharm: The comprehensive pharmacology reference, Elsevier: New 283 York, 2007; pp 1-5. 284
5. Reddy, M.S.; Mutalik, S.; Rao, G.V. Preparation and evaluation of minoxidil gels for topical application 285 in alopecia. Indian journal of pharmaceutical sciences 2006, 68, doi: 10.4103/0250-474X.27813. 286
6. Mura, S.; Manconi, M.; Sinico, C.; Valenti, D.; Fadda, A.M. Penetration enhancer-containing vesicles 287 (pevs) as carriers for cutaneous delivery of minoxidil. International journal of pharmaceutics 2009, 380, 288 72-79, doi: 10.1016/j.ijpharm.2009.06.040. 289
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 25 September 2017 doi:10.20944/preprints201709.0123.v1

9 of 10
7. Lopedota, A.; Cutrignelli, A.; Denora, N.; Laquintana, V.; Lopalco, A.; Selva, S.; Ragni, L.; Tongiani, S.; 290 Franco, M. New ethanol and propylene glycol free gel formulations containing a 291 minoxidil-methyl-β-cyclodextrin complex as promising tools for alopecia treatment. Drug development 292 and industrial pharmacy 2015, 41, 728-736, doi: 10.3109/03639045.2014.900078. 293
8. Khullar, R.; Kumar, D.; Seth, N.; Saini, S. Formulation and evaluation of mefenamic acid emulgel for 294 topical delivery. Saudi Pharm J 2012, 20, 63-67, doi: 10.1016/j.jsps.2011.08.001. 295
9. Bonacucina, G.; Cespi, M.; Palmieri, G.F. Characterization and stability of emulsion gels based on 296 acrylamide/sodium acryloyldimethyl taurate copolymer. AAPS PharmSciTech 2009, 10, 368-375, doi: 297 10.1208/s12249-009-9218-1. 298
10. Joshi, M.; Patravale, V. Formulation and evaluation of nanostructured lipid carrier (nlc)-based gel of 299 valdecoxib. Drug Dev Ind Pharm 2006, 32, 911-918, doi: 10.1080/03639040600814676. 300
11. Khurana, S.; Jain, N.K.; Bedi, P.M. Development and characterization of a novel controlled release 301 drug delivery system based on nanostructured lipid carriers gel for meloxicam. Life Sci 2013, 93, 302 763-772, doi: 10.1016/j.lfs.2013.09.027. 303
12. Khurana, S.; Jain, N.K.; Bedi, P.M. Nanoemulsion based gel for transdermal delivery of meloxicam: 304 Physico-chemical, mechanistic investigation. Life Sci 2013, 92, 383-392, doi: 10.1016/j.lfs.2013.01.005. 305
13. Patel, V.M.; Prajapati, B.G.; Patel, H.V.; Patel, K.M. Mucoadhesive bilayer tablets of propranolol 306 hydrochloride. AAPS PharmSciTech 2007, 8, E77, doi: 10.1208/pt0803077. 307
14. Yong, C.S.; Sah, H.; Jahng, Y.; Chang, H.W.; Son, J.-K.; Lee, S.H.; Jeong, T.C.; Rhee, J.-D.; Baek, S.H.; 308 Kim, C.-K. Physicochemical characterization of diclofenac sodium-loaded poloxamer gel as a rectal 309 delivery system with fast absorption. Drug development and industrial pharmacy 2003, 29, 545-553, doi: 310 10.1081/DDC-120018643. 311
15. Uprit, S.; Kumar Sahu, R.; Roy, A.; Pare, A. Preparation and characterization of minoxidil loaded 312 nanostructured lipid carrier gel for effective treatment of alopecia. Saudi Pharm J 2013, 21, 379-385, doi: 313 10.1016/j.jsps.2012.11.005. 314
16. Kathuria, H.; Li, H.; Pan, J.; Lim, S.H.; Kochhar, J.S.; Wu, C.; Kang, L. Large size microneedle patch to 315 deliver lidocaine through skin. Pharm Res 2016, 33, 2653-2667, doi: 10.1007/s11095-016-1991-4. 316
17. Kumar, P.; Singh, S.K.; Mishra, D.N.; Girotra, P. Enhancement of ketorolac tromethamine permeability 317 through rat skin using penetration enhancers: An ex-vivo study. International journal of pharmaceutical 318 investigation 2015, 5, 142, doi: 10.4103/2230-973X.160850. 319
18. Shams, M.S.; Alam, M.I.; Ali, A.; Sultana, Y.; Aqil, M. Pharmacodynamics of a losartan transdermal 320 system for the treatment of hypertension. Drug Dev Ind Pharm 2010, 36, 385-392, doi: 321 10.3109/03639040903188471. 322
19. Rompicharla, S.V.K.; Bhatt, H.; Shah, A.; Komanduri, N.; Vijayasarathy, D.; Ghosh, B.; Biswas, S. 323 Formulation optimization, characterization, and evaluation of in vitro cytotoxic potential of curcumin 324 loaded solid lipid nanoparticles for improved anticancer activity. Chem Phys Lipids 2017, 208, 10-18, 325 doi: 10.1016/j.chemphyslip.2017.08.009. 326
20. Padois, K.; Cantieni, C.; Bertholle, V.; Bardel, C.; Pirot, F.; Falson, F. Solid lipid nanoparticles 327 suspension versus commercial solutions for dermal delivery of minoxidil. Int J Pharm 2011, 416, 328 300-304, doi: 10.1016/j.ijpharm.2011.06.014. 329
21. Shinde, U.; Pokharkar, S.; Modani, S. Design and evaluation of microemulsion gel system of 330 nadifloxacin. Indian J Pharm Sci 2012, 74, 237-247, doi: 10.4103/0250-474X.106066. 331
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 25 September 2017 doi:10.20944/preprints201709.0123.v1

10 of 10
22. Khan, A.W.; Kotta, S.; Ansari, S.H.; Sharma, R.K.; Kumar, A.; Ali, J. Formulation development, 332 optimization and evaluation of aloe vera gel for wound healing. Pharmacogn Mag 2013, 9, S6-S10, doi: 333 10.4103/0973-1296.117849. 334
23. Muller, R.H.; Radtke, M.; Wissing, S.A. Solid lipid nanoparticles (sln) and nanostructured lipid carriers 335 (nlc) in cosmetic and dermatological preparations. Adv Drug Deliv Rev 2002, 54 Suppl 1, S131-155, doi: 336 10.1016/S0169-409X(02)00118-7. 337
24. Barakat, N.S. Evaluation of glycofurol-based gel as a new vehicle for topical application of naproxen. 338 Aaps Pharmscitech 2010, 11, 1138-1146, doi: 10.1208/s12249-010-9485-x. 339
25. PATEL, B.; BANWAIT, H.; PARMAR, K.; PATEL, M. Formulation and evaluation of topical 340 aceclofenac gel using different gelling agent. International Journal of drug development and research 2011, 341 doi. 342
26. Higuchi, T. Mechanism of sustained-action medication. Theoretical analysis of rate of release of solid 343 drugs dispersed in solid matrices. J Pharm Sci 1963, 52, 1145-1149, doi: 10.1002/jps.2600521210. 344
27. Trottet, L.; Merly, C.; Mirza, M.; Hadgraft, J.; Davis, A.F. Effect of finite doses of propylene glycol on 345 enhancement of in vitro percutaneous permeation of loperamide hydrochloride. Int J Pharm 2004, 274, 346 213-219, doi: 10.1016/j.ijpharm.2004.01.013. 347
28. Scheel, J.; Heppenheimer, A.; Lehringer, E.; Kreutz, J.; Poth, A.; Ammann, H.; Reisinger, K.; Banduhn, 348 N. Classification and labeling of industrial products with extreme ph by making use of in vitro 349 methods for the assessment of skin and eye irritation and corrosion in a weight of evidence approach. 350 Toxicology in Vitro 2011, 25, 1435-1447, doi: 10.1016/j.tiv.2011.04.017. 351
352
353
354
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 25 September 2017 doi:10.20944/preprints201709.0123.v1
Related Documents


![Symmetric alopecia in the dog [Read-Only]alaskanmalamute.org/.../uploads/2015/11/Symmetric-alopecia-in-the … · of alopecia in the dog Pathogenesis Clinical appearance of alopecia](https://static.cupdf.com/doc/110x72/5ebdda54a09b4c70d34c1b77/symmetric-alopecia-in-the-dog-read-only-of-alopecia-in-the-dog-pathogenesis.jpg)