1. Introduction 2. ‘Injectable’ platforms 3. Patch-based platforms 4. Future platform technologies 5. Expert opinion Review Engineering cell platforms for myocardial regeneration Udi Sarig & Marcelle Machluf † Technion--Israel Institute of Technology, The Laboratory of Cancer, Drug Delivery & Mammalian Cell Technology, Faculty of Biotechnology & Food Engineering, Haifa, Israel Introduction: Various engineered ‘cell-platforms’ have been reported in recent years for the possible treatment of myocardial infarction (MI) and end-stage heart failure. These engineered platforms rely on two key factors: cells and/or biomaterial scaffolds for the regeneration of the infarcted heart tissue. Areas covered: Two major cell-platform approaches are described and broadly categorized as ‘injectable cell platforms’ and ‘patch-based cell platforms’. The recent advancements in these cell-platforms in terms of their relative successes in-vivo as well as their clinical feasibility are summarized. Natural as well as synthetic scaffolds, with or without the cellular compo- nent, are compared with cell based therapy alone. This review focuses on achievements, as well as the gaps that are presently checking any progress towards producing clinically relevant panacea for myocardial regeneration. Expert opinion: Cardiac and induced pluripotent stem cells will probably be the focus of future research. The combined cell-biomaterial scaffold therapy is superior to cell therapy alone. Nevertheless, encouraging pre-clinical successes have limited translation into clinical practice due to limited cell survival post transplantation, inadequate construct thicknesses for human- sized hearts and the traditional use of ‘flat (2D) tissue culture’ techniques. The development of complementary dynamic 3D cultivation platforms will probably lead to improved outcomes and enable fast screening of various therapeutic approaches. Keywords: cardiomyocyte cell sources, cell therapy, extracellular matrix (ECM), injection- and patch-based cell platforms, myocardial infarction, myocardial tissue engineering, scaffolds Expert Opin. Biol. Ther. (2011) 11(8):1055-1077 1. Introduction In myocardial infarction (MI) the blood supply to the cardiac muscle (myocardium) is halted, leading to profound cell necrosis, downstream of the blocked artery. As cardiomyocytes (CM, the actively contracting heart cells) have a limited regenera- tion capacity, rapid inflammatory response takes over, leading to the formation of a fibrotic scar tissue that is unable to actively contract and imposes an extra burden on the remaining healthy myocardium. In the USA alone, approximately 1 million individuals suffer from acute MI annually, making it the leading cause of heart fail- ure [1]. Current pharmacological therapies and surgical interventions can slow the progression to end-stage disease, but they rarely prevent or reverse the progression of the failing state [2]. At present, the only therapeutic options available to treat patients with terminal end-stage heart failure are heart transplantations or ventricu- lar assist devices (VADs). These options have significant cost and availability limita- tions, leading to vast research in emerging fields such as cell therapy and tissue engineering [3]. Such research has resulted in the development of various engineered 10.1517/14712598.2011.578574 © 2011 Informa UK, Ltd. ISSN 1471-2598 1055 All rights reserved: reproduction in whole or in part not permitted Expert Opin. Biol. Ther. Downloaded from informahealthcare.com by Hebrew University on 11/28/11 For personal use only.

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

1. Introduction
2. ‘Injectable’ platforms
3. Patch-based platforms
4. Future platform technologies
5. Expert opinion
Review
Engineering cell platforms formyocardial regenerationUdi Sarig & Marcelle Machluf†
Technion--Israel Institute of Technology, The Laboratory of Cancer, Drug Delivery & Mammalian
Cell Technology, Faculty of Biotechnology & Food Engineering, Haifa, Israel
Introduction: Various engineered ‘cell-platforms’ have been reported in
recent years for the possible treatment of myocardial infarction (MI) and
end-stage heart failure. These engineered platforms rely on two key factors:
cells and/or biomaterial scaffolds for the regeneration of the infarcted
heart tissue.
Areas covered: Two major cell-platform approaches are described and
broadly categorized as ‘injectable cell platforms’ and ‘patch-based cell
platforms’. The recent advancements in these cell-platforms in terms of their
relative successes in-vivo as well as their clinical feasibility are summarized.
Natural as well as synthetic scaffolds, with or without the cellular compo-
nent, are compared with cell based therapy alone. This review focuses on
achievements, as well as the gaps that are presently checking any progress
towards producing clinically relevant panacea for myocardial regeneration.
Expert opinion: Cardiac and induced pluripotent stem cells will probably be
the focus of future research. The combined cell-biomaterial scaffold therapy
is superior to cell therapy alone. Nevertheless, encouraging pre-clinical
successes have limited translation into clinical practice due to limited cell
survival post transplantation, inadequate construct thicknesses for human-
sized hearts and the traditional use of ‘flat (2D) tissue culture’ techniques.
The development of complementary dynamic 3D cultivation platforms will
probably lead to improved outcomes and enable fast screening of various
therapeutic approaches.
Keywords: cardiomyocyte cell sources, cell therapy, extracellular matrix (ECM),
injection- and patch-based cell platforms, myocardial infarction,
myocardial tissue engineering, scaffolds
Expert Opin. Biol. Ther. (2011) 11(8):1055-1077
1. Introduction
In myocardial infarction (MI) the blood supply to the cardiac muscle (myocardium)is halted, leading to profound cell necrosis, downstream of the blocked artery. Ascardiomyocytes (CM, the actively contracting heart cells) have a limited regenera-tion capacity, rapid inflammatory response takes over, leading to the formation ofa fibrotic scar tissue that is unable to actively contract and imposes an extra burdenon the remaining healthy myocardium. In the USA alone, approximately 1 millionindividuals suffer from acute MI annually, making it the leading cause of heart fail-ure [1]. Current pharmacological therapies and surgical interventions can slow theprogression to end-stage disease, but they rarely prevent or reverse the progressionof the failing state [2]. At present, the only therapeutic options available to treatpatients with terminal end-stage heart failure are heart transplantations or ventricu-lar assist devices (VADs). These options have significant cost and availability limita-tions, leading to vast research in emerging fields such as cell therapy and tissueengineering [3]. Such research has resulted in the development of various engineered
10.1517/14712598.2011.578574 © 2011 Informa UK, Ltd. ISSN 1471-2598 1055All rights reserved: reproduction in whole or in part not permitted
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

‘cell-platforms’ that rely on two key factors: cells and/or bio-material scaffolds for the regeneration of the infarctedheart tissue.The cellular component, the more complex part of the
engineered cell-platform, has to contract, remodel and ulti-mately regenerate the defective myocardium. The ideal cellsource should be easy to obtain and cultivate in great num-bers as the native cardiac tissue is densely populated (~ 5 �108 cells/cm3) [4]. Furthermore, the cell source and/or its dif-ferentiated products should be biocompatible, to avoid rejec-tion post transplantation. Last but not least, cell safety is amatter of concern, particularly when referring to geneticallymodified cells.The heart muscle (i.e., myocardium) consists of at least
three basic cell types (i.e., 20 -- 40% CMs; 60 -- 80% car-diac fibroblasts and endothelial cells) [4]. Thus any appliedtissue engineering technique should be able to combinethese three cell populations resulting in CM that are elec-tromechanically coupled to the host tissue while having aproper vascular supply and connective tissue to ensurefunctionality [5]. However, as only CM contribute to func-tional contraction, and these cannot be expanded ex-vivo,several other CM cell sources have been suggested for thereplacement and regeneration of the infarcted heart,including embryonic stem cells (ESCs) [6-12], induced plu-ripotent stem cells (iPSCs) [11-18], mesenchymal stem cells(MSCs) [19-27], and cardiac stem cells (CSCs) [28-32]. Eachof these cell sources has its own pros and cons, as discussedin recent reviews [1,3,33].Nonetheless, cellular therapy by itself is still limited and does
not yet lead to sufficient cardiac tissue regeneration [3], demon-strating the need for other supporting, yet crucial factors, suchas the biomaterial scaffold. Biomaterial scaffolds serve to mimicthe natural extracellular matrix (ECM) and aim to provide thephysical and biological support to the grafted cells duringin-vitro/ ex-vivo cultivation, as well as to the host cardiac tissuepost transplantation. Ideally, these scaffolds should degradeto biocompatible byproducts in parallel to the secretion of
a substituting ECM by the host tissue and the grafted cells.Further incorporation of growth and pro-survival factors withinthese scaffolds may enhance tissue regeneration by affectingboth host and transplanted cells. However, the applicationand effect of such growth factors will be discussed briefly, asit is outside the scope of this review.
Despite the importance of these two key elements (i.e., cellsand biomaterial scaffolds), they cannot solely account for theperformance of engineered myocardial cell platforms withoutmechanical stimuli in the form of the cardiac rhythm andelectrical cues, which mimic the natural cardiac environment.This area of dynamic cultivation technologies is an emergingone that plays a fundamental role at the level of cell -- celland cell -- scaffold interactions. It is also thoroughly reviewedelsewhere [34,35].
In this article, recent cell platforms that have been engi-neered for myocardial regeneration are addressed (Figure 1).We discuss, in detail, their relative successes in-vivo and theirclinical feasibility. Furthermore, the most promising emergingtechnologies, particularly those that might contribute toimproved outcomes in-vivo are also described.
2. ‘Injectable’ platforms
Injection of cells alone, biomaterial alone or combinationsthereof, is a clinically preferred delivery technique, as it is con-sidered to be minimally invasive and a controlled procedure.The injection can be performed either directly into the infarctarea or, when cell size permits, through the coronary circula-tion [36]. Injected platforms can take the form of any infarctwith relatively little effort, delaying subsequent wall thinning.Furthermore, the ability of injected cells and active biomateri-als to attract host stem and progenitor cells into the infarctarea is compelling [37]. Studies have reported the injection ofcells alone or in combination with polymers such as liquidizedECM, collagen, fibrin, alginate, chitosan, hyaluronic acid(HA) hydrogels, and synthetic derivatives of poly(N-isopropy-lacrylamide) (PNIPAAM) and PEG (Tables 1,2,3). Thesetwo forms of injections will be discussed separately in thefollowing sections.
2.1 Injectable cell-therapyIn general, the contribution of cells to cardiac regeneration isbelieved to be mitigated through three independent mecha-nisms of action: angiogenesis, myogenesis and paracrineeffects [3]. The intracoronary injection of cells has shown lim-ited success in terms of their delivery efficiency into the myo-cardium and in terms of transplanted cells’ homing andsurvival, when compared with direct intramyocardial injec-tions [36]. This review focuses on the use of the most reportedand clinically relevant cell sources for CM differentiation:ESCs [10,38-51], iPSC [11-18], MSCs [52-65] and CSC [28-32].Nevertheless, as many studies have reported the utilizationof other cell types (such as skeletal myoblasts, bone marrowmononuclear cells and endothelial progenitor cells), we would
Article highlights.
. Cell platforms for myocardial regeneration can bebroadly categorized as either injection- or patch-basedplatforms.
. Combined cell--biomaterial scaffold platforms showsuperior results compared with cell therapy alone.
. Even though many reports have shown significantimprovement in pre-clinical studies, the translation intoclinical practice is still limited.
. We review the latest achievements and drawbacks ofthese strategies and mark the technological hurdlesblocking the achievement of clinically relevant solutions.
. Evolving technologies that may enable improvedpre-clinical outcomes are discussed.
This box summarizes key points contained in the article.
Engineering cell platforms for myocardial regeneration
1056 Expert Opin. Biol. Ther. (2011) 11(8)
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

like to direct the reader to recent in depth reviews discussingthe cellular aspects of myocardial regeneration [3,66-68].
2.1.1 Embryonic stem cellsESCs have the ability to self renew and also to differentiatein a robust biochemical procedure into beating and contract-ing CM-like cells, having similar (although not identical)characteristics to that of the adult CM [6,7,11,41,69]. InjectedESC-derived CM have been shown to integrate with hostmyocardium and improve the electrical conduction ininfarcted mouse and rat hearts [38,41,44,50]. Similar resultswere obtained using human-ESC-derived CM in a porcinemodel [39] and early cardiac progenitors (stage-specificembyonic antigen (SSEA)+) of primate ESCs transplanted inan infarcted primate model [12].
Nonetheless these cells are considered immunogenic [67]
and are known to form teratomas post transplantationin-vivo [9,42,43,70]. Immunogenic rejection could be overcomewith the use of autologous induced pluripotent cells (iPSCs,further discussed hereafter) and the occurrence of teratomaformation is reduced by the selection of phenotypically dif-ferentiated CM produced from ESCs [9,42,51]. Further majordifficulties include collecting unadulterated hESC-derivedCM (hESC-CM) in large quantities and assuring their longterm survival. These represent major obstacles for cell-basedtherapy [10,44].
To increase hESC-CM yield, Laflamme et al., have utilizedactivin- A and bone morphogenetic protein 4 (BMP4). Theyfurther incorporated a pro survival factors’ cocktail (PSC) tolimit hESC-CM death post transplantation into a rat acute MImodel [41]. The engrafted human myocardium attenuated ven-tricular dilation and preserved regional and global contractilefunction compared with controls receiving non-cardiac hESCderivatives or vehicle. However, the significance of these resultshas been challenged by van Laake et al. who evaluated thelong-term (12 weeks) fate of hESC-CM transplanted in immu-nocompromised acute MI mice model. Their results exhibitedrapid formation of grafts with organized CM that havingmatured over time, were further accompanied with significantimprovement in cardiac function at 4 weeks post transplanta-tion, yet this was not sustained at 12 weeks [44]. From theseresults, it was argued that there is a requirement for a minimum3 month follow-up in studies that claim to observe improvedcardiac function. We further infer that this requirement is inde-pendent of whether hESC or other (adult) cell types are used fortransplantation. In a more recent study by the former group,Intramyocardial injection of hESC-CM with the same PSCinto chronic rat MI models was evaluated. Histology performedat the 3 month time point revealed that human CM survived,developed increased sarcomere organization andwere still prolif-erating. Despite successful engraftment, both echocardiographyand MRI analyses showed no significant difference in left
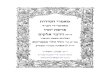
Injectable platforms Patch-based platforms
C.
B.
A. D.
E.
F.
Figure 1. Schematic representation of the major strategies for myocardial tissue engineering. These strategies rely on
cardiogenic cell sources, which are administered either alone or in combination with various natural or synthetic scaffolds.
Injectable platforms (A. -- C.) could be delivered through the vena cava (intravenous, A.), through the coronary arteries
(intracoronary, B.) or into the infarcted zone or its border (intramyocardial, C.). Patch based platforms (D. -- F.) include
scaffold-free or cell-sheet transplantation (D.), tissue engineered constructs made out of various cell--biomaterial scaffold
combinations (E.) or patches made out of biomaterial scaffolds alone (F.).
Sarig & Machluf
Expert Opin. Biol. Ther. (2011) 11(8) 1057
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

Table
1.Cardiomyocyte
cellso
urces.
Cell
type
Cell
source
Advantages
Disadvantages
Pre-clinical
studies
Clinical
trials
ESCs
Embryo
BiochemicaldifferentiationtowardsCM
likebeating
cells
iswellcharacterized
Giverise
tootherregenerative
celltypes(i.e.,
endothelialcells
andfibroblasts)
Integrateswithhost
tissueandim
prove
conductivity
andfunction
Requireschronicim
munosuppression
Capable
ofteratomaform
ation
(particularlyifnotfully
differentiated)
Relatively
low
yield
ofCM
Ethicalissues
Murine[38,40-46,49,51,
136] ;Porcine[39]
Nonereported
iPSCs
Derm
alfibroblasts
Autologouscellsource(noim
munosuppression
required)
Knownbiochemicaldifferentiationtowards
CM-likebeatingcells
Integrate
withhost
tissueandim
prove
conductivity
andfunction
Requiresgeneticmanipulation
Relatively
low
yield
ofCM
Murine[16];Primate
[12]
Nonereported
MSCs
Bonemarrow
Umbilicalvein
Adipose
tissue
Dentalpulp
Autologouscellsource(noim
munosuppression
required)
Relatively
easy
toisolate
andculture
inlarge
quantities
Improve
cardiacfunction
Giverise
tootherregenerative
celltypes(i.e.,
endothelialcells
andvascularmuscle)
Nolong-term
effect/survivability
(>6months)
Little
integrationwithhost
tissue
Positive
effectsare
basedonparacrine
effectsandangiogenesisinductionrather
thanCM
differentiation
Norobust
andsafe
CM
differentiation
procedure
reportedto
date
Murine[21,56,59,60,133,
139,157,158,166,167,175,178,
190-191] ;Porcine[61-63]
Phase
I[72]
CSCs
Heart
Autologouscellsource(noim
munosuppression
required)
Relatively
easy
toisolate
andculture
inlarge
quantities
Improve
cardiacfunction
Secrete
acocktailofgrowth
andprosurvival
factors
thatprobably
best
fitmyocardial
regeneration
Giverise
tootherregenerative
celltypes
(i.e.,epithelialcells
andvascular
muscle)
Norobust
CM
differentiationprocedure
inlarge-anim
almodelsreportedto
date
Murine[29,31-32]
Phase
I[80]
CM:Cardiomyocytes;
CSCs:
Cardiacstem
cells;ESCs:
Embryonic
stem
cells;iPSCs:
Inducedpluripotentstem
cells;MSCs:
Mesenchym
alstem
cells.
Engineering cell platforms for myocardial regeneration
1058 Expert Opin. Biol. Ther. (2011) 11(8)
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

Table
2.Naturalbiomaterials
formyocardialcellplatform
s.
Polymer
Advantages
Disadvantages
Pre-clinicalstudies
Clinicaltrials
ECM
Closest
mim
icto
naturalcellsurroundings
Bioactive,biodegradable
andbiocompatible
Improvesmyocardialgeometryandfunction
Promotesvasculature
form
ation
Inducible
gellingmechanism
insitu
Highbatchto
batchvariability
More
problematicin
term
sofmass
production
Inconvenientisolationprocedures
Murine[41,83,84,86,87,150,157,158,
168,175] ;Canine[146,148];Porcine
[147,152]
Nonereported
Collagen/
Gelatin
Themajorbuildingblock
ofnaturalECM
Bioactive,biodegradable
andbiocompatible
Improvesmyocardialgeometryandfunction
Enhancedcellretention/survivalupontransplantation
Commercially
available
Inducible
gellingmechanism
insitu
Adverseeffectsonangiogenesisand
vasculature
form
ation
Murine[40,89-94,131,165-168,170,175,
176,178,180] ;Porcine[95]
Phase
I[179]
Fibrin
Biologicalglueandcelladhesive
withcontrolled
polymerizationanddegradationkinetics
Bioactive,biodegradable
andbiocompatible
Leadsto
improvedmyocardialgeometryandfunction
uponinjection
Nosignificantlongterm
effects
observedin
humanpatients
Murine[99,100];Chick[101];Sheep
[98]
Phase
II[102]
Alginate
Biodegradable
andbiocompatible
Inducible
gellingmechanism
insitu
Commercially
available
atrelatively
low
cost
FDA
approved
Improvesmyocardialgeometry
andfunctionuponinjection
Low
mechanicalpropertiesmatchwith
themyocardium
Nosignificantim
provementin
vasculature
form
ationuponinjection
Adversebioactivity
Murine[104-106,172-174];Porcine[107]
On-going
Phase
II[109]
Chitosan
Biodegradable
andbiocompatible
Commercially
available
atrelatively
low
cost
Variable
form
ulationsallow
forcontrolledandversatile
end-product
mechanicalproperties
Inducible
gellingmechanismsin
situ
Improvesmyocardialgeometryandfunction
uponinjection
Promotesvasculature
form
ation
Mechanism
ofvasculature
support
are
poorly
understood
Absence
ofdata
onchitosanbioactivityand
contributionin
large-anim
almodels
Murine[46,113]
Nonereported
HA
Improvesmyocardialgeometryandfunctionupon
injection
Bioactive,biodegradable
andnon-immunogenic
Commercially
available
Absentdata
onbioactivityin
largeanim
al
models
Low
mechanicalpropertiesmatchwith
themyocardium
Relatively
expensive
Murine[116]
Nonereported
ECM:Extracellularmatrix;HA:Hyaluronic
acid.
Sarig & Machluf
Expert Opin. Biol. Ther. (2011) 11(8) 1059
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

Table
3.Syntheticbiomaterials
formyocardialcellplatform
s.
Polymer
Advantages
Disadvantages
Pre-clinicalstudies
Clinicaltrials
PNIPAAM
(andderivatives)
Inducible
gellingmechanism
insitu
Promotesvasculature
form
ation
Celladherence
istemperature-dependent
Mechanicalpropertiescould
matchthose
of
thenative
myocardium
Controlledandrobust
manufacturingprocesses
Commercially
available
atrelatively
low
cost
Lacksbiodegradability
(derivative-dependent)
Poorphysiologicalclearance
(derivative-dependent)
Lack
ofdata
inlargeanim
almodels
Murine[126];Rabbit
[121,125]
Nonereported
PEG
(andderivatives)
Improvesmyocardialgeometryandfunction
uponinjection(derivative
dependent)
Bio-inert
Lacksbiodegradability
(derivative-dependent)
Poorphysiologicclearance
(derivative-dependent)
Lack
ofdata
onPEG
andderivativescontributionin
largeanim
almodels
Nosignificantim
provementin
vasculature
form
ation
uponinjection
Murine[128,129];
Rabbit
[130]
Nonereported
Polyesters
(e.g.,poly-a-
Hydroxy-acid;PLA
;PGA;
PCL;
PLG
A;PCLA
;PLC
L)
Biodegradable
andbiocompatible
Co-polymers
could
allow
foramore
controlled
degradationkinetics
Controlledandrobust
manufacturingprocesses
Commercially
available
Improvesmyocardialgeometryandfunction
Mightcause
localhighacidconcentrationsleading
toaninflammatory
response
Suddenloss
offunctionalintegrity
dueto
bulk
degradationkinetics
Usedprimarily
forpatch-basedplatform
sLow
mechanicalpropertiesmatchwiththemyocardium
Lack
ofdata
onpolyesters
contributionin
large-anim
al
models
Murine[45,138,
139,175,176,178]
Nonereported
Elastomers
(PU;poly(TMC)
andco-polymers
withPLA
/PCL;
PGS
Biodegradable
Biocompatible
(derivative-dependent)
Mechanicalpropertiescould
bemadeto
match
those
ofthemyocardium
Short-term
improvementin
myocardialgeometry
andfunction
Localinflammationcausedbydegradationbyproducts
(derivative-dependent)
Usedprimarily
forpatch-basedplatform
sLack
ofdata
onelastomers
contributionin
largeanim
al
models
Murine[49,141,
142,175]
Nonereported
NIPAAM:Poly(N-isopropylacrylamide);PCL:
Poly(e-caprolactone);PCLA
:Caprolactone-co-L-lactidespongereinforcedwithknittedpoly-L-lactidefabric;
PGA:Poly(glycolic
acid);PGS:Poly(glycerol-sebacate);PLA
:Poly(lactic
acid);PLC
L:Poly(lactide-co-e-caprolactone);PLG
A:Poly
(lactic
co-glycolic
acid);poly(TMC):Poly(1,3
trim
ethylenecarbonate);PU:Polyurethane.
Engineering cell platforms for myocardial regeneration
1060 Expert Opin. Biol. Ther. (2011) 11(8)
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

ventricular structure or function compared with controls. Thissuggested that cell transplantation should be conducted in theacute or sub-acute phases of MI and is probably not effectiveonce the fibrotic scar tissue is already formed at the chronicphase of MI [71]. This finding contradicts previous resultsreported by Caspi et al., who injected hESC-CM into a similarchronic infarction rat model, revealing attenuation of left ven-tricular dilatation and improved cardiac function one monthpost tranplantation [9].
Although more preclinical studies are needed beforesuch therapies can be implemented clinically, a recent FDAapproval for ESC-based clinical trials in human patientsfor the treatment of spinal injuries [72] is a positive signthat ESC technology may one day be applied to clinicalcardiac regeneration.
2.1.2 Induced pluripotent stem cellsIn the last few years efforts have been invested in reprogram-ming autologous dermal fibroblasts, both murine and human,into a pluripotent state to avoid immunogenic rejection. Thephenotype of isolated iPSCs is very similar to that of ESCsand thus CM isolation from an autologous source is possible,as demonstrated by several groups [13,16-18]. In addition, theability to create iPSCs, without the use of genome-integratedviral vectors and oncogenes, has been demonstrated recentlyand supports the notion of future clinical use [14,15,73].Nelson et al., have recently reported the intramyocardial deliv-ery of iPSCs into immune-competent adult MI mice model,yielding progeny that properly engrafted without disruptingcytoarchitecture. In contrast to parental non-reparative fibro-blasts, iPSCs treatment restored post-ischemic contractile per-formance, ventricular wall thickness and electrical stabilitywhile achieving in situ regeneration of cardiac, smooth muscleand endothelial tissue [16]. However, as the isolation techniquefor iPSC-derived CM, still relies on the micromanipulation ofbeating areas within the embryonic body [10], the ability to pro-duce the needed amount of CM-like cells still limits its applica-tion for clinical cell-based therapy. Furthermore, the limitedunderstanding of the process of iPSCs senescence, may hindertheir potential use in the elderly [74].
2.1.3 Mesenchymal stem cellsMSCs are multipotent stem cells isolated from several adulttissues including bonemarrow, adipose, umbilical vein and den-tal pulp [53,75]. Their ability to differentiate into CM like cellswas first demonstrated a decade ago by the exposure of murinebone marrow stromal cells to 5-azacytidine [19,20]. Even thoughthese results have not yet been reproduced with humanMSCs [57,58] and are probably dependent on the MSC tissue oforigin and on yet unknown signaling factors within the myocar-dial milieu [75], they serve as a proof of concept for the applicabil-ity of MSC in cardiac regeneration. In addition, MSCswere demonstrated to express cardiac-specific markers [23],which increase when exposed to neonatal CM-conditionedmedia [26,27,52]. Intracoronary [59,64], intravenous [56,60,64] and
intramyocardial [64,65] injection of MSCs alone, yieldedimproved results compared with controls in mice and rat animalmodels. However, MSCs did not exhibit long term (6 months)survivability [55] and their positive influence is largely due toparacrine effects [24] rather than differentiation into active CMcell populations.
Schuleri et al. reported the autologous intramyocardialinjection of MSCs in a swine chronic MI model. High-dose(200 million cells) MSC therapy reduced infarct size andincreased regional contractility in both infarct and borderzones [63]. They also reported that engrafted MSCs can differen-tiate into three lineages: CM, endothelial and vascular mus-cle [62]. Poncelet et al., have shown that allogeneic porcinemesenchymal stem cell transplantation enhanced angiogenesisafter myocardial infarction, yet this effect was limited to the via-ble myocardium in the borders of the infarct area [61]. Theseencouraging results have led to a recent clinical trial with alloge-neic MSCs administered intravenously to MI patients. Inaddition to significant improvement in cardiac function, noimmunosuppression was required post transplantation and nosafety issues were detected, hence demonstrating the feasibilityof using allogeneic MSC cell sources [54]. Unfortunately, thelack of a reproducible differentiation procedure holds back thedegree of regeneration that could be expected using this cellsource as non differentiated MSC do not actively contract.
2.1.4 Cardiac stem cellsThe traditional view that myocardium lacks regenerativecapacity, has been questioned in the past decade with thediscovery of cardiac progenitor cells [28,76-78] Several groupshave since reported the successful isolation of CSC frommurine [31,78], rat [28], porcine [32] and human hearts [30-32].Oh et al., performed magnetic enrichment of stem cellantigen positive cells (Sca1+) from mice hearts and differenti-ated them in-vitro upon exposure to 5-azcytidine [78].Messina et al., developed a robust technique for the isolationof CSC from cardiac explants of murine and human origin.Using a cardiosphere intermediate step, they isolated cellsthat are capable of self-renewal and give rise to vascular andcontractile cells. While murine cells exhibited spontaneousdifferentiation upon formation of cardiospheres, human cellsexhibited CM differentiation only upon exposure to rat neo-natal CM [31]. Transplantation into infarcted murine heartsled to functional improvement which was also reported in asubsequent collaborative study with the same group usinghuman and porcine CSC [31,32]. In a more recent study, Davisand co-workers further improved the isolation procedure byskipping the cardiosphere step altogether, while exhibitingsimilar results when transplanting the directly explanted crudepopulation into a rat MI model [29]. Despite the fact thatthe efficiency of the cardiosphere methodology has yet to bereproduced sufficiently, with some reports challenging thestemness of these cardiospheres [79], these cells are regardedas holding great promise for future cardiac regeneration andare currently under evaluation in a clinical trial [80].
Sarig & Machluf
Expert Opin. Biol. Ther. (2011) 11(8) 1061
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

2.2 Biomaterial-injection-based platformsTo improve cell attachment, survivability and proliferation,studies have also focused on the incorporation of liquidizedbiomaterials. These biomaterials can be injected to the myo-cardium either alone, with various homing and growth factorsor in combination with various cell sources with the aim ofsupporting the infarcted scar tissue or recruiting endogenousstem and progenitor cells. These attractive biomaterials canbe rapidly polymerized in-situ by various chemical, thermalor optical stimuli [81], thus assuring site-specific delivery in aminimally invasive technique.Different injectable biomaterials have been utilized for
myocardial tissue engineering, which include both syntheticand natural biomaterials. Natural materials feature high bio-activity, biocompatibility and biodegradability. However,there is a high variability associated with their productionand no exact control of their composition and physical char-acteristics, hence standardization and quality control in massproduction becomes overly complex. In contrast, syntheticmaterials have a more robust manufacturing capability, allow-ing for a controlled biochemical composition and characteris-tics. Unfortunately, their bioactivity and biocompatibilityqualities are less than satisfactory in comparison with thenatural scaffolds.
2.2.1 Extracellular matrixThe cardiac ECM consists of a variety of structural proteins (col-lagen, elastin), adhesive proteins (fibronectin, laminin) andother active components (MMP, tissue inhibitors of MMP(TIMP) and plasmin) within a hydrated proteoglycan andglycosaminoglycan-rich milieu [82]. To mimic this complexenvironment, three distinct strategies have been employed: I.Using commercially manufactured ECM (MatrigelTM, BDBiosciences), II. Using acellular ECM and III. Using definedsingle ECM components or mimetics.Matrigel is a secreted ECM mixture that is commercially
manufactured, exploiting mouse tumor cell ECM production.It has been proven effective in the delivery of mouse ESCs tothe left ventricle (LV) either by injection into a pouch madein the left ventricle of rats [83] or by using a direct injectioninto the infarcted myocardium of a mouse model [84]. Boththese studies have resulted in improved heart geometry andfunction with no apparent side effects as compared with eithercells-only or Matrigel-only controls. Similar results were con-firmed by Zhang et al., who mixed Matrigel, collagen and cellculture medium for the delivery of neonatal CM into a rat MImodel [85]. In another study, Laflamme et al., formulated acocktail of pro-survival factors preventing ESC-derived CMdeath. This formula contained Matrigel, which was shownto independently prevent anoikis and increase vasculatureformation after injection into the infarcted myocardium [41].In an attempt to regenerate the infarcted heart using acellular
matrices, Singelyn et al., liquidized acellular cardiac ECM usingpepsin and subsequently injected it into the myocardium viacatheter in a rat MI model [86]. Gelation occurred within the
infarcted scar, leading to a significantly increased infiltrationof endothelial and smooth muscle cells 11 days post injectionalong with an increase in the number of arterioles. The groupalso reported similar results when using pericardial matrix [66].Zhao et al. injected an emulsion made out of acellular sub-intestinal ECM directly into the rat myocardium followingan ischemia--reperfusion event [87]. They reported an improve-ment in functional cardiac parameters (i.e., ejection fraction,fractional shortening and stroke volume) compared with con-trols given injections of saline solution. Taken together, theseresults raise a question as to the difference between variousECM origins, as to that which one has the optimal characteris-tics for promoting myocardial regeneration. As no reporteddata so far has compared these different materials, it is difficultto assess which would be most beneficial for long-term effect.Future experimentation may focus on elucidating this questionas well as on the incorporation of various CM cell sourcestogether with the injected acellular ECM.
2.2.2 CollagenAs the most abundant structural protein in our body’s ECM,collagen has been widely researched for its suitability forinjectable myocardial tissue engineering. So far 28 distinct typesof collagen have been described [88], of which, types I, III and Vare the most abundant in cardiac tissue. Most studies reportedimproved LV geometry and cardiac function when dissolvedcollagen was injected. However, a question arises as to its contri-bution to angiogenesis with some reporting no involvement [89]
whereas others showing improved capillary density and myofi-broblasts infiltration [90]. Researchers also attempted to incorpo-rate cells into injectable collagen or its gelatinous derivatives.According to these studies this approach resulted in improvedcell retention, survival and angiogenesis accompanied by abetter cardiac function compared with either cell-only orcollagen-only controls. Suuronen et al., have shown a significantrestoration of the vascular supply to ischemic tissues uponinjection of a collagen-based matrix with progenitor cells [91].Kutschka et al., further indicated, through bioluminescence,that injection of cardiomyoblasts into pre-transplanted collagenbased GelfoamTM (Pfizer) [92] or together with liquidizedGelfoam [93] enhances their survival in rat hearts comparedwith cell-only injections and non treated controls. Moreoverthe incorporation of reduced Matrigel (with no growth factors)together with the pre-transplanted Gelfoam matrix, showed aneven better improvement than that of cardiomyoblast injectedGelfoam alone. This may be attributed to other ECM compo-nents within the Matrigel that contributed to cell adhesionand survival [92,93]. In another study Zhang et al., usedpositron-emission tomography in addition to histology to assessthe bio-distribution of collagen-seeded progenitor cells. Theirresults showed enhanced cell retention and survival comparedwith cells-only-seeded controls [94].
Takehara et al., used gelatin, a collagen derivative, todeliver basic fibroblast growth factor (bFGF). This growthfactor, with or without gelatin, was injected into a porcine
Engineering cell platforms for myocardial regeneration
1062 Expert Opin. Biol. Ther. (2011) 11(8)
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

MI model alone or in combination with either humancardiosphere-derived cells (CDCs) or MSCs. Their resultssuggested increased microvasculature formation in the gelat-in--bFGF group compared with bFGF directly injected withno gelatin. They also reported a synergistic effect of bFGF--gelatin when combined with human CDCs (but not withMSCs), which included improved cardiac function, LV wallmotion, CM differentiation and infarct scar size [95].
2.2.3 FibrinFibrin, the active truncated form of fibrinogen (cleaved bythrombin), is an important physiological protein that hasbeen widely used in tissue engineering [96,97]. The attractivefeatures of fibrin are its ability to serve as a biological glue,holding cells together in the desired site as well as its abilityto stimulate angiogenesis [96]. Due to these properties, fibrinhas been used both as a delivery vehicle as well as a tissue engi-neering bioactive scaffold [97]. Several groups have shownimprovement in geometry and function of the LV when itwas subjected to fibrin alone or in combinations with variouscells (i.e., endothelial cells, skeletal myoblasts and bone mar-row mononuclear cells) compared with controls that receivedinjections of saline [98-100]. In addition, under physiologicalconditions, fibrin undergoes degradation in parallel to the for-mation of a healthy replacement tissue. This process can becontrolled using inhibitory drugs such as aprotinin [97,101],therefore enabling the adjustment of the degradation kineticswith that of substitute ECM production by the host andseeded cells. Fibrin polymerization kinetics in situ has beencharacterized by Martens et al., proving its suitability forcatheter-based delivery. By maintaining fibrinogen andthrombin concentrations below 5% w/v and under 20 U/mlrespectively, polymerization rates can be controlled to allowadequate time for delivery [81].
Despite these encouraging pre-clinical results in animalmodels, and the vast use of fibrin glues in the clinical setting,little is known on the effects of fibrin on MI in humanpatients. In a clinical trial aimed to reduce reperfusion injurypost MI, Atar et al., have shown that the intravenous bolusinjection of a fibrin derivative (FX06) led to a significantshort term effect on the size of the necrotic center withinthe infarct zone compared with controls receiving placeboinjections [102]. Yet, no significant long-term effect wasobserved apart from that there were fewer patients with seri-ous cardiac events in the treated groups compared with theplacebo group patients.
2.2.4 AlginateThe natural polysaccharide alginate forms compliant hydro-gels upon exposure to divalent ions such as Ca2+ [103]. Thisinduced gelling mechanism, the low cost of high-quantity pro-duction and most importantly the FDA approval for humanuse as a wound dressing material, makes alginate an ideal celldelivery platform for myocardial tissue engineering. Severalrecent studies [104-106], have demonstrated the effectiveness
of alginate injections as it had similar and in some casesbetter effects on the infarct size and function, compared withsaline [105], neonatal CM [104] or fibrin injections [106] inrodents. Alginate has also been reported to cause reverse remod-eling in swine [107]. Its positive effect on the remodeling andfunction of the left ventricle is probably related to its chemicaland physical traits [105]. Ruvinov et al., have developed aninjectable affinity-binding alginate enabling the sequentialdelivery of IGF-1 and hepatocyte growth factor (HGF). Theaffinity-binding alginate protected the proteins from proteolysiswhile maintaining their bioactivity as demonstrated by massspectroscopy and several in-vitro assays respectively. Intramyo-cardial delivery to a rat model of acute MI, preserved scar thick-ness, attenuated infarct expansion and reduced scar fibrosisafter 4 weeks, concomitantly with increased angiogenesis andmature blood vessel formation at the infarct. Apparently thistreatment prevented cell apoptosis, induced cardiomyocytecell cycle re-entry and increased the incidence of GATA-4+
cell clusters implying that this biomaterial has potential toinduce endogenous regeneration of cardiac muscle [108]. Theseimpressive results in animal models, are currently progressingtowards a clinical trial [109].
2.2.5 ChitosanChitosan is another naturally occurring polysaccharide, whichis widely studied as a biocompatible scaffold for skin, bone,cartilage, liver and blood vessel tissue engineering [110]. Chito-san allows the formation of relatively hard porous structures,nanofibrous meshes or compliant hydrogels -- depending onthe choice of chitosan derivative [67]. Chitosan hydrogel isformed either by temperature changes (chitosan -- glycerolphosphate [67]) or optical stimuli (acrylate conjugated [111];or photoinitiator based hdrogels [112]), hence it is capable ofpolymerizing in-situ while entrapping genes, growth factorsand, most attractively for tissue engineering, cells.
Temperature responsive chitosan-glycerol phosphate (GP)hydrogels have been studied for the delivery of ESC and nucleartransferred ESCs to an infarcted rat myocardium, showingimprovement in heart function and wall thickness comparedwith the injection of chitosan-GP or cells only [46,113]. Interest-ingly, both studies showed improvement in the micro-vessel density of the infarcted scar in the chitosan-GP onlyinjected hearts. Though the exact mechanism by which thisangiogenesis process occurs is unknown, it is probably relatedto the ability of chitosan to modulate the proliferation ofvascular cells in-vitro as well as in-vivo [114].
2.3 Other biomaterial-injection based platformsDavis et al., have developed a self-assembling peptide-basedscaffold, which was injected into healthy murine hearts eitheralone or in combination with neonatal CM. In both cases,recruitment of endogenous smooth muscle cells and endothe-lial cells was reported, particularly when CM were added tothe injectable scaffold [115]. Recently, Yoon et al., reportedthe epicardial injection of a hyaluronic acid (HA)-based
Sarig & Machluf
Expert Opin. Biol. Ther. (2011) 11(8) 1063
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

hydrogel for the treatment of MI in rats. They reported a sig-nificant improvement in wall thickness and cardiac function-ality (assessed by histology and hemodynamic measurementsrespectively) of the HA-gel-treated group compared with themyocardial infarction non-treated control group [116].Injectable platforms based on synthetic biomaterial
used for the treatment of MI, include mostly variations of poly(N-isopropylacrylamide) (PNIPAAM) and PEG. PNIPAAM isa synthetic hydrogel that is in a liquid state at room temperatureyet solidifies to a compliant gel form at 37oC. However, PNI-PAAM is non-biodegradable and is not cleared from the bodyat physiological temperature [117]. Thus, several modificationswere explored to enhance its biodegradability by incorporat-ing either natural biodegradable materials (i.e., hyaluronicacid [118], collagen [119], gelatin [120], dextran [117,121] and peptidederivatives [122]) or by copolymerization with synthetic mono-mers having hydrolytic polyester side chains [123,124]. Upon cleav-age of these side chains the polymer hydrophobicity wasincreased, leading to an increase in the lower critical solutiontemperature of the polymer above body temperature enablingpolymer dissolving and physiological clearance. Recently, severalvariations of PNIPAAM have been utilized for the treatmentof MI in rabbit [121,125] and rat models [126] showing overallimprovement in cardiac function, neovascularization andventricular remodeling. Thus the addition of a biodegradabledextran grafted to poly (e-caprolactone)-2-hydroxylethyl-methacrylate (Dex-PCL-HEMA/NIPAAM) yielded a reductionin scar size and wall thinning accompanied by improvement inthe left ventricular ejection fraction and overall cardiac func-tion [121]. Li et al., also incorporated bone marrow mononuclearcells (BMMC) with this composite [125] leading to an increase inneovascular formation. Similar modification to PNIPAAM wasemployed by Fujimoto et al., who evaluated the copolymeriza-tion of NIPAAM, acrylic acid (AAc) and hydroxyethylmethacrylate-poly(trimethylene carbonate) (HEMAPTMC).They assessed a range of monomer ratios, poly(NIPAAm-co-AAc-co-HEMAPTMC), showing that at a feed ratio of86:4:10 the polymer formed a hydrogel at 37� C and in-vitro itgradually became soluble over more than 5 months, throughhydrolytic cleavage of the PTMC residues. Injecting the hydrogelinto rats with chronic infarction has led to the preservationof the LV cavity area and contractility, compared to the controls.Furthermore, tissue ingrowth was observed in the hydrogel-injected area, together with a thicker LVwall and higher capillarydensity. These effects were found in the hydrogel-treated groupand were absent in the PBS-treated controls [126]. Another varia-tion of PNIPAAM in combination with other natural and syn-thetic polymers was recently reported by Wang et al. [127].Hydrogel composites were fabricated from Type I collagen,chondroitin sulfate (CS) and a copolymer based on NIPAAM,AAc, N-acryloxysuccinimide and the macromer poly(trimethy-lene carbonate)-hydroxyethyl methacrylate. These compositeswere capable of being injected through a 26-gauge needle andgelled within 6 sec at 37�C forming highly flexible gels withmoduli matching those of the rat and human myocardium.
Finally, PEG, well known as a commonly used bio-inertmaterial has also been studied as a non-degradable alternativefor MI injection [66]. Nevertheless, injection of PEG-vinylsulfone in a rat MI model, showed no difference in the long-term functional benefit as compared with saline injections [128].As it is believed that PEG’s non-degradability prevents along-term sustainable effect [66], other PEG derivatives thatenable proteolytic degradation have been suggested. Theseinclude, PEGylated fibrinogen [47] and PEGylated fibrinbiomatrix [129] and a hydrogel made out of a-cyclodextrin(a-CD) combined with PEG-b-polycaprolactone-(dodecane-dioic acid)-polycaprolactone-PEG (MPEG-PCL-MPEG) tri-block polymer [130]. Both these biomaterials have shownimproved heart geometry and function upon injection intomouse [129] or rabbit [130] MI models. The effect of thesematerials in larger animal models has yet to be reported.
3. Patch-based platforms
Patch-based platforms, are extensively studied for cardiacregeneration. They are composed of biomaterial either withor without cells, and can be transplanted on the epicardial sur-face of the infarct. They serve as a ‘bag pack’ that contains bio-logical therapeutics and growth factors needed for the supportof the transplanted cells and host tissue, until angiogenesisoccurs and the natural ECM is remodeled by the cells, eventu-ally replacing the artificial patch platform. It is suggested thatwith time, the recruitment of endogenous stem and progeni-tor cells may enable a mechanical and electrical integrationof such a patch with the host myocardium hopefully enablingthe regeneration of the infarcted scar tissue.
Patch deposition requires a more invasive surgical inter-vention in contrast to the relative ease of employment ofthe injection-based platforms. Nevertheless, a recent sideby side comparison between intra-myocardial injections ofskeletal myoblasts, and a patch of skeletal myoblasts in colla-gen foams showed that the latter is much more effective interms of improved cardiac functionality as determined byechocardiography and histological assessment one monthpost transplantation in rats [131].
Two major patch-based platform groups have been dis-cussed in literature; patch-based platforms that are composedof solely cells forming cell sheets and patch-based platformscomposed of synthetic or natural polymers with or withoutthe combination of cells.
3.1 ‘Cells only’-patch based platformsShimizu et al., were the first to report, in 2002, the construc-tion of a cell patch stacked out of four CM monolayers [132].They utilized poly-NIPAAM-coated dishes for the cultivationof neonatal rat cardiomyocytes which were later detached usingtemperature reduction (below 32�C). The engineered con-structs were macroscopically observed to pulse spontaneously,in-vitro, and ‘morphologically communicate’ via connexin43.In-vivo, layered cardiomyocyte sheets were transplanted into
Engineering cell platforms for myocardial regeneration
1064 Expert Opin. Biol. Ther. (2011) 11(8)
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

subcutaneous tissues of nude rats, leading to the formation ofneovasculature. Miyahara et al. transplanted stacked mono-layers of adipose tissue-derived mesenchymal stem cells ontohearts of myocardial infarcted rats [133]. One of their mostimpressive findings was that the monolayers expended,in situ, producing a 600-µm-thick tissue over the infarct scar.This finding contradicted the previously held view that myo-cardial patches could not grow beyond ~ 100 µm due to diffu-sion limitation. Nevertheless, given the thickness of human leftventricles (circa 10 -- 15 mm), this diffusion limitation stillneeds to be surpassed to achieve human cardiac restoration [134].In a more recent work published by the same group, the pro-motion of neovascularization by increasing densities ofco-cultured endothelial cells within the same cell-sheet-basedplatform was studied. In-vivo studies, performed in a MI ratmodel, revealed that the cardiac function was significantlyimproved in correlation with the increase in endothelial celldensities of the original co-cultured constructs. They alsoreported a significant increase in the number of capillaries inthe grafts which connected with the host tissue vasculatureand functionally supplied the grafted construct [135].
A different novel and scalable method, which is a ‘scaffoldfree’-based platformbut in a shape of a patchwas lately developedby Stevens et al. [48,136]. A rotating orbital shaker was used to formmacroscopic disc-shaped 300 -- 600 µm thick beating ESC-derived CM patches having diameters directly proportional toinput cell number [48]. CMs were concentrated around the patchedges and exhibited increased purity and maturation with time(determined by the abundance of b-MHC transcript using quan-titative reverstranscription (RT)-PCR and immunohistologicalstaining). Patches also exhibited automaticity and synchronouscalcium transients, indications of electromechanical coupling.A recent study published by this group, demonstrated that thesepatches, composed only of enriched CM, did not survive to formsignificant grafts after implantation in-vivo in rats [136]. Thus,‘second-generation’ prevascularized, and entirely human patchesfromCM, endothelial cells and fibroblasts were created. Implan-tation of these patches resulted in 10-fold larger cell grafts com-pared with patches composed of CM only. Despite the greatinterest these new technologies have generated, they still needto be tested in large-animal models.
3.2 Synthetic patch-based platformsTwo classes of synthetic materials have been proposed in thelast decade for the generation of patch based platforms: poly-esters and elastomers. Each of these materials has unique char-acteristics in terms of structure and composition. They cangive rise to a family of derivatives with distinct propertiesthorough structural and biochemical modifications, such asdifferent toxicity profiles of their degradation byproductsand various mechanical elasticities and strengths.
3.2.1 PolyestersThe general definition ‘Polyester’ refers to a group of polymers,which contain the ester functional group in their main chain.
Although this term is applicable to many types of materials,we will focus on the ones that are the most commonly usedfor myocardial tissue engineering such as polylactic acid(PLA), polyglycolic acid (PGA) (or their copolymer (PLGA)),poly(a-Hydroxy acid) and poly-e-caprolactone (PCL) [134,137].These polymers are of great interest because their degradationproducts are mostly biocompatible (lactic, glycolic and hydrox-ycarboxylic acids respectively). However, these polymers arenot without flaws. Their degradation products may cause alocal high acidic concentration leading to an inflammatoryresponse, which will impair the targeted tissue [2]. Furthermore,due to their bulk degradation kinetics, a sudden loss of struc-tural integrity is expected and might be less desirable. Nonethe-less, seeing as their mechanical properties, morphology anddegradation kinetics are relatively easy to control, they aresimple to manufacture and so became a most useful tool forpatch-based myocardial tissue engineering research.
Combinations of PLA and PCL (PCLA) were first producedby Ozawa et al., who employed PCLA patches, seeded withsyngeneic rat aortic smooth muscle cells to replace a surgicallycreated defect in the right ventricular outflow tract (RVOT)of rats. Compared with gelatin- and PGA-seeded patches,PCLA patches permitted better cellular penetration in-vitro,did not thin or dilate in vivo and did not produce an inflamma-tory response [138]. Jin et al., have investigated the effect oftransplanted poly(lactide-co-e-caprolactone) (PLCL) scaffoldspre seeded with MSC in a rat MI model. Ten days postimplantation, some transplanted MSCs survived and differenti-ated into cardiomyocytes in the injured region, which wasaccompanied with some 20 -- 30% improvement in cardiacfunction [139].
Notable work using PLGA-based patch platforms wasrecently published by the Levenberg group [9,45], who used atri-culture of ESC-derived CM, endothelial cells and embry-onic fibroblasts to form a synchronously contracting engi-neered human cardiac-like tissue containing endothelialvessel networks [9]. This tissue construct was further assessedin terms of its ability to engraft in-vivo into the rat heartand was found to promote functional vascularization [45].Interestingly, in common with the ‘scaffold free’ techniquediscussed above, the patch thickness did not develop tomore than 600 µm. Even though, this thickness representsalmost half the wall thickness of the rat heart, it is far fromthat required for clinical application. In addition, there isincreasing evidence that successful scaffold materials musthave elastic properties that resemble those of the native heart,allowing them to move in synchrony with every heart beat,thus maintaining their structural integrity. Unfotunately, pol-yesters, are generally less flexible than the heart tissue, hencethere is a requirement for more elastic synthetic materialssuch as ‘elastomers’.
3.2.2 ElastomersElastomers are synthetic mimics of natural rubber. Accordinglythey are defined as synthetic materials that have the ability to
Sarig & Machluf
Expert Opin. Biol. Ther. (2011) 11(8) 1065
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

undergo elastic deformation under the influence of a force andregain their original shape once the force has been removed.A 3D cardiac construct made out of polyurethane (PU), exhib-ited, good cell adhesion in-vitro [140]. Further in-vitro andin-vivo evaluations showed no tissue inflammation and tran-sient inhibition in the progression towards heart failure. Thistransient inhibition was no surprise, as transplanted cells wereundetectable one year post treatment [141,142]. These promisingobservations are flawed by the fact that PU release a toxicbyproduct -- disocyanate that hampers its clinical use [2]. Otherelastomeric materials that were reported as suitable for myocar-dial patch engineering are 1,3 trimethylene carbonate [143] andPEG, which was suggested as a screening method for the opti-mization of tri-culture conditions [144]. A more biocompatibleand absorbable elastomer - poly(glycerol sebacate) (PGS) wasdeveloped by the renowned Langer group in 2002 [145]. Thesame material was recently reported by Chen et al., to supportthe LVs of transplanted rat hearts while serving as an efficientdelivery vehicle for ESC-derived CM [49]. The promise ofthese materials cannot yet be fully judged as to date nolarge-animal studies have been performed.
3.3 Natural patch-based platforms
3.3.1 Extracellular matrixThe use of ECM, as a patch platform for myocardial tissueengineering was introduced by the Badylak group in 2005.They reported the successful implementation of urinarybladder ECM multilaminate as an acellular myocardialpatch that significantly augmented ventricular function incanine and porcine models [146,147]. Further work on acanine RV defect model, demonstrated that the mechanicalfunction generated in the patch region correlates to thequantity of local tissue myocytes infiltration [148]. Neverthe-less, when using the natural ECM, its origin needs to beconsidered as different tissues exhibit different ECM compo-sitions and ultrastructure that may affect the formation ofthe desired tissue [66,149-151]. Therefore, a suitable ECM forcardiac regeneration may be the one that originates fromheart tissue. Such ECM has the potential of better preservingthe unique strutted, woven and coiled structures that enableefficient CM contraction. It may also allow the appropriatecell guidance and differentiation signals, while avoidingnon-favorable remodeling towards other tissue types as alsodiscussed by Badylak et al. [152].Four groups (including our own) independently reported
the successful isolation of cardiac ECM scaffold from rat [150]and from a more human relevant porcine xenogeneicorigin [153-155]. An in-vivo application was reported in a ratMI model by Ott et al., who utilized an impressive perfusiondecellularization technique to obtain an ECM template of anentire rat heart. This ECM was further re-seeded with ratneonatal CM and cultivated in a modified Langendorffapparatus to yield active beating synchronous heart. Hetero-topic transplantation of this cardiac ECM platform in rats,demonstrated that functional connectivity of the vascular
infrastructure is preserved during the decellularization pro-cedure [150]. As the scale up from rat to porcine myocardiumdecellularization is a challenging one, the isolation of por-cine acellular myocaridal ECM was achieved either fromthin (2 -- 3 mm) left ventricular slices [153,155] or by usingperfusion through the inherent vasculature [154]. Nonethe-less, the yellowish appearance of the acellular perfused car-diac tissue in the latter report indicates the need for a moreextensive decellularization technique as demonstrated byOtt et al. [150]. Indeed, large scale acellularity that is sup-ported by an immunogenic evaluation has yet to be achievedto allow large animal model studies to be performed.
Our own group has recently reported a procedure for isolatingporcine myocardial acellular ECM (1 -- 2 mm in thickness) [153].We demonstrated the effectiveness of such decellularization pro-cedure, which selectively removes all inflammation-inducing cel-lular components while preserving much of the ECM (Figure 2).In our studies the decellularization process produced yellow areason the ECM that were indicative of a non-complete decellulari-zation (Figure 2B). As remaining cellular debris is potentiallyimmunogenic [149] and may possibly affect cell attachment andviability, any decellularization process, particularly one of thicktissue, should produce complete acellular ECM and also addressthe remains of the coronary adipose tissue. Moreover when iso-lating a thick heart tissue, the left ventricular tissue can be advan-tageous, as the inherent vasculature can be used for the perfusioncleaning process and can also be proven to be essential for futureconstruction of functional inherent blood vessels by seeding withendothelial cells (Figure 2C). Once having ensured that the ECMis totally acellular, it was evident that it encourages cell growthand cellular remodeling both in-vitro as well as in-vivo (Figure 3).Current work in our lab focuses on the optimization of thisprocedure for thicker tissue specimens that could be potentiallyused as patch material and also for transmural replacementtherapies (Figure 4).
Another approach for obtaining an acellular patch materialis by the decellularization of pericardial matrix as reported byChang et al., [156]. In more recent studies performed by thesame group, mesenchymal stromal cell [157] or MSC mono-layers [158] were sandwiched together with pre cut acellularpericardia to form a multilaminate. This tissue graft (sand-wiched patch) was used not only as a patch, but also as areplacement for the infarcted wall in a syngeneic Lewis ratmodel with chronic MI. At retrieval, the area of the emptypatch serving as control, was relatively enlarged, suggestingreduced structural support while that of the sandwiched patchremained about the same. The sandwiched patches, were pop-ulated with both host and originally seeded cells [157].Whether these results could be scaled up in larger animalmodels where infarct sizes are by far bigger, remains tobe proven.
3.3.2 CollagenThe casting of liquid collagen with neonatal CM into circularmolds yielded in-vitro engineered heart like tissue (EHT) that
Engineering cell platforms for myocardial regeneration
1066 Expert Opin. Biol. Ther. (2011) 11(8)
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

was subsequently electrically [159-161] or mechanically [160,162]
stimulated to create synchronous beating hoops. This EHTwas used for both patch implantation on infarcted immune-suppressed rat hearts [163] as well as to create a novel bio-logical assist device out of a pouch like EHT [164]. Othergroups have also attempted to use collagen-patch-basedplatforms [40,165-166]. Kofidis et al., transplanted a collagen
patch, which was solidified with human ESC-derived CMon an athymic nude rat heterotopic heart transplant model.Their results indicated that the three dimensional matrix pre-vented myocardial wall thinning and improved contractil-ity [40]. In a recent study by Pozzoboen et al., a porouscollagen patch was transplanted on a cryoinjured rat model,and allowed to neo-vascularize for a period of two weeks after
A.
C.
B.
D.
C.
Figure 2. Isolation of porcine cardiac extracellular matrix (ECM). Slices of fresh porcine heart (A.), incomplete decellularized
slices showing retention of cellular debris (Yellow/Brown) marked by an arrow (B.) and clean acellular ECM preserving
structural properties such as blood vessel ECM marked by arrows (C.). Masson tri-chrome staining of representative cross
sections shows high cellular density (red -- cytoplasms) adjacent to ECM fibers (Blue) in native porcine cardiac tissue (D.). No
cellular remains are apparent in the acellular scaffold (E.). Scale bars in D. and E.: 100 µm.
A.
D. E.
B. C.
Figure 3. Cellular remodeling of porcine cardiac extracellular matrix (ECM). Rat neonatal cardiomyocytes (CM) seeded on
porcine cardiac ECM. Immunological staining for a-cardiac actinin (A.) and connexin-43 (B.) at day 7 shows CM organization.
Seeded CM secretes ECM fibers and remodels the acellular scaffold visualized by scanning electron microscopy (C.).
Subcutaneous transplantation in mice shows the transplanted ECM at one-week post transplantation (D.) and 8 weeks post
transplantation (E.). Arrows mark cell penetration and remodeling. Scale bars: A. -- C. 20 µm; D. -- E. 200 µm.
Sarig & Machluf
Expert Opin. Biol. Ther. (2011) 11(8) 1067
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

which, human CD133+ cells were injected directly into thepatch. Their results indicated that this strategy, though suit-able for angiogenesis and arteriogenesis, does not produce bet-ter results, in terms of selective homing and differentiationinto CMs, than the ‘traditional’ method of cell injectioninto the myocardium [166].Simpson et al., have also attempted to assess whether an
epicardially applied, tissue-engineered cardiac patch contain-ing progenitor cells would result in enhanced exogenouscell engraftment [167]. They have embedded human MSC(hMSC) into patches made of rat tail type I collagen andglued this patch to rat MI model hearts using fibrin glue.Although hMSC engraftment, one week post implantationwas about 23 ± 4% of the original seeded quantity,long-term cell survival was not detected at 4 weeks.A patch composed of collagen and Matrigel, was used by
Giraud et al., to deliver skeletal myoblasts into the infarctedmyocardium of rats [168]. The patch was glued onto the myo-cardium using fibrin glue leading to some functional benefits,namely improved systolic heart function, however, skeletalmyoblasts survival rate was low and the arrhythmogenic effectwas not properly monitored [169].
3.3.3 GelatinSeveral studies have reported the use of gelatin for the produc-tion of cardiac patch platforms [137]. Li et al. seeded fetal ven-tricular muscle cells onto a gelatin mesh in-vitro andcultivated it for 7 days prior to implantation on a cryoinjured
rat heart. Although cells survived the transplantation andinterconnected with the native tissue, no analysis of cardiacfunction was made [170]. In a follow-up study, they reportedon increased cellular proliferation and better performancewhen mechanical stress regimes were applied on the gelatinfoam [171].
3.3.4 AlginateAlginate patches were first proposed by Leor et al., who iso-lated and grew fetal rat cardiac cells within 3D porous alginatescaffolds. Scaffolds were manufactured using a freeze dryingtechnique and had 90% porosity with an average pore sizeof 100 µm. Intensive neovascularization was revealed posttransplantation of the alginate scaffold in a rat MI model [172].In more recent studies performed by the same group, similaralginate scaffolds were implanted for 7 days on the omentumto achieve pre-vascularization and than transplanted on a MIrat model. The vascularized cardiac patch showed structuraland electrical integration into host myocardium and inducedthicker scars that prevented further dilatation of the chamberand ventricular dysfunction [173]. In a heterotopic heart trans-plant model similar alginate patches also exhibited improvedleft ventricular function [174].
3.4 Synthetic-and-natural-combined patch platformsDifferent studies exploited the advantages of both the syntheticas well as the natural biomaterials producing bio-syntheticchimeras for the construction of cardiac patches. The in-vitro
A. B.
C.
Figure 4. Perfusion -- decellularization of thick porcine cardiac extracellular matrix ECM. Porcine left ventricle is perfused
through the coronary artery while immersed in the same decellularization solutions for a week. Note the difference in cellular
remains in the perfused area (black arrows) compared with the non-perfused parts that were exposed to the decellularization
solutions only from submerging the tissue in solution (A., white arrows). Hematoxylin and eosin staining of cryosectioned
slices obtained from the dashed square in A. (effective decellularization, B.) and from the continuous square in A. (ineffective
decellularization, C.).
Engineering cell platforms for myocardial regeneration
1068 Expert Opin. Biol. Ther. (2011) 11(8)
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

fate of such scaffolds has been reviewed by [2,33,137]. The currentreview addresses the combined-patch platforms which demon-strated in-vivo success. Krupnick et al., seeded a mixture ofbone marrow-derived MSC, collagen types I and IV andMatri-gel onto a nonwoven polymermeshmade out of PLA reinforcedwith poly(tetrafluoroethylene) (PTFE). This construct was thenheterotopically implanted into infarcted syngenic rat hearts.Their results suggested that this construct is non-immunogenicand biocompatible as minimal intracardiac inflammation wasobserved [175]. Similarly, Fukuhara et al., seeded crude bonemar-row cells (cBMC) onto a bioengineered polyglycolic acid cloth(PGAC) impregnatedwith collagen type I and bFGF. The patchwas subsequently sutured on top of a MI scar tissue of rat heartsdemonstrating improved cardiac function, and a distinct cellularpopulation within the patch material including infiltratinginflammatory cells at 4 weeks post implantation [176].
Siepe et al., produced another interesting combination of syn-thetic and natural polymers, which is composed of polyurethane(PU) patches coatedwith laminin, a natural adhesion and signal-ing glycoprotein of the ECM [141]. When implanted with myo-blasts, this type of patch led to significantly improved heartfunction in a MI rat model as assessed by echocardiography. Itwas concluded that myoblast-seeded PU scaffolds preventedpost--myocardial infarction progression toward heart failurewith the same efficiency as direct intramyocardial injection. Ina follow-up study by the same group, a progression toward heartfailure was significantly prevented for up to 6months after injec-tion of myoblasts and for up to 9 months following biograftimplantation [177]. This effect vanished after 12 months, withimmunohistological examinations revealing the absence oftransplanted myoblasts within the scaffold, thus, suggestingonce more that polymer-based platforms in combination withcells are superior to cell therapy alone. However, the beneficialeffects were transient and are probably dependent on the survivaland viability of the seeded cells [177].
Finally, Miyagi et al., developed a new, biodegradable patchmade of a sponge like inner core (modified Gelfoam, MGF)that encourages cell engraftment and an outer coating of PCLproviding sufficient strength to permit ventricular repair. Usingrat MI model, they demonstrated that animals whose heartswere repaired with untreated Gelfoam died of ventricular rup-ture, while the MGF-treated group had significantly improvedmyocardial systolic function. Further incorporation of cyto-kines (stem cell factor, stromal cell-derived factor-1a) and/orbone-marrow-derived MSC within the patched platform, pro-moted a-smooth muscle actin-positive cells, greater capillaryformation, increased wall thickness and better preserved systolicelastance than MGF alone [178].
4. Future platform technologies
Several emerging technologies in tissue regeneration havebeen recently reported to improve cell survival, differentia-tion, spatial organization and/or biomechanical integrationwith host myocardial tissue upon transplantation. These
include combinations of injection- and patch-basedplatforms [179,180] and the use of either physical (mechanicalstretching [162,171], perfusion [181,182] and electrical [183-189])or biochemical (hypoxic pre-conditioning [190,191])stimulation procedures.
Combinations of patch and injectable platforms exploitboth themechanical support of the patch with the ease of deliveryaccompanying intramyocardial injections. Cortes-Morichettiet al., tested in a mouse MI model, the effect of intrainfarctinjection of human umbilical cord blood mononuclear cells(HUCBS) followed by fixation onto the epicardium of a collagenmatrix seeded with the same cell type. This treatment proved tobe advantageous in terms of post-ischemic ventricular dilationand remodeling, over cell-only or non-seeded-patch-only con-trols [180]. Further proof of concept was later provided using asimilar approach in a Phase I controlled clinical feasibility studyperformed in 20 patients, half of whom received the combinedtreatment (using bone marrow cells) while the rest receivedonly the intra-infarct cell injection. The results indicated thatthe combined strategy appears to improve the efficiency of cellu-lar cardiomyoplasty as the collagen scaffold increased the wallthickness with viable tissue while limiting remodeling andnormalizing cardiac wall stress in the injured regions [179].
Effective bio-mechanical pre-conditioning for collagen (andgelatin) stretching has already been discussed with respect topatch-based platforms above [160,162,171]. Perfusion offersanother approach to exert mechanical stimuli on cells and con-structs. This methodology confers increased mass transfer effi-ciency for nutrient supply and waste products removal [181,182].Radisic et al., employed a custom built bioreactor system todemonstrate that the interstitial flow of culturemedium throughrat neonatal CM-seeded porous collagen scaffold, yielded thick,compact and contractile cardiac constructs. These constructsexhibited physiological densities of metabolically active and via-ble cells containing cardiac markers [182]. Similar observationwere also reported by Dvir et al., who also developed a perfusionbioreactor prototype for alginate based constructs seeded withthe same cell type [181]. The in-vivo evaluation of these perfusionend-products compared with non-perfused controls is still tobe reported.
Another physical condition associated with cardiac celldifferentiation and maturation is that of electro-stimulation.Electrical stimuli have shown increased pre-commitmenttowards cardiac lineages of neonatal cadiomyocytes [185-188],fibroblasts [186], hMSCs [184], skeletal myoblasts [183] andhESC [188,189]. Genovese and colleagues have recentlyshown that electrostimulation induces cardiomyocyte pre-commitment of hMSCs in-vitro and is an effective alternativeto cytokine-induced differentiation. ElectrostimulatedhMSCs have exhibited both morphological and biochemicalchanges, resulting in a shift toward a striated muscle cell phe-notype expressing cardiac specific markers. This partiallydifferentiated phenotype may allow a gradual, ongoing differ-entiation within the cardiac environment thus conveyingpotential advantages in clinical applications. The same group
Sarig & Machluf
Expert Opin. Biol. Ther. (2011) 11(8) 1069
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

further evaluated the effects of in-situ electrostimulation(using biventricular pacemakers) on skeletal myoblasts trans-planted in sheep MI model. Stimulation resulted in a signifi-cant improvement in the ejection fraction and limitation ofleft ventricular dilatation compared with controls. Eventhough the arrhythmogenic nature of skeletal myoblasts is stilla matter of controversy [192], no evident arrhythmias wereobserved in this study, rendering the strategy of skeletal myo-blast electrical stimulation prior to transplantation clinicallyrelevant. Tandon et al., have recently reported the develop-ment of a set of electrical stimulation procedures enablingthe use of modified culture dishes [188]. Such reports wouldhopefully lead to the establishment of standard proceduresthat in turn would enable a better understanding of theelectrical stimulation mechanism of action.Finally, hypoxia (i.e., oxygen starvation) had long been
known to have a considerable effect on the proliferation, dif-ferentiation and maintenance of the cardiovascular systemduring development [193]. As such, the use of hypoxia to pre-condition transplanted cells lead to improved results in termsof increased cell survival and angiogenesis [190,191]. Hu et al.,reported that mouse MSCs grown under hypoxic conditions(0.5% oxygen for 24 h) displayed increased expression ofpro-survival and pro-angiogenic factors (hypoxia induciblefacor 1, angiopoietin-1, vascular endothelial growth factorand its receptor fetal liver kinase 1 (Flk-1), erythropoietin,B cell lymphoma 2 (Bcl-2) and Bcl-2-like X (Bcl-xL)).When transplanted to the peri-infarct region of a rat MImodel, hypoxia preconditioned MSC exhibited higher sur-vival rates leading to an increase in angiogenesis and to othermorphologic and functional benefits, most probably associ-ated with MSC paracrine effects [190]. Similar results werealso recently reported by Wang et al., who demonstratedthat anoxia preconditioning enhanced the capacity of MSCsto repair the infarcted myocardium. This was attributed toincreased cell survival and angiogenesis [191]. This studytogether with other in-vitro evidence concerning the effective-ness of sub-physiological oxygen concentrations on ex-vivocell proliferation, gene expression and commitment [193-198]
may call into question the traditional and standard laboratorycell conditions (i.e., 5% CO2, 95% air) used in most of thestudies mentioned in this report.Taken together, these evolving technologies, offer genuine
opportunity to new discoveries as boundaries of ‘traditional’cell therapy and tissue engineering techniques are beingchallenged to create platforms having actual bio-mimeticproperties in an ex-vivo environment.
5. Expert opinion
The future choice of the cell or cell combinations for heartregenerative cell-based platforms are probably autologous iPSCsand CSCs. These cells offer a genuine clinical alternative mainly
due to their autologous origin and their overall tendency tospontaneously give rise to several supporting cell types includingbeating CM and endothelial cells. Nonetheless, major researchstill needs to be performed towards achieving a robust andtime effective differentiation procedure(s) that enhances theyield of CMproduction with as little genetic interference as pos-sible being introduced. It is expected that clinical trials of in-situ-injectable biomaterial platforms would produce similar results tothose already obtained in large-animal models, showingimproved cardiac function, with the hope of total cardiac regen-eration. Nonetheless, one cannot ignore the promising resultswith cardiac patches. This potential should motivate furtherbasic in-vitro research aiming to deal with several major limita-tions still hampering the production of relevant thick andorganized tissue constructs for patch or infarct replacement ther-apies. These limitations include the lack of cell survival posttransplantation, as it is evident from the data presented hereinthat without cells populating these tissue engineered constructs,no long-term effect can be achieved. Most importantly, the oxy-gen diffusion limitation in culture media, which dictates thatin-vitro produced constructs exhibit inadequate thicknesses forhuman sized hearts. Finally, the static ‘flat tissue culture’ isinappropriate for 3D tissue constructs. Hence a ‘Biomimeticapproach’ to cardiac tissue engineering would probably directthe ‘assembly of functional tissues using biologically deriveddesign requirements’ [34]. Several pivotal reports, reviewedelsewhere [34], have already been published in recent years byleading researchers in this field, such prestigious groups includethose of Robert Langer, Smadar Cohen, Gordana Vunjak-Novakovic, Milica Radisic, Thomas Eschenhagen, WolframHubertus Zimmerman, Juan Carlos Chachques and Alain FCarpentier [35,159,162,163,182-185,187,199-200]. In summary, ourgrowing understanding and ability to supply pulsed-flowfeeding as well as timely mechanical, electrical and biochemicalstimuli would enable the establishment of complementarydynamic cultivation platforms. These will in turn producemore densely populated, thicker and aligned constructsprior to implantation. Furthermore, in-vitro-developed tissueconstructs, serving as cardiac mimetics, would also enablerapid screening of novel therapeutics and their effects oncardiac regeneration.
Acknowledgments
The authors would like to sincerely thank S Irvineand Y Eitan for their help in the preparation of thismanuscript. We would like to acknowledge D Machlouffor contributing Figure 1.
Declaration of interest
The authors state no conflict of interest and have received nopayment in preparation of this manuscript.
Engineering cell platforms for myocardial regeneration
1070 Expert Opin. Biol. Ther. (2011) 11(8)
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

Bibliography
1. Taylor DA, Zenovich AG.
Cardiovascular cell therapy and
endogenous repair.
Diabetes Obes Metab
2008;10(Suppl 4):5-15
2. Jawad H, Lyon AR, Harding SE,
et al. Myocardial tissue engineering.
Br Med Bull 2008;87:31-47
3. Wang F, Guan J. Cellular
cardiomyoplasty and cardiac tissue
engineering for myocardial therapy.
Adv Drug Deliv Rev 2010;62:784-97
4. Gerecht-Nir S, Radisic M, Park H,
et al. Biophysical regulation during
cardiac development and application
to tissue engineering. Int J Dev Biol
2006;50:233-43
5. Bolli P, Chaudhry HW. Molecular
physiology of cardiac regeneration.
Ann NY Acad Sci 2010;1211:113-26
6. Kehat I, Kenyagin-Karsenti D, Snir M,
et al. Human embryonic stem cells can
differentiate into myocytes with
structural and functional properties of
cardiomyocytes. J Clin Invest
2001;108:407-14
7. Boheler KR, Czyz J, Tweedie D,
et al. Differentiation of pluripotent
embryonic stem cells into
cardiomyocytes. Circ Res
2002;91:189-201
8. Behfar A, Perez-Terzic C, Faustino RS,
et al. Cardiopoietic programming of
embryonic stem cells for tumor-free
heart repair. J Exp Med
2007;204:405-20
9. Caspi O, Lesman A, Basevitch Y,
et al. Tissue engineering of vascularized
cardiac muscle from human embryonic
stem cells. Circ Res 2007;100:263-72
10. Arbel G, Caspi O, Huber I, et al.
Methods for human embryonic stem
cells derived cardiomyocytes cultivation,
genetic manipulation, and
transplantation. Methods Mol Biol
2010;660:85-95
11. Xi J, Khalil M, Shishechian N, et al.
Comparison of contractile behavior of
native murine ventricular tissue and
cardiomyocytes derived from
embryonic or induced pluripotent
stem cells. FASEB J 2010;24:2739-51
12. Blin G, Nury D, Stefanovic S, et al.
A purified population of multipotent
cardiovascular progenitors derived from
primate pluripotent stem cells engrafts
in postmyocardial infarcted nonhuman
primates. J Clin Invest
2010;120:1125-39
13. Mauritz C, Schwanke K, Reppel M,
et al. Generation of functional murine
cardiac myocytes from induced
pluripotent stem cells. Circulation
2008;118:507-17
14. Nakagawa M, Koyanagi M, Tanabe K,
et al. Generation of induced pluripotent
stem cells without Myc from mouse
and human fibroblasts. Nat Biotechnol
2008;26:101-6
15. Okita K, Nakagawa M, Hyenjong H,
et al. Generation of mouse induced
pluripotent stem cells without viral
vectors. Science 2008;322:949-53
16. Nelson TJ, Martinez-Fernandez A,
Yamada S, et al. Repair of acute
myocardial infarction by human
stemness factors induced pluripotent
stem cells. Circulation
2009;120:408-16
17. Zwi L, Caspi O, Arbel G, et al.
Cardiomyocyte differentiation of
human induced pluripotent stem
cells. Circulation 2009;120:1513-23
18. Ieda M, Fu JD, Delgado-Olguin P,
et al. Direct reprogramming of
fibroblasts into functional
cardiomyocytes by defined factors.
Cell 2010;142:375-86
19. Makino S, Fukuda K, Miyoshi S,
et al. Cardiomyocytes can be
generated from marrow stromal
cells in vitro. J Clin Invest
1999;103:697-705
20. Tomita S, Li RK, Weisel RD, et al.
Autologous transplantation of bone
marrow cells improves damaged heart
function. Circulation 1999;100:II247-56
21. Toma C, Pittenger MF, Cahill KS,
et al. Human mesenchymal stem cells
differentiate to a cardiomyocyte
phenotype in the adult murine heart.
Circulation 2002;105:93-8
22. Romanov YA, Svintsitskaya VA,
Smirnov VN. Searching for alternative
sources of postnatal human mesenchymal
stem cells: candidate MSC-like cells from
umbilical cord. Stem Cells
2003;21:105-10
23. Prat-Vidal C, Roura S, Farre J,
et al. Umbilical cord blood-derived
stem cells spontaneously express
cardiomyogenic traits. Transplant Proc
2007;39:2434-7
24. Nakanishi C, Yamagishi M, Yamahara K,
et al. Activation of cardiac progenitor
cells through paracrine effects of
mesenchymal stem cells.
Biochem Biophys Res Commun
2008;374:11-16
25. Pereira WC, Khushnooma I,
Madkaikar M, Ghosh K. Reproducible
methodology for the isolation of
mesenchymal stem cells from human
umbilical cord and its potential for
cardiomyocyte generation. J Tissue Eng
Regen Med 2008;2:394-9
26. Labovsky V, Hofer EL, Feldman L,
et al. Cardiomyogenic differentiation of
human bone marrow mesenchymal cells:
role of cardiac extract from neonatal rat
cardiomyocytes. Differentiation
2009;79:93-101
27. He XQ, Chen MS, Li SH, et al.
Co-culture with cardiomyocytes
enhanced the myogenic conversion
of mesenchymal stromal cells in a
dose-dependent manner.
Mol Cell Biochem 2010;339:89-98
28. Beltrami AP, Barlucchi L, Torella D,
et al. Adult cardiac stem cells are
multipotent and support myocardial
regeneration. Cell 2003;114:763-76
29. Davis DR, Kizana E, Terrovitis J,
et al. Isolation and expansion of
functionally-competent cardiac progenitor
cells directly from heart biopsies. J Mol
Cell Cardiol 2010;49:312-21
30. Davis DR, Zhang Y, Smith RR, et al.
Validation of the cardiosphere method to
culture cardiac progenitor cells from
myocardial tissue. PLoS ONE
2009;4:e7195
31. Messina E, De Angelis L, Frati G, et al.
Isolation and expansion of adult cardiac
stem cells from human and murine heart.
Circ Res 2004;95:911-21
32. Smith RR, Barile L, Cho HC, et al.
Regenerative potential of
cardiosphere-derived cells expanded from
percutaneous endomyocardial biopsy
specimens. Circulation
2007;115:896-908
33. Jawad H, Ali NN, Lyon AR, et al.
Myocardial tissue engineering: a review.
J Tissue Eng Regen Med 2007;1:327-42
Sarig & Machluf
Expert Opin. Biol. Ther. (2011) 11(8) 1071
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

34. Grayson WL, Martens TP, Eng GM,
et al. Biomimetic approach to tissue
engineering. Semin Cell Dev Biol
2009;20:665-73
35. Radisic M, Park H, Gerecht S, et al.
Biomimetic approach to cardiac tissue
engineering. Philos Trans R Soc
Lond B Biol Sci 2007;362:1357-68
36. Bonaros N, Rauf R, Schachner T,
et al. Enhanced cell therapy for
ischemic heart disease.
Transplantation 2008;86:1151-60
37. Vandervelde S, van Luyn MJ,
Tio RA, Harmsen MC. Signaling
factors in stem cell-mediated repair
of infarcted myocardium. J Mol
Cell Cardiol 2005;39:363-76
38. Hodgson DM, Behfar A,
Zingman LV, et al. Stable benefit of
embryonic stem cell therapy in
myocardial infarction. Am J Physiol
Heart Circ Physiol 2004;287:H471-9
39. Kehat I, Khimovich L, Caspi O,
et al. Electromechanical integration
of cardiomyocytes derived from
human embryonic stem cells.
Nat Biotechnol 2004;22:1282-9
40. Kofidis T, de Bruin JL, Hoyt G,
et al. Myocardial restoration with
embryonic stem cell bioartificial
tissue transplantation. J Heart
Lung Transplant 2005;24:737-44
41. Laflamme MA, Chen KY,
Naumova AV, et al. Cardiomyocytes
derived from human embryonic stem
cells in pro-survival factors enhance
function of infarcted rat hearts.
Nat Biotechnol 2007;25:1015-24
42. Leor J, Gerecht S, Cohen S, et al.
Human embryonic stem cell
transplantation to repair the infarcted
myocardium. Heart 2007;93:1278-84
43. Nussbaum J, Minami E, Laflamme MA,
et al. Transplantation of undifferentiated
murine embryonic stem cells in the
heart: teratoma formation and
immune response. FASEB J
2007;21:1345-57
44. van Laake LW, Passier R,
Doevendans PA, Mummery CL.
Human embryonic stem cell-derived
cardiomyocytes and cardiac repair in
rodents. Circ Res 2008;102:1008-10
45. Lesman A, Habib M, Caspi O, et al.
Transplantation of a tissue-engineered
human vascularized cardiac muscle.
Tissue Eng Part A 2009;16:115-25
46. Lu WN, Lu SH, Wang HB, et al.
Functional improvement of infarcted
heart by co-injection of embryonic stem
cells with temperature-responsive
chitosan hydrogel. Tissue Eng Part A
2009;15:1437-47
47. Shapira-Schweitzer K, Habib M,
Gepstein L, Seliktar D.
A photopolymerizable hydrogel for 3-D
culture of human embryonic stem
cell-derived cardiomyocytes and rat
neonatal cardiac cells. J Mol Cell Cardiol
2009;46:213-24
48. Stevens KR, Pabon L, Muskheli V,
Murry CE. Scaffold-free human cardiac
tissue patch created from embryonic stem
cells. Tissue Eng Part A
2009;15:1211-22
49. Chen QZ, Ishii H, Thouas GA, et al.
An elastomeric patch derived from poly
(glycerol sebacate) for delivery of
embryonic stem cells to the heart.
Biomaterials 2010;31:3885-93
50. Christoforou N, Oskouei BN, Esteso P,
et al. Implantation of mouse embryonic
stem cell-derived cardiac progenitor cells
preserves function of infarcted murine
hearts. PLoS ONE 2010;5:e11536
51. Lin Q, Fu Q, Zhang Y, et al.
Tumourigenesis in the infarcted rat
heart is eliminated through
differentiation and enrichment of the
transplanted embryonic stem cells.
Eur J Heart Fail 2010;12:1179-85
52. Arminan A, Gandia C,
Garcia-Verdugo JM, et al. Cardiac
transcription factors driven
lineage-specification of adult stem
cells. J Cardiovasc Transl Res
2010;3:61-5
53. Covas DT, Siufi JL, Silva AR,
Orellana MD. Isolation and culture of
umbilical vein mesenchymal stem cells.
Braz J Med Biol Res 2003;36:1179-83
54. Hare JM, Traverse JH, Henry TD,
et al. A randomized, double-blind,
placebo-controlled, dose-escalation
study of intravenous adult human
mesenchymal stem cells (prochymal)
after acute myocardial infarction.
J Am Coll Cardiol 2009;54:2277-86
55. Huang XP, Sun Z, Miyagi Y,
et al. Differentiation of allogeneic
mesenchymal stem cells induces
immunogenicity and limits their
long-term benefits for myocardial
repair. Circulation
2010;122:2419-29
56. Jiang W, Ma A, Wang T, et al.
Intravenous transplantation of
mesenchymal stem cells improves cardiac
performance after acute myocardial
ischemia in female rats. Transpl Int
2006;19:570-80
57. Martin-Rendon E, Sweeney D, Lu F,
et al. 5-Azacytidine-treated human
mesenchymal stem/progenitor cells
derived from umbilical cord, cord blood
and bone marrow do not generate
cardiomyocytes in vitro at high
frequencies. Vox Sang 2008;95:137-48
58. Mastitskaya S, Denecke B. Human
spongiosa mesenchymal stem cells fail to
generate cardiomyocytes in vitro.
J Negat Results Biomed 2009;8:11
59. Molina EJ, Palma J, Gupta D, et al.
Improvement in hemodynamic
performance, exercise capacity,
inflammatory profile, and left ventricular
reverse remodeling after intracoronary
delivery of mesenchymal stem cells in an
experimental model of pressure overload
hypertrophy. J Thorac Cardiovasc Surg
2008;135:292-9.299.e291
60. Nagaya N, Fujii T, Iwase T, et al.
Intravenous administration of
mesenchymal stem cells improves cardiac
function in rats with acute myocardial
infarction through angiogenesis and
myogenesis. Am J Physiol Heart
Circ Physiol 2004;287:H2670-6
61. Poncelet AJ, Hiel AL, Vercruysse J,
et al. Intracardiac allogeneic
mesenchymal stem cell transplantation
elicits neo-angiogenesis in a fully
immunocompetent ischaemic swine
model. Eur J Cardiothorac Surg
2010;38:781-7
62. Quevedo HC, Hatzistergos KE,
Oskouei BN, et al. Allogeneic
mesenchymal stem cells restore cardiac
function in chronic ischemic
cardiomyopathy via trilineage
differentiating capacity. Proc Natl Acad
Sci USA 2009;106:14022-7
63. Schuleri KH, Feigenbaum GS,
Centola M, et al. Autologous
mesenchymal stem cells produce reverse
remodelling in chronic ischaemic
cardiomyopathy. Eur Heart J
2009;30:2722-32
64. Henning RJ, Burgos JD, Vasko M, et al.
Human cord blood cells and myocardial
infarction: effect of dose and route of
administration on infarct size.
Cell Transplant 2007;16:907-17
Engineering cell platforms for myocardial regeneration
1072 Expert Opin. Biol. Ther. (2011) 11(8)
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

65. Orlic D, Kajstura J, Chimenti S, et al.
Bone marrow cells regenerate infarcted
myocardium. Nature 2001;410:701-5
66. Singelyn JM, Christman KL. Injectable
materials for the treatment of myocardial
infarction and heart failure: the promise
of decellularized matrices. J Cardiovasc
Transl Res 2010;3:478-86
67. Wang H, Zhou J, Liu Z, Wang C.
Injectable cardiac tissue engineering for
the treatment of myocardial infarction.
J Cell Mol Med 2010;14:1044-55
68. Piepoli MF, Capucci A. Cardiac
regeneration by progenitor cells:
what is it known as and what is it
still to be known as? Cardiovasc Hematol
Agents
Med Chem 2009;7:127-36
69. Satin J, Kehat I, Caspi O, et al.
Mechanism of spontaneous excitability
in human embryonic stem cell derived
cardiomyocytes. J Physiol
2004;559:479-96
70. Hess PG. Risk of tumorigenesis in
first-in-human trials of embryonic
stem cell neural derivatives: ethics in
the face of long-term uncertainty.
Account Res 2009;16:175-98
71. Fernandes S, Naumova AV, Zhu WZ,
et al. Human embryonic stem
cell-derived cardiomyocytes engraft
but do not alter cardiac remodeling
after chronic infarction in rats.
J Mol Cell Cardiol 2010;49:941-9
72. Mayor S. First patient enters trial to
test safety of stem cells in spinal
injury. BMJ 2010;341:c5724
73. Zwi L, Mizrahi I, Arbel G, et al.
Scalable production of cardiomyocytes
derived from induced pluripotent stem
(iPS) cells without c-Myc. Tissue Eng
Part A 2011;17:1027-37
74. Banito A, Gil J. Induced pluripotent
stem cells and senescence: learning the
biology to improve the technology.
EMBO Rep 2010;11:353-9
75. Arminan A, Gandia C, Bartual M,
et al. Cardiac differentiation is
driven by NKX2.5 and GATA4
nuclear translocation in tissue-specific
mesenchymal stem cells.
Stem Cells Dev 2009;18:907-18
76. Beltrami AP, Urbanek K, Kajstura J,
et al. Evidence that human cardiac
myocytes divide after myocardial
infarction. N Engl J Med
2001;344:1750-7
77. Bergmann O, Bhardwaj RD, Bernard S,
et al. Evidence for cardiomyocyte renewal
in humans. Science 2009;324:98-102
78. Oh H, Bradfute SB, Gallardo TD, et al.
Cardiac progenitor cells from adult
myocardium: homing, differentiation,
and fusion after infarction. Proc Natl
Acad Sci USA 2003;100:12313-18
79. Andersen DC, Andersen P, Schneider M,
et al. Murine "cardiospheres" are not a
source of stem cells with cardiomyogenic
potential. Stem Cells 2009;27:1571-81
80. Cedars-Sinai Medical Center;
CArdiosphere-Derived aUtologous
Stem CElls to Reverse ventricUlar
dySfunction (CADUCEUS).
ClinicalTrials.gov NCT00893360.
Available from: http://www.clinicaltrials.
gov/ct2/show/NCT00893360
81. Martens TP, Godier AF, Parks JJ, et al.
Percutaneous cell delivery into the heart
using hydrogels polymerizing in situ.
Cell Transplant 2009;18:297-304
82. Graham HK, Horn M, Trafford AW.
Extracellular matrix profiles in the
progression to heart failure. European
Young Physiologists Symposium
Keynote Lecture-Bratislava 2007.
Acta Physiol (Oxf) 2008;194:3-21
83. Kofidis T, de Bruin JL, Hoyt G, et al.
Injectable bioartificial myocardial tissue
for large-scale intramural cell transfer
and functional recovery of injured heart
muscle. J Thorac Cardiovasc Surg
2004;128:571-8
84. Kofidis T, Lebl DR, Martinez EC,
et al. Novel injectable bioartificial
tissue facilitates targeted, less invasive,
large-scale tissue restoration on the
beating heart after myocardial injury.
Circulation 2005;112:I173-7
85. Zhang P, Zhang H, Wang H,
et al. Artificial matrix helps neonatal
cardiomyocytes restore injured
myocardium in rats. Artif Organs
2006;30:86-93
86. Singelyn JM, DeQuach JA,
Seif-Naraghi SB, et al. Naturally
derived myocardial matrix as an
injectable scaffold for cardiac tissue
engineering. Biomaterials
2009;30:5409-16
87. Zhao ZQ, Puskas JD, Xu D, et al.
Improvement in cardiac function with
small intestine extracellular matrix is
associated with recruitment of C-kit cells,
myofibroblasts, and macrophages after
myocardial infarction. J Am Coll Cardiol
2010;55:1250-61
88. Shoulders MD, Raines RT. Collagen
structure and stability.
Annu Rev Biochem 2009;78:929-58
89. Dai W, Wold LE, Dow JS, Kloner RA.
Thickening of the infarcted wall by
collagen injection improves left
ventricular function in rats: a novel
approach to preserve cardiac function
after myocardial infarction. J Am
Coll Cardiol 2005;46:714-19
90. Huang NF, Yu J, Sievers R, et al.
Injectable biopolymers enhance
angiogenesis after myocardial infarction.
Tissue Eng 2005;11:1860-6
91. Suuronen EJ, Veinot JP, Wong S, et al.
Tissue-engineered injectable
collagen-based matrices for improved cell
delivery and vascularization of ischemic
tissue using CD133+ progenitors
expanded from the peripheral blood.
Circulation 2006;114:I138-44
92. Kutschka I, Chen IY, Kofidis T, et al.
Collagen matrices enhance survival of
transplanted cardiomyoblasts and
contribute to functional improvement of
ischemic rat hearts. Circulation
2006;114:I167-73
93. Kutschka I, Chen IY, Kofidis T, et al.
In vivo optical bioluminescence imaging
of collagen-supported cardiac cell grafts.
J Heart Lung Transplant 2007;26:273-80
94. Zhang Y, Thorn S, DaSilva JN, et al.
Collagen-based matrices improve the
delivery of transplanted circulating
progenitor cells: development and
demonstration by ex vivo radionuclide
cell labeling and in vivo tracking with
positron-emission tomography.
Circ Cardiovasc Imaging
2008;1:197-204
95. Takehara N, Tsutsumi Y, Tateishi K,
et al. Controlled delivery of basic
fibroblast growth factor promotes human
cardiosphere-derived cell engraftment to
enhance cardiac repair for chronic
myocardial infarction. J Am Coll Cardiol
2008;52:1858-65
96. Leor J, Amsalem Y, Cohen S. Cells,
scaffolds, and molecules for myocardial
tissue engineering. Pharmacol Ther
2005;105:151-63
97. Ahmed TA, Dare EV, Hincke M.
Fibrin: a versatile scaffold for tissue
engineering applications. Tissue Eng Part
B Rev 2008;14:199-215
Sarig & Machluf
Expert Opin. Biol. Ther. (2011) 11(8) 1073
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

98. Chekanov V, Akhtar M, Tchekanov G,
et al. Transplantation of autologous
endothelial cells induces angiogenesis.
Pacing Clin Electrophysiol
2003;26:496-9
99. Christman KL, Fok HH, Sievers RE,
et al. Fibrin glue alone and skeletal
myoblasts in a fibrin scaffold preserve
cardiac function after myocardial
infarction. Tissue Eng 2004;10:403-9
100. Ryu JH, Kim IK, Cho SW, et al.
Implantation of bone marrow
mononuclear cells using injectable
fibrin matrix enhances neovascularization
in infarcted myocardium. Biomaterials
2005;26:319-26
101. Smith JD, Chen A, Ernst LA, et al.
Immobilization of aprotinin to
fibrinogen as a novel method for
controlling degradation of fibrin gels.
Bioconjug Chem 2007;18:695-701
102. Atar D, Huber K, Rupprecht HJ,
et al. Rationale and design of the
‘F.I.R.E.’ study. A multicenter,
double-blind, randomized,
placebo-controlled study
to measure the effect of FX06 (a
fibrin-derived peptide Bbeta15--42 on
ischemia-reperfusion injury in
patients with acute myocardial
infarction undergoing primary
percutaneous coronary intervention.
Cardiology 2007;108:117-23
103. Shachar M, Cohen S. Cardiac tissue
engineering, ex-vivo: design principles
in biomaterials and bioreactors.
Heart Fail Rev 2003;8:271-6
104. Landa N, Miller L, Feinberg MS,
et al. Effect of injectable alginate
implant on cardiac remodeling and
function after recent and old infarcts
in rat. Circulation 2008;117:1388-96
105. Tsur-Gang O, Ruvinov E, Landa N,
et al. The effects of peptide-based
modification of alginate on left
ventricular remodeling and function
after myocardial infarction.
Biomaterials 2009;30:189-95
106. Yu J, Christman KL, Chin E,
et al. Restoration of left ventricular
geometry and improvement of left
ventricular function in a rodent model
of chronic ischemic cardiomyopathy.
J Thorac Cardiovasc Surg
2009;137:180-7
107. Leor J, Tuvia S, Guetta V, et al.
Intracoronary injection of in situ forming
alginate hydrogel reverses left ventricular
remodeling after myocardial infarction
in Swine. J Am Coll Cardiol
2009;54:1014-23
108. Ruvinov E, Leor J, Cohen S. The
promotion of myocardial repair by the
sequential delivery of IGF-1 and HGF
from an injectable alginate biomaterial
in a model of acute myocardial
infarction. Biomaterials 2011;32:565-78
109. Ikaria Holdings, Inc. IK-5001 for the
Prevention of Remodeling of the
Ventricle and Congestive Heart Failure
After Acute Myocardial Infarction
(PRESERVATION I). ClinicalTrials.gov
NCT01226563. Available from: http://
www.clinicaltrials.gov/ct2/show/
NCT01226563
110. Kim IY, Seo SJ, Moon HS, et al.
Chitosan and its derivatives for tissue
engineering applications. Biotechnol Adv
2008;26:1-21
111. Cho YI, Park S, Jeong SY, Yoo HS. In
vivo and in vitro anti-cancer activity of
thermo-sensitive and photo-crosslinkable
doxorubicin hydrogels composed of
chitosan-doxorubicin conjugates. Eur J
Pharm Biopharm 2009;73:59-65
112. Hu X, Gao C. Photoinitiating
polymerization to prepare
biocompatible chitosan hydrogels.
J Appl Polym Sci
2008;110:1059-67
113. Lu S, Wang H, Lu W, et al.
Both the transplantation of somatic
cell nuclear transfer- and
fertilization-derived mouse embryonic
stem cells with temperature-responsive
chitosan hydrogel improve myocardial
performance in infarcted rat hearts.
Tissue Eng Part A 2010;16:1303-15
114. Chupa JM, Foster AM, Sumner SR,
et al. Vascular cell responses to
polysaccharide materials: in vitro and
in vivo evaluations. Biomaterials
2000;21:2315-22
115. Davis ME, Motion JP, Narmoneva DA,
et al. Injectable self-assembling peptide
nanofibers create intramyocardial
microenvironments for endothelial cells.
Circulation 2005;111:442-50
116. Yoon SJ, Fang YH, Lim CH, et al.
Regeneration of ischemic heart using
hyaluronic acid-based injectable
hydrogel. J Biomed Mater Res B
Appl Biomater 2009;91:163-71
117. Wu DQ, Qiu F, Wang T, et al.
Toward the development of
partially biodegradable and injectable
thermoresponsive hydrogels for potential
biomedical applications. ACS Appl
Mater Interfaces 2009;1:319-27
118. Ohya S, Nakayama Y, Matsuda T.
Thermoresponsive artificial extracellular
matrix for tissue engineering: hyaluronic
acid bioconjugated with poly(N-
isopropylacrylamide) grafts.
Biomacromolecules 2001;2:856-63
119. Li F, Carlsson D, Lohmann C, et al.
Cellular and nerve regeneration within
a biosynthetic extracellular matrix for
corneal transplantation. Proc Natl Acad
Sci USA 2003;100:15346-51
120. Ohya S, Matsuda T. Poly(N-
isopropylacrylamide) (PNIPAM)-grafted
gelatin as thermoresponsive
three-dimensional artificial extracellular
matrix: molecular and formulation
parameters vs. cell proliferation potential.
J Biomater Sci Polym Ed
2005;16:809-27
121. Wang T, Wu DQ, Jiang XJ, et al.
Novel thermosensitive hydrogel
injection inhibits post-infarct ventricle
remodelling. Eur J Heart Fail
2009;11:14-19
122. Kim S, Chung EH, Gilbert M,
Healy KE. Synthetic
MMP-13 degradable ECMs based on
poly(N-isopropylacrylamide-co-acrylic
acid) semi-interpenetrating polymer
networks. I. Degradation and cell
migration. J Biomed Mater Res A
2005;75:73-88
123. Lee BH, Vernon B. In situ-gelling,
erodible N-isopropylacrylamide
copolymers. Macromol Biosci
2005;5:629-35
124. Lee BH, Vernon B. Copolymers of N
isopropylacrylamide, HEMA lactate and
acrylic acid with time dependent lower
critical solution temperature as a
bioresorbable carrier. Polym Int
2005;54:418-22
125. Li XY, Wang T, Jiang XJ, et al.
Injectable hydrogel helps bone
marrow-derived mononuclear cells restore
infarcted myocardium. Cardiology
2010;115:194-9
126. Fujimoto KL, Ma Z, Nelson DM, et al.
Synthesis, characterization and
therapeutic efficacy of a biodegradable,
thermoresponsive hydrogel designed for
application in chronic infarcted
myocardium. Biomaterials
2009;30:4357-68
Engineering cell platforms for myocardial regeneration
1074 Expert Opin. Biol. Ther. (2011) 11(8)
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

127. Wang F, Li Z, Khan M, et al. Injectable,
rapid gelling and highly flexible hydrogel
composites as growth factor and cell
carriers. Acta Biomater 2010;6:1978-91
128. Dobner S, Bezuidenhout D, Govender P,
et al. A synthetic non-degradable
polyethylene glycol hydrogel retards
adverse post-infarct left ventricular
remodeling. J Card Fail 2009;15:629-36
129. Zhang G, Hu Q, Braunlin EA, et al.
Enhancing efficacy of stem cell
transplantation to the heart with a
PEGylated fibrin biomatrix.
Tissue Eng Part A 2008;14:1025-36
130. Jiang XJ, Wang T, Li XY, et al.
Injection of a novel synthetic hydrogel
preserves left ventricle function after
myocardial infarction. J Biomed Mater
Res A 2009;90:472-7
131. Hamdi H, Furuta A, Bellamy V, et al.
Cell delivery: intramyocardial injections
or epicardial deposition? A head-to-head
comparison. Ann Thorac Surg
2009;87:1196-203
132. Shimizu T, Yamato M, Isoi Y, et al.
Fabrication of pulsatile cardiac tissue
grafts using a novel 3-dimensional cell
sheet manipulation technique and
temperature-responsive cell culture
surfaces. Circ Res 2002;90:e40-8
133. Miyahara Y, Nagaya N, Kataoka M,
et al. Monolayered mesenchymal stem
cells repair scarred myocardium after
myocardial infarction. Nat Med
2006;12:459-65
134. Christman KL. Lee, RJ: Biomaterials
for the treatment of myocardial
infarction. J Am Coll Cardiol
2006;48:907-13
135. Sekine H, Shimizu T, Hobo K,
et al. Endothelial cell coculture within
tissue-engineered cardiomyocyte sheets
enhances neovascularization and
improves cardiac function of ischemic
hearts. Circulation 2008;118:S145-52
136. Stevens KR, Kreutziger KL, Dupras SK,
et al. Physiological function and
transplantation of scaffold-free and
vascularized human cardiac muscle tissue.
Proc Natl Acad Sci USA
2009;106:16568-73
137. Giraud MN, Armbruster C, Carrel T,
Tevaearai HT. Current state of the art
in myocardial tissue engineering.
Tissue Eng 2007;13:1825-36
138. Ozawa T, Mickle DA, Weisel RD,
et al. Optimal biomaterial for creation
of autologous cardiac grafts. Circulation
2002;106:I176-82
139. Jin J, Jeong SI, Shin YM, et al.
Transplantation of mesenchymal stem
cells within a poly(lactide-co-e-caprolactone) scaffold improves cardiac
function in a rat myocardial infarction
model. Eur J Heart Fail 2009;11:147-53
140. McDevitt TC, Woodhouse KA.
Hauschka, SD et al. Spatially organized
layers of cardiomyocytes on
biodegradable polyurethane films for
myocardial repair. J Biomed Mater Res A
2003;66:586-95
141. Siepe M, Giraud MN, Pavlovic M, et al.
Myoblast-seeded biodegradable scaffolds
to prevent post-myocardial infarction
evolution toward heart failure. J Thorac
Cardiovasc Surg 2006;132:124-31
142. Giraud MN, Flueckiger R, Cook S,
et al. Long-term evaluation of myoblast
seeded patches implanted on infarcted
rat hearts. Artif Organs 2010;34:E184-92
143. Pego AP, Van Luyn MJ, Brouwer LA,
et al. In vivo behavior of poly
(1,3-trimethylene carbonate) and
copolymers of 1,3-trimethylene
carbonate with D,L-lactide or e-caprolactone: Degradation and tissue
response. J Biomed Mater Res A
2003;67:1044-54
144. Iyer RK, Chiu LL, Radisic M.
Microfabricated poly(ethylene glycol)
templates enable rapid screening of
triculture conditions for cardiac tissue
engineering. J Biomed Mater Res A
2009;89:616-31
145. Wang Y, Ameer GA, Sheppard BJ,
Langer R. A tough biodegradable
elastomer. Nat Biotechnol 2002;20:602-6
146. Kochupura PV, Azeloglu EU, Kelly DJ,
et al. Tissue-engineered myocardial patch
derived from extracellular matrix provides
regional mechanical function. Circulation
2005;112:I144-9
147. Robinson KA, Li J, Mathison M, et al.
Extracellular matrix scaffold for cardiac
repair. Circulation 2005;112:I135-43
148. Kelly DJ, Rosen AB, Schuldt AJ, et al.
Increased myocyte content and
mechanical function within a
tissue-engineered myocardial patch
following implantation. Tissue Eng
Part A 2009;15:2189-201
149. Gilbert TW, Sellaro TL, Badylak SF.
Decellularization of tissues and organs.
Biomaterials 2006;27:3675-83
150. Ott HC, Matthiesen TS, Goh SK,
et al. Perfusion-decellularized matrix:
using nature’s platform to engineer
a bioartificial heart. Nat Med
2008;14:213-21
151. McCurdy S, Baicu CF, Heymans S,
Bradshaw AD. Cardiac extracellular
matrix remodeling: fibrillar collagens
and Secreted Protein Acidic and Rich in
Cysteine (SPARC). J Mol Cell Cardiol
2010;48:544-9
152. Badylak S, Obermiller J, Geddes L,
Matheny R. Extracellular matrix for
myocardial repair. Heart Surg Forum
2003;6:E20-6
153. Eitan Y, Sarig U, Dahan N, Machluf M.
Acellular cardiac extracellular matrix as a
scaffold for tissue engineering: in vitro
cell support, remodeling, and
biocompatibility. Tissue Eng Part
C Methods 2009;16:671-83
154. Wainwright JM, Czajka CA, Patel UB,
et al. Preparation of cardiac extracellular
matrix from an intact porcine heart.
Tissue Eng Part C Methods
2010;16:525-32
155. Wang B, Borazjani A, Tahai M, et al.
Fabrication of cardiac patch with
decellularized porcine myocardial scaffold
and bone marrow mononuclear cells.
J Biomed Mater Res A 2010;94:1100-10
156. Chang Y, Tsai CC, Liang HC,
Sung HW. In vivo evaluation of cellular
and acellular bovine pericardia fixed with
a naturally occurring crosslinking agent
(genipin). Biomaterials 2002;23:2447-57
157. Chen CH, Wei HJ, Lin WW, et al.
Porous tissue grafts sandwiched with
multilayered mesenchymal stromal cell
sheets induce tissue regeneration for
cardiac repair. Cardiovasc Res
2008;80:88-95
158. Wei HJ, Chen CH, Lee WY, et al.
Bioengineered cardiac patch constructed
from multilayered mesenchymal stem
cells for myocardial repair. Biomaterials
2008;29:3547-56
159. Eschenhagen T, Fink C, Remmers U,
et al. Three-dimensional reconstitution of
embryonic cardiomyocytes in a collagen
matrix: a new heart muscle model
system. FASEB J 1997;11:683-94
160. Kofidis T, Akhyari P, Boublik J, et al. In
vitro engineering of heart muscle:
artificial myocardial tissue. J Thorac
Cardiovasc Surg 2002;124:63-9
Sarig & Machluf
Expert Opin. Biol. Ther. (2011) 11(8) 1075
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

161. Zimmermann WH, Fink C, Kralisch D,
et al. Three-dimensional engineered heart
tissue from neonatal rat cardiac
myocytes. Biotechnol Bioeng
2000;68:106-14
162. Zimmermann WH, Schneiderbanger K,
Schubert P, et al. Tissue engineering of
a differentiated cardiac muscle construct.
Circ Res 2002;90:223-30
163. Zimmermann WH, Melnychenko I,
Wasmeier G, et al. Engineered heart
tissue grafts improve systolic and
diastolic function in infarcted rat
hearts. Nat Med 2006;12:452-8
164. Yildirim Y, Naito H, Didie M, et al.
Development of a biological ventricular
assist device: preliminary data from a
small animal model. Circulation
2007;116:I16-23
165. Callegari A, Bollini S, Iop L, et al.
Neovascularization induced by porous
collagen scaffold implanted on intact
and cryoinjured rat hearts. Biomaterials
2007;28:5449-61
166. Pozzobon M, Bollini S, Iop L, et al.
Human bone marrow-derived
CD133+ cells delivered to a collagen
patch on cryoinjured rat heart
promote angiogenesis and arteriogenesis.
Cell Transplant 2010;19:1247-60
167. Simpson D, Liu H, Fan TH, et al.
A tissue engineering approach to
progenitor cell delivery results in
significant cell engraftment and
improved myocardial remodeling.
Stem Cells 2007;25:2350-7
168. Giraud MN, Ayuni E, Cook S,
et al. Hydrogel-based engineered
skeletal muscle grafts normalize heart
function early after myocardial
infarction. Artif Organs
2008;32:692-700
169. Kanwal S, Malik N, Singh J, et al. Re:
Hydrogel-based engineered skeletal
muscle grafts normalize heart function
early after myocardial infarction.
Artif Organs
2009;33:87-author reply 87 -- 88
170. Li RK, Jia ZQ, Weisel RD, et al.
Survival and function of bioengineered
cardiac grafts. Circulation
1999;100(19 Suppl):II63-9
171. Akhyari P, Fedak PW, Weisel RD,
et al. Mechanical stretch regimen
enhances the formation of bioengineered
autologous cardiac muscle grafts.
Circulation 2002;106:I137-42
172. Leor J, Aboulafia-Etzion S, Dar A,
et al. Bioengineered cardiac grafts:
A new approach to repair the infarcted
myocardium? Circulation
2000;102:III56-61
173. Dvir T, Kedem A, Ruvinov E, et al.
Prevascularization of cardiac patch on
the omentum improves its therapeutic
outcome. Proc Natl Acad Sci USA
2009;106:14990-5
174. Amir G, Miller L, Shachar M, et al.
Evaluation of a peritoneal-generated
cardiac patch in a rat model of
heterotopic heart transplantation.
Cell Transplant 2009;18:275-82
175. Krupnick AS, Kreisel D, Engels FH,
et al. A novel small animal model of left
ventricular tissue engineering. J Heart
Lung Transplant 2002;21:233-43
176. Fukuhara S, Tomita S, Nakatani T,
et al. Bone marrow cell-seeded
biodegradable polymeric scaffold
enhances angiogenesis and improves
function of the infarcted heart.
Circ J 2005;69:850-7
177. Giraud MN, Flueckiger R, Cook S,
et al. Long-term evaluation of myoblast
seeded patches implanted on infarcted
rat hearts. Artif Organs
2010;34:E184-92
178. Miyagi Y, Zeng F, Huang XP, et al.
Surgical ventricular restoration with a
cell- and cytokine-seeded biodegradable
scaffold. Biomaterials 2010;31:7684-94
179. Chachques JC, Trainini JC, Lago N,
et al. Myocardial Assistance by
Grafting a New Bioartificial Upgraded
Myocardium (MAGNUM trial): clinical
feasibility study. Ann Thorac Surg
2008;85:901-8
180. Cortes-Morichetti M, Frati G,
Schussler O, et al. Association between
a cell-seeded collagen matrix and cellular
cardiomyoplasty for myocardial support
and regeneration. Tissue Eng
2007;13:2681-7
181. Dvir T, Benishti N, Shachar M,
Cohen S. A novel perfusion bioreactor
providing a homogenous milieu for tissue
regeneration. Tissue Eng
2006;12:2843-52
182. Radisic M, Yang L, Boublik J, et al.
Medium perfusion enables engineering
of compact and contractile cardiac tissue.
Am J Physiol Heart Circ Physiol
2004;286:H507-16
183. Shafy A, Lavergne T, Latremouille C,
et al. Association of electrostimulation
with cell transplantation in ischemic
heart disease. J Thorac Cardiovasc Surg
2009;138:994-1001
184. Genovese JA, Spadaccio C, Chachques E,
et al. Cardiac pre-differentiation of
human mesenchymal stem cells by
electrostimulation. Front Biosci
2009;14:2996-3002
185. Radisic M, Park H, Shing H, et al.
Functional assembly of engineered
myocardium by electrical stimulation of
cardiac myocytes cultured on scaffolds.
Proc Natl Acad Sci USA
2004;101:18129-34
186. Au HTH, Cheng I, Chowdhury MF,
Radisic M. Interactive effects of surface
topography and pulsatile electrical field
stimulation on orientation and
elongation of fibroblasts and
cardiomyocytes. Biomaterials
2007;28:4277-93
187. Barash Y, Dvir T, Tandeitnik P, et al.
Electric field stimulation integrated into
perfusion bioreactor for cardiac tissue
engineering. Tissue Eng Part C Methods
2010;16:1417-26
188. Tandon N, Cannizzaro C, Chao PH,
et al. Electrical stimulation systems for
cardiac tissue engineering. Nat Protoc
2009;4:155-73
189. Serena E, Figallo E, Tandon N, et al.
Electrical stimulation of human
embryonic stem cells: cardiac
differentiation and the generation of
reactive oxygen species. Exp Cell Res
2009;315:3611-19
190. Hu X, Yu SP, Fraser JL, et al.
Transplantation of
hypoxia-preconditioned mesenchymal
stem cells improves infarcted heart
function via enhanced survival of
implanted cells and angiogenesis.
J Thorac Cardiovasc Surg
2008;135:799-808
191. Wang JA, He A, Hu X, et al.
Anoxic preconditioning: a way to
enhance the cardioprotection of
mesenchymal stem cells. Int J Cardiol
2009;133:410-12
192. Gepstein L, Ding C, Rehemedula D,
et al. In vivo assessment of the
electrophysiological integration and
arrhythmogenic risk of myocardial cell
transplantation strategies. Stem Cells
2010;28:2151-61
Engineering cell platforms for myocardial regeneration
1076 Expert Opin. Biol. Ther. (2011) 11(8)
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.

193. Ng KM, Lee YK, Chan YC, et al.
Exogenous expression of HIF-1alpha
promotes cardiac differentiation of
embryonic stem cells. J Mol Cell Cardiol
2010;48:1129-37
194. Bianco C, Cotten C, Lonardo E, et al.
Cripto-1 is required for hypoxia to
induce cardiac differentiation of mouse
embryonic stem cells. Am J Pathol
2009;175:2146-58
195. Iyer NV, Kotch LE, Agani F, et al.
Cellular and developmental control of
O2 homeostasis by hypoxia-inducible
factor 1a. Genes Dev 1998;12:149-62
196. Wang JA, Chen TL, Jiang J, et al.
Hypoxic preconditioning attenuates
hypoxia/reoxygenation-induced
apoptosis in mesenchymal stem cells.
Acta Pharmacol Sin 2008;29:74-82
197. Wang S, Zhou Y, Seavey CN, et al.
Rapid and dynamic alterations of gene
expression profiles of adult porcine bone
marrow-derived stem cell in response to
hypoxia. Stem Cell Res 2010;4:117-28
198. Chacko SM, Ahmed S, Selvendiran K,
et al. Hypoxic preconditioning induces
the expression of prosurvival and
proangiogenic markers in mesenchymal
stem cells. Am J Physiol Cell Physiol
2011;299:C1562-70
199. Khademhosseini A, Eng G, Yeh J,
et al. Microfluidic patterning for
fabrication of contractile cardiac
organoids. Biomed Microdevices
2007;9:149-57
200. Radisic M, Park H, Chen F, et al.
Biomimetic approach to cardiac
tissue engineering: oxygen carriers and
channeled scaffolds. Tissue Eng
2006;12:2077-91
AffiliationUdi Sarig & Marcelle Machluf†
†Author for correspondence
Technion--Israel Institute of Technology,
The Laboratory of Cancer,
Drug Delivery & Mammalian Cell Technology,
Faculty of Biotechnology & Food Engineering,
Haifa 32000, Israel
Tel: +972 4 8294916/3079;
Fax: +972 4 8293399;
E-mail: [email protected]
Sarig & Machluf
Expert Opin. Biol. Ther. (2011) 11(8) 1077
Exp
ert O
pin.
Bio
l. T
her.
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
Heb
rew
Uni
vers
ity o
n 11
/28/
11Fo
r pe
rson
al u
se o
nly.
Related Documents