THE COMMONWEALTH FUND Why Not the Best? Results from the National Scorecard on U.S. Health System Performance, 2011 Cathy Schoen, Senior Vice President The Commonwealth Fund www.commonwealthfund.org [email protected] October 18, 2011

THE COMMONWEALTH FUND Why Not the Best? Results from the National Scorecard on U.S. Health System Performance, 2011 Cathy Schoen, Senior Vice President.
Mar 27, 2015
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

THE COMMONWEALTH
FUND
Why Not the Best? Results from the National Scorecard
on U.S. Health System Performance, 2011
Cathy Schoen, Senior Vice President
The Commonwealth Fundwww.commonwealthfund.org
October 18, 2011

22011 Scorecard Methodology
• Third edition: same framework and methods as previous editions– Five dimensions of health system performance: healthy lives,
quality, access, efficiency, and equity– 42 indicators of health system performance
• Scores are simple ratios of U.S. average to benchmark– Benchmarks are levels achieved by other countries or top U.S.
states, regions, health plans, or providers (select indicators have policy goals or targets)
– Updates benchmarks whenever they improved
• To score dimensions, we average ratio scores for all indicators within dimension; dimension scores are then averaged for overall score
• Time trends capture at least three years of data; more than two-thirds span 5+ years
• Data primarily up through 2009, before reform

32011 Scorecard Overview Findings: Overall Score is 64 out of 100
• Overall U.S. health system performance relative to benchmarks failed to improve between 2006 and 2011 scorecards
– Performance compared with benchmarks improved on less than half of indicators
– Wide disparities by income, race/ethnicity persist
• Steep declines in access and affordability
• Substantial variation across the U.S., with as much as fourfold spread
• Uneven performance on quality, yet encouraging pockets of improvement
– Rapid progress on quality metrics that have been focus of national initiatives and public reporting
– Improvement on key quality metrics demonstrates significant progress possible when specific goals and targets set
• Broad evidence of inefficient care and high costs
• Substantial potential to improveTHE
COMMONWEALTH FUND

4
Average spending on healthper capita ($US PPP)
Total expenditures on healthas percent of GDP
*PPP= Purchasing power paritySource: OECD Health Data 2011 (June 2011).
International Comparison of Spending on Health, 1980–2009
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011.

5Scores: Dimensions of a High Performance Health System
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011.
* Note: Includes indicator(s) not available in earlier years.
75
70
67
52
69
67
73
71
57
53
71
65
70
75
55
53
69
64
0 100
Healthy Lives
Quality
Access
Efficiency
Equity
OVERALL SCORE
2006 revised
2008 revised
2011

6
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011.
76
88 8981
88
99 97
109116
106
97
134
115 113
127120
55 57 60 61 61 64 66 67 74 76 77 78 79 80 8396
0
50
100
150 1997–98 2006–07
Deaths per 100,000 population*
* Countries’ age-standardized death rates before age 75; including ischemic heart disease, diabetes, stroke, and bacterial infections.See Appendix B for list of all conditions considered amenable to health care in the analysis.Data: E. Nolte, RAND Europe, and M. McKee, London School of Hygiene and Tropical Medicine, analysis of World Health Organization mortality files and CDC mortality data for U.S. (Nolte and McKee, 2011).
Mortality Amenable to Health Care

7
7.2 7.0 6.9 6.8 7.0 6.8 6.8 6.9 6.7 6.8
10.311.1
10.2 9.9 9.9 9.610.1
10.810.0 9.9
5.3 5.1 5.0 4.9 4.8 4.7 4.7 5.0 5.0 5.0
0
4
8
12
U.S. average Bottom 10% states Top 10% states
International Comparison, 2007
2.02.5 2.6 2.7
3.1
4.0
5.1
6.8
Infant Mortality RateInfant deaths per 1,000 live births
^ Denotes years in 2006 and 2008 National Scorecards.Data: National and state—National Vital Statistics System, Linked Birth and Infant Death Data (AHRQ 2003–2008; Mathews and MacDorman, 2011); international comparison—OECD Health Data 2011 (database), Version 06/2011.
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011.
U.S. National and State Trends

8Percent of Adults Ages 19–64 Uninsured by State
Data: U.S. Census Bureau, 2000–01 (revised) and 2010–11 Current Population Survey ASEC Supplement.
1999–2000median = 15.0%
2009–2010median = 19.4%
19%–22.9%
Less than 14%
14%–18.9%
23% or more
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011.

9Steep Decline in Access: 81 Million Uninsured and
Underinsured Adults, Up from 61 Million in 2003
9
Percent of adults ages 19–64 who are uninsured or underinsured
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011.
Insured all year, not underinsured
Underinsured*
Uninsured during year
Millions of adults ages 19–64 who are uninsured or underinsured, 2010
102
29
52
Total: 184 million**
35
42 44
* Underinsured defined as insured all year but experienced one of the following: medical expenses equaled 10% or more of income; medical expenses equaled 5% or more of income if low-income (<200% of poverty); or deductibles equaled 5% or more of income.** Subgroups may not sum to total because of rounding.Data: 2003, 2007, and 2010 Commonwealth Fund Biennial Health Insurance Surveys.

10
Employer Premiums as Percentage of Median Household Income for Population Under Age 65
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011. 10
2003 2009
15%–17.9%
Less than 12%
12%–14.9%
18% or more
Data: Average total premiums—2003, 2005, and 2009 Medical Expenditure Panel Survey; state median income for single and family households (all under age 65) —2003–2004, 2005–2006, and 2009-2010 Current Population Survey.
WA
OR
ID
MT ND
WY
NV
CAUT
AZNM
KS
NE
MN
MO
WI
TX
IA
IL IN
AR
LA
AL
SC
TNNC
KY
FL
OH
MI
WV
PA
NY
AK
MEVTNH
MA
RI
DE
DC
HI
CO
GAMS
OK
NJ
SD
VA
CT
MD
WA
OR
ID
MT ND
WY
NV
CAUT
AZNM
KS
NE
MN
MO
WI
TX
IA
IL IN
AR
LA
AL
SC
TNNC
KY
FL
OH
MI
WV
PA
NY
AK
MEVTNH
MA
RI
DE
DC
HI
CO
GAMS
OK
NJ
SD
VA
CT
MD
HI HI

11
31
45
27
6066
53
Total Under 200% ofpoverty
200% of poverty ormore
Insured all year Uninsured during year
3440
0
25
50
75
100
2005 2010
Medical Bill Problems or Medical Debt, 2010
By income and insurance status, 2010U.S. average
Percent of adults ages 19–64 with any medical bill problem or outstanding debt*
* Problems paying or unable to pay medical bills, contacted by a collection agency for medical bills, had to change way of life to pay bills, or has medical debt being paid off over time.Data: 2005 and 2010 Commonwealth Fund Biennial Health Insurance Surveys.
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011.

12
45
64
55
53
55
55
60
45
56
63
42
0 20 40 60 80 100
Uninsured part year
Insured all year
<200% of poverty
200%–399% of poverty
400%+ of poverty
Hispanic
Black
White
2008
2005
2002
U.S. Variation 2008
U.S. Average
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011.
Percent of adults ages 19–64 with an accessible primary care provider*
Adults with an Accessible Primary Care Provider
* An accessible primary care provider is defined as a usual source of care who provides preventive care, care for new and ongoing health problems, referrals, and who is easy to get to and easy to contact by phone during regular office hours.Data: N. Tilipman, Columbia University analysis of Medical Expenditure Panel Survey.

13Receipt of Recommended Screening and Preventive
Care for Adults
* Recommended care includes at least six key screening and preventive services: blood pressure, cholesterol, Pap, mammogram,fecal occult blood test or sigmoidoscopy/colonoscopy, and flu shot. See Appendix B for complete description.Data: N. Tilipman, Columbia University analysis of Medical Expenditure Panel Survey.
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011.
32
46
56
41
49
60
51
50
49
0 20 40 60 80 100
Uninsured all year
Uninsured part year
Insured all year
<200% of poverty
200%–399% of poverty
400%+ of poverty
2008
2005
2002
U.S. Variation 2008
U.S. Average
Percent of adults age 18+ who received all recommended screening and preventive care within a specific time frame given their age and sex*

14
Chronic Disease Under Control: Diabetes and Hypertension
85
49
76
55
72
29
Diabetes under control* High blood pressure undercontrol**
Private Public Uninsured
*Refers to diabetic adults whose hemoglobin A1c is <9.0% **Refers to hypertensive adults whose blood pressure is <140/90 mmHg. Data: J. M. McWilliams, Harvard Medical School analysis of National Health and Nutrition Examination Survey.
79
31
88
41
86
50
0
25
50
75
100
Diabetes under control* High blood pressure undercontrol**
1999–2000 2003–2004 2007–2008
Percent of adults age 18+
U.S. Average By Insurance, 2005–2008
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011.
Percent of nonelderly adults ages 18–64

15
87
59
49
9389
83
74
66
98 97 96 9490
71
81
0
25
50
75
100
90th %ile 75th %ile Median 25th %ile 10th %ile
2004 2006 2009
Hospitals: Prevention of Surgical Complications
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011.
Percent of adult surgical patients who received appropriate care to prevent complications*
* See Appendix B for methods and description of clinical indicators.Data: IPRO analysis of data from CMS Hospital Compare.

16
Prescription of Potentially Unsafe Medications Among Elderly Beneficiaries, by Hospital Referral Regions, 2007
25
1821
31
36
0
10
20
30
40
50
Median 10th %ile 25th %ile 75th %ile 90th %ile
Percent of elderly Medicare beneficiaries
20
1517
23
26
Median 10th %ile 25th %ile 75th %ile 90th %ile
Use of high-risk medication*Potentially harmful
drug–disease interactions**
* Medicare beneficiary received at least one drug from a list of 13 classes of high-risk prescriptions that should be avoided by the elderly. ** Medicare beneficiaries with dementia, hip or pelvic fracture, or chronic renal failure, and received a prescription in an ambulatory care setting that is contraindicated for the condition. Data: Y. Zhang analysis of 5% sample of Medicare beneficiaries enrolled in stand-alone Medicare Part D plans (Zhang et al., 2010).
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011.

17
20
1618
2224
1618
22 222020
0
10
20
30
2003 2005 2009 10th 25th 75th 90th 10th 25th 75th 90th
Medicare Hospital 30-Day Readmission Rates Remain High
Hospital Referral Region percentiles, 2009
State percentiles, 2009
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011.
Percent of Medicare beneficiaries initially admitted for one of 45 medical conditions or surgical procedures who are readmitted within 30 days following discharge*
* See Appendix B for list of conditions and procedures used in the analysis.Data: G. Anderson and R. Herbert, Johns Hopkins University analysis of Medicare Standard Analytical Files (SAF) 5% Inpatient Data.
U.S. average

18
Potentially Preventable Hospital Admissions for Select Ambulatory Care Sensitive Conditions
156
49
230
49
209
135
U.S.average
Top 10%states
Bottom 10%states
202
104
251205
108
251
U.S.average
Top 10%states
Bottom 10%states
2004 2007
Adjusted rate per 100,000 population*
476
246
634
545
211
416
0
100
200
300
400
500
600
700
U.S.average
Top 10%states
Bottom10% states
Diabetes**Heart failure Pediatric asthma
* Rates are adjusted by age and gender using the total U.S. population for 2000 as the standard population.** Combines three diabetes admission measures: uncontrolled diabetes without complications, diabetes with short-term complications, and diabetes with long-term complications. Data: U.S. average—Healthcare Cost and Utilization Project, Nationwide Inpatient Sample; State distribution—State Inpatient Databases; not all states participate in HCUP (AHRQ 2010).
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011. 18

19
Nursing Homes: Hospital Admission and Readmission Rates Among Nursing Home Residents, by Hospital Referral Regions
18
13
24
20
15
25
21
16
26
Median 10th %ile 90th %ile
2000 2004 2008
18
11
26
20
12
28
20
12
28
0
20
40
Median 10th %ile 90th %ile
2000 2004 2008
Data: V. Mor and Z. Feng, Brown University analysis of Medicare enrollment data and Part A claims data for all Medicare beneficiaries who entered a nursing home and had a Minimum Data Set assessment.
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011.
Percent of long-stay nursing home residents hospitalized over a six-month period
Percent of first-time nursing home residents rehospitalized within 30 days of hospital discharge to nursing home

20
Use of Electronic Medical Records
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011.
17
28
46
97 97 96 95 94 94
7268
37
99
0
25
50
75
100
2000 2006 2009 NETH NZ NOR UK AUS ITA SWE GER FRA CAN
International Comparison, 2009
Percent of primary care physicians using electronic medical records
United States
AUS=Australia; CAN=Canada; FRA=France; GER=Germany; ITA=Italy; NETH=Netherlands; NZ=New Zealand; NOR=Norway; SWE=Sweden; UK=United Kingdom.Data: Commonwealth Fund International Health Policy Survey of Physicians.

21
International Comparison of Spending on Insurance Administration, 2009
a 2008* Includes claims administration, underwriting, marketing, profits, and other administrative costs; based on premiums minus claims expenses for private insurance. NHE=National Health ExpendituresData: OECD Health Data 2011 (database), Version 06/2011.
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011. 21
Percent of NHE Per capita ($US PPP)
Japana 1.9% $53.6
Finland 2.1% $63.2
Australiaa 3.6% $118.3
Austria 3.6% $146.8
Canada 3.7% $153.3
Netherlands 4.0% $185.1
Switzerland 4.9% $253.2
Germany 5.4% $221.8
France 7.0% $270.8
United States* 7.0% $531.5

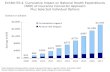
22Potential to Improve: National AnnualGains if Reach Benchmark Performance
• Up to 91,000 fewer deaths before age 75 from causes potentially preventable with timely and appropriate health care if the U.S. achieved best country rate; 84,000 if achieved lowest 3 countries
• 66 million more adults would receive recommended screenings and preventive care at appropriate ages according to guidelines
• 38 million more adults ages 19–64 would have an accessible primary care provider
• $55 billion in saving in insurance administrative costs if the U.S. achieved levels of other countries with competing private insurance plans– $114 billion if U.S. achieved levels of lowest rate countries– Does not include potential savings to physicians and hospitals
from reduced complexity

23
Data: U.S. Census Bureau, 2010–11 Current Population Survey ASEC Supplement; estimates for 2019 by Jonathan Gruber and Ian Perry of MIT using the Gruber Microsimulation Model for The Commonwealth Fund.
Post-Reform: Projected Percent of Adults Ages 19–64 Uninsured by State
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011. 23
2009–2010median = 19.4%
2019 (estimated)median = 8.4%
19%–22.9%
14%–18.9%
23% or more
8%–13.9%
Less than 8%
23
WA
OR
ID
MT ND
WY
NV
CAUT
AZNM
KS
NE
MN
MO
WI
TX
IA
IL IN
AR
LA
AL
SC
TNNC
KY
FL
OH
MI
WV
PA
NY
AK
MEVTNH
MA
RI
DE
DC
HI
CO
GAMS
OK
NJ
SD
VA
CT
MD
WA
OR
ID
MT ND
WY
NV
CAUT
AZNM
KS
NE
MN
MO
WI
TX
IA
IL IN
AR
LA
AL
SC
TNNC
KY
FL
OH
MI
WV
PA
NY
AK
MEVTNH
MA
RI
DE
DC
HI
CO
GAMS
OK
NJ
SD
VA
CT
MD

24Summary and Implications
• Access is an essential foundation for improvement– U.S. losing ground in ensuring access to affordable health care– Access to care, health care quality, and efficiency are interrelated
• What receives attention gets improved– Focused quality improvement and public reporting initiatives have led to
significant gains– Measurable and actionable benchmarks provide targets to improve– Gaps between average performance and benchmarks remain large,
underscoring potential gains• Better primary care and care coordination needed to improve outcomes at lower
costs– Strengthen primary care system to ensure access, ongoing care management,
and care coordination– Improve transitions and follow-up care after hospitalization needed
• Align incentives to promote more effective and efficient use of staff, IT, and clinical resources

25
Affordable Care Act Reforms on Target
• Insurance reforms will provide foundation for affordable, comprehensive insurance
• Payment and care system reforms targeted on gaps, wide variations across the United States
• Investment in information systems to guide and inform action
• Emphasis on primary care and coordination, with patient-centered care teams
• Accountability for health, care, and cost outcomes
• Should expect to see positive scorecard results in the future

26
For More Information Visit the Fund’s website atwww.commonwealthfund.org
Why Not the Best provides comparative data for hospitals. To access: www.whynotthebest.org
Related Documents