Pediatric Skin Disorders

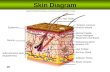
Pediatric Skin Disorders. Compare skin differences Infant: skin not mature at birth Adolescence: sebaceous glands become enlarged & active.
Dec 26, 2015
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

Pediatric Skin Disorders

Compare skin differences
Infant: skin not mature at birth Adolescence: sebaceous glands become
enlarged & active.

Skin Assessment
Assess history Assess exposure Assess character Assess sensation

Dermatitis

Dermatitis
Inflammation of the skin that occurs in response to contact with an allergen or irritant; also referred to as “contact dermatitis”

Dermatitis
Common irritants:
Soap, fabric softeners, lotions, urine and stool
♦ Common allergens
poison ivy, poison oak
lanolin, latex, rubber
nickel, fragrances

Dermatitis: signs and symptoms
Erythema Edema Pruritus Vesicles or bullae
that rupture, ooze and crust

Dermatitis: Treatment
Medications– Application of a corticosteroid topical agent:
remind pt to continue use for 2-3 wks after signs of healing
– Application of protective barrier ointments
Oatmeal baths, cool compresses
Antihistamines given for sedative effect

Eczema
Chronic superficial skin disorder characterized by intense pruritis

Eczema: signs and symptoms
Erythematous patches with vesicles Pruritis Exudate and crusts Drying and scaling Lichenification
(thickening of the skin)

Eczema, cont.

Goal of Treatment
Hydrate the skin

Treatment of Eczema
Emollients (creams which lubricate the skin)
Oral antihistamines (control itching) Antibiotics (treat superinfections) Corticosteroids (anti-inflammatories) Immunomodulators (inhibit T lymphocyte
activation) AVOID SOAPS!

Acne

Acne
Inflammatory disease of the skin involving the sebaceous glands and hair follicles.
Contributing factors include: heredity, hormonal influences and emotional stress

Acne: Three main types
Follicular plugs Pustular papules Cystic nodules

Patient teaching
Do not pick! This increases the bacterial count on the surface of the skin and opens lesions to infection which worsens scarring
Remind patients that the treatment will not show improvement until about 4-6 weeks but they must consistently follow the regime set up by the physician

Medical treatment for acne
Topical (Benzoyl peroxide, Tretinoin (RetinA), topical preferred to systemic; however, both may be needed
Oral: Tetracycline, minocycline, erythromycin; estrogen for female pts., Accutane

Acne: Nursing care
Avoid picking and squeezing Use gentle skin cleansers Avoid use of astringents containing ETOH Avoid hats or abrasive rubbing of the skin Wash hands after handling greasy foods Limit use of petrolatum-based hair products; hair
away from face Use oil-free makeup, protections from windy,
cold weather Continue therapy even when improved

Impetigo
http://www.emedicine.com/emerg/topic283.htm
Impetigo became infected
Hemolytic Strep infection of the skin Incubation period is 2-5 days after contact

Begins as a reddish macular rash, commonly seen on face/extremities
Progresses to papular and vesicular rash that oozes and forms a moist, honey colored crust. Pruritis of skin
Common in 2-5 year age group

Therapeutic Management
Apply moist soaks of Burrow’s solution Apply moist soaks of Burrow’s solution Antibiotic therapy: Keflex for 10 days Patient education

Therapeutic Interventions for impetigo
Goal: prevent scarring and promote + self image.
Individualize treatment to gender, age, and severity of infection
Takes 4-6 wks to improve What is the major nursing implication
here?

Candiditis- Thrush
Overgrowth of Candida albicans
Acquired through delivery

Thrush
Characterized by white patches in the mouth, gums, or tongue
Treated with oral Nystatin suspension: swish and swallow

Dermatophytosis (Ringworm)
Tinea Capitis fungal
infection known as
“ringworm”
Transmission: – Person-to-person – Animal-to-person

S&S:
Scaly, circumscribed patches to patchy, gray scaling areas of alopecia.
Pruritic Generally asymptomatic, but severe, deep
inflammatory reaction may appear as boggy, encrusted lesions (kerions)

http://www.ecureme.com/quicksearch_reference.asp

Clinical manifestations
Fungal infection of the stratum corneum, nails and hair (the base of hair shaft causing hair to break off…rarely permanent)
Scaly, patches Pruritis Generally asymptomatic, but severe
reactions may appear as encrusted lesions

Tinea: signs and symptoms

Therapeutic Interventions
Transmitted by clothing, bedding, combs and animals (cats especially)
May take 1-3 months to heal completely, even with treatment
Child doesn’t return to school until lesions dry

Diagnosis
Potassium hydroxide examination
Black Light

Medication Therapy
Antifungals:– Oral griseofulvin (Lamisil)
• Give with fatty foods to aid in absorption
• Treatment is 4-6 wks
• Can return to daycare when lesions are dry

Pediculosis Capitis (lice)
http://www.emedicine.com/emerg/topic409.htm
a parasitic skin disorder caused by lice the lice lay eggs which look like white
flecks, attached firmly to base of the hair shaft, causing intense pruritus

Diagnosis
Direct identification of egg (nits)
Direct identification of live insects

Pediculosis

Medication Therapy
Treatment: shampoos RID, NIX, Kwell(or Lindane) shampoo: is applied to wet hair to form a lather and rubbed in for at least amount of time recommended, followed by combing with a fine-tooth comb to remove any remaining nits.

Scabies
http://www.nlm.nih.gov/medlineplus/scabies.htmlSarcoptes scabei mite. Females are 0.3 to 0.4 mm long and 0.25 to 0.35 mm wide.
Males are slightly more than half that size.
A parasitic skin disorder (stratum corneum- not living tissue) caused by a female mite.
The mite burrows into the skin depositing eggs and fecal material; between fingers, toes, palms, axillae
pruritic & grayish-brown, thread-like lesion

http://www.aad.org/pamphlets_spanish/sarna.html
Scabies between thumb and index finger
On foot

Therapeutic Interventions
transmitted by clothing, towels, close contact Diagnosis confirmed by demonstration from skin
scrapings. treatment: application of scabicide cream which
is left on for a specific number of hours (4 to 14)to kill mite
rash and itch will continue until stratum corneum is replaced (2-3 weeks)

Care:
Fresh laundered linen and underclothing should be used.
Contacts should be reduced until treatment is completed.

Related Documents