Inflammation-Induced Airway Hypersensitivity: From Ion Channels to Patients Lu-Yuan Lee, Ph.D. Airway Sensory Neurobiology Laboratory Department of Physiology University of Kentucky Medical Center BACKGROUND AND HYPOTHESES My research interest focuses on the neurogenic mechanisms involved in the bronchial hyperreactivity, and ongoing projects are currently conducted in the Airway Sensory Neurobiology Laboratory at the University of Kentucky to study this in animal models and in human subjects. Airway hypersensitivity is a characteristic feature of airway inflammatory diseases such as asthma. When airway hypersensitivity develops during airway mucosal inflammation, the excitability of chemosensitive nerve endings innervating the airways is drastically enhanced. In healthy lungs, these tachykinin-containing sensory terminals located superficially in the airway mucosa (Fig. 1) play an important role in protecting the airways against inhaled irritants. Stimulation of these sensory endings elicits extensive cardiopulmonary reflex responses such as cough, bronchospasm, hypersecretion of mucus, etc. However, when these nerve endings become hypersensitive as a result of inflammation or injury of airway mucosa, a given level of stimulus will then evoke more sustained and intense stimulation. Thus, greater intensities of the reflex reactions as well as the neurogenic inflammation mediated through local release of tachykinins can lead to the development of bronchial hyperreactivity. Function of TRPV1-expressing sensory nerves and their interaction with other cell types in airway mucosa. EO, eosinophil; LO, lipooxygenase; PGE 2 , prostaglandin E 2 ; BK, bradykinin; NGF, nerve growth factor; MBP, eosinophil major basic proteins; TKs, tachykinins; CGRP, calcitonin gene-related peptide. (From: Lee & Gu, 2009)

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

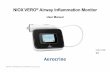
Inflammation-Induced Airway Hypersensitivity: From Ion Channels to Patients
Lu-Yuan Lee, Ph.D. Airway Sensory Neurobiology Laboratory
Department of Physiology University of Kentucky Medical Center
BACKGROUND AND HYPOTHESES My research interest focuses on the neurogenic mechanisms involved in the bronchial hyperreactivity, and ongoing projects are currently conducted in the Airway Sensory Neurobiology Laboratory at the University of Kentucky to study this in animal models and in human subjects. Airway hypersensitivity is a characteristic feature of airway inflammatory diseases such as asthma. When airway hypersensitivity develops during airway mucosal inflammation, the excitability of chemosensitive nerve endings innervating the airways is drastically enhanced.
In healthy lungs, these tachykinin-containing sensory terminals located superficially in the airway mucosa (Fig. 1) play an important role in protecting the airways against inhaled irritants. Stimulation of these sensory endings elicits extensive cardiopulmonary reflex responses such as cough, bronchospasm, hypersecretion of mucus, etc. However, when these nerve endings become hypersensitive as a result of inflammation or injury of airway mucosa, a given level of stimulus will then evoke more sustained and intense stimulation. Thus, greater intensities of the reflex reactions as well as the neurogenic inflammation mediated through local release of tachykinins can lead to the development of bronchial hyperreactivity. Function of TRPV1-expressing sensory nerves and their interaction with
other cell types in airway mucosa. EO, eosinophil; LO, lipooxygenase; PGE2, prostaglandin E2; BK, bradykinin; NGF, nerve growth factor; MBP, eosinophil major basic proteins; TKs, tachykinins; CGRP, calcitonin gene-related peptide. (From: Lee & Gu, 2009)

LONG-TERM OBJECTIVES
Our long-term objectives are to answer the following questions: • What are the physiological and pharmacological properties of the chemosensitive nerve endings in the lung? • What are the roles of these sensory nerves in regulating cardiopulmonary functions under normal and various pathophysiological conditions of the airways? • What are the endogenous and exogenous chemical substances that can alter the sensitivity of these sensory endings? • What are the cellular mechanisms underlying the hypersensitivity of these sensory nerves caused by inflammation of airway mucosa, such as during airway injury or allergic reaction? • What is the role of the transient receptor potential vanilloid type 1 (TRPV) ion channels in the airway hypersensitivity (exaggerated cough and bronchoconstrictive responses to inhaled irritants) developed during airway inflammatory reaction?
ONGOING PROJECTS
Several projects are currently conducted in our lab aimed specifically to: • Uncover the mechanism of hypersensitivity of bronchopulmonary C neurons caused by cationic proteins, that are released from inflammatory cells (e.g., eosinophil, neutrophil, etc.) during airway anaphylaxis or injury. • Identify the specific ion channels and the intracellular signal transduction pathways involved in the hypersensitivity of pulmonary sensory neurons induced by certain endogenous chemical mediators (e.g., prostaglandin E2, adenosine, hydrogen ions, etc.) and pro-inflammatory cytokines (e.g., tumor necrosis factor-α) • Determine the temperature-sensitive properties of bronchopulmonary C neurons, and investigate their roles in regulating the cardiopulmonary functions in responses to an acute increase in airway temperature (e.g., during airway inflammation, exercise, etc.) • Understand the underlying mechanisms of airway hypersensitivity in patients with mild asthma, allergic rhinitis, laryngopharyngeal reflux, and post-viral infection • Investigate the possible involvement of the TRPV1 channel in the manifestation of bronchoconstriction, cough and dyspneic sensation in these patients.
REPRESENTATIVE RECENT STUDIES Sensitization of Vagal Pulmonary Sensory Neurons by Human Eosinophil-Derived Cationic Proteins
Rationale and Hypothesis: During airway inflammatory reaction (e.g., in asthma), a number of low molecular weight, highly cationic proteins, such as major basic protein (MBP) and eosinophil cationic protein, are secreted by eosinophils that infiltrate into the airways. It is well documented that the release of these proteins can induce mucosal injury and airway hyperresponsiveness. However, the mechanism underlying both the initial stimulatory and the sustained sensitizing effects of cationic proteins on pulmonary sensory nerves is poorly understood.

Fig. 1. MBP potentiates the capsaicin-evoked whole-cell inward current in isolated rat vagal pulmonary sensory neurons.
Fig. 2. MBP enhances the action potential firing in response to electrical stimulation in rat vagal pulmonary sensory neurons.
Fig. 3. MBP inhibits both sustained delayed-rectifier voltage-gated K+ current (IKdr) and A-type, fast-inactivating K+ current (IKa) in rat vagal pulmonary sensory neurons.
Fig. 1 Fig. 3
Fig. 2
Summary of Results: Our studies have established the first evidence demonstrating an intense and sustained effect of eosinophil granule-derived proteins on vagal bronchopulmonary C-fiber endings, which is dependent on their cationic charge. Our results also demonstrate that MBP potentiates the capsaicin-evoked inward current in isolated pulmonary sensory neurons and up-regulates the excitability of these neurons to electrical stimulation. Our data further demonstrate that MBP significantly inhibits both IKdr and IKa in these neurons. Our studies therefore suggest that the direct and long-lasting sensitizing effect of these cationic proteins on pulmonary sensory nerves may play an important part in the manifestation of airway hyperresponsiveness associated with eosinophil infiltration in the airways.
Hypersensitivity of TRPV1 Induced by Activation of Protease-activated Receptor-2
Rationale and Hypothesis: Protease-activated Receptor-2 (PAR2) belongs to a family of G-protein-coupled, seven-transmembrane-domain receptors named PARs that are uniquely activated by proteolysis. Compelling evidence indicates that PAR2 plays a critical role in the pathogenesis of airway inflammation and airway hyperresponsiveness. The primary objective of this study is to uncover the mechanism involved in the interaction between PAR2 and C-fiber sensory nerves in the lung/airways.

Fig. 4. Activation of PAR2 potentiates the capsaicin-evoked whole-cell inward current in isolated rat vagal pulmonary sensory neurons.
Fig. 5. PAR2-AP potentiates single-channel activity of TRPV1 in cell-attached patches from rat pulmonary sensory neurons.
Fig. 4 Fig. 5
Summary of Results: In anesthetized spontaneously breathing rats, airway exposure to trypsin, an endogenous agonist of PAR2, significantly amplifies the capsaicin-induced pulmonary chemoreflex responses. In isolated rat vagal pulmonary sensory neurons, pretreatment with trypsin potentiated the capsaicin-induced whole-cell inward current; the effect is mimicked by PAR2-activating peptide (PAR2-AP) in a concentration-dependent manner. Activation of PAR2 up-regulates single-channel activities of TRPV1 and the effect is mediated through the protein kinase C-dependent transduction pathway.
An increase in capsaicin sensitivity and TRPV1 expression of pulmonary myelinated afferents in ovalbumin-sensitized rats
Rationale and Hypothesis: Increasing evidence indicates that the TRPV1 receptor selectively expressed in vagal bronchopulmonary C-fibers plays a pivotal role in the manifestation of airway hypersensitivity, a prominent pathophysiological feature of airway inflammatory diseases. This study was carried out to investigate whether the sensitivity vagal afferents and expression of TRPV1 in these nerves are altered when chronic airway inflammation is induced by ovalbumin (Ova) sensitization in an animal model of asthma.
Fig. 6. Effect of Ova sensitization on TRPV1 expression in NF-positive and NF-negative neurons with DiI-labelling in nodose ganglion. Arrows, co-localization of NF staining, DiI labelling and TRPV1 staining in the same neurons. Asterisks, co-localization of NF staining and DiI labeling, but without TRPV1 staining. Scale bar, 50 μm.
Fig. 6

Hyperthermia Increases Sensitivity of Pulmonary C-fiber Neurons: Role of TRPV channels
Rationale and Hypothesis: When body temperature increases during strenuous exercise or fever, the lung tissues including the sensory endings residing within the lung structures are subjected to hyperthermia. The TRPV channels expressed in the sensory terminals of bronchopulmonary C fibers are known to function as thermal transducers, with a different activation temperature threshold in each subtype of the TRPV channels. This study was, therefore, carried out to answer the following specific questions: 1) Are vagal pulmonary C-fibers sensitive to an increase in the temperature within the normal physiological range, and if so, can hyperthermia also directly activate isolated vagal pulmonary sensory neurons? 2) Is the response of these neurons to increase in temperature mediated through activation of TRPV channels?
Summary of Results: This study showed that allergen sensitization markedly elevates the baseline activity and excitability of pulmonary C-fibers. Interestingly, vagal bronchopulmonary myelinated afferents also exhibited capsaicin sensitivity in sensitized rats. Furthermore, the immunohistochemistry experiments showed that there was a significant increase in the proportion of TRPV1-expressing pulmonary neurons in nodose ganglia of sensitized rats, particularly in neurofilament-positive (myelinated) neurons.
Fig. 8
Fig. 8. Blocking effects of capsazepine (CPZ, 10 µM) and ruthenium red (RR, 3 µM) on the hyperthermia-induced current in rat vagal pulmonary sensory neurons. C: group data (n=11) showing the effects of different treatments on cell response to hyperthermia.
Fig. 7. Effect of increasing temperature on vagal pulmonary sensory neurons in voltage-clamp (A) and current-clamp mode (B). C: the temperature-current relationships obtained from the two hyperthermia challenges in the same neuron (data taken from A).
Fig. 7

Hyperthermia-induced bronchoconstriction and cough in patients with mild asthma: a translational study
Rationale and Hypothesis: Our recent studies have demonstrated that an activation of TRPV1 is primarily responsible for the stimulatory effect of hyperthermia on vagal bronchopulmonary C-fibers. We reasoned that a stimulation of these afferents will elicit bronchoconstriction via cholinergic reflex mechanism. Further, we hypothesized that the temperature threshold for activating these afferents will be reduced in patients with mild asthma. Hence, breathing warm, humid air can activate TRPV1 and elicit reflex bronchoconstriction and other airway dysfunction (e.g., cough, dyspnea, etc.).
Summary of Results: Isolated vagal pulmonary sensory neurons can be activated by an increase in temperature within the physiological range, and the thermal sensitivity of these neurons is mediated primarily through the activation of TRPV1. Increasing temperature also exerts a pronounced potentiating effect on the responses to TRPV1 activators in these neurons. This sensitizing effect results from a positive interaction between hyperthermia and these chemical activators at the TRPV1 channel.
Fig. 9
Fig. 9. Effect of increasing temperature on the response of vagal pulmonary sensory neurons to capsaicin (Cap). Vm, membrane potential; BT, body temperature; HT, hyperthermic temperature; ∆I, inward current evoked by Cap.

Summary of Results: This pilot study showed that breathing warm humidified air triggered cough and acute bronchoconstriction in mild asthmatic patients; the latter could be prevented by a pretreatment with ipratropium (atropine). These preliminary results indicated the involvement of airway sensory nerves and cholinergic mechanisms in the manifestation of various symptoms evoked by airway hyperthermia in these patients, which further suggests the potential involvement of TRPV1 over-expression in asthmatic airways as a possible contributing factor.
Fig.12
Fig. 10. Effect of pretreatment with ipratropium aerosol or placebo on the response of airway resistance to warm humid air inhalation challenge air in six asthmatic patients.
Fig. 11. Bronchomotor and cough responses were measured in asthmatic patients (UK Pulmonary Function Testing Laboratory and Clinical Research Development & Operations Center)
Fig. 12. Experimental records illustrating a comparison of the flow-volume curves between baseline (blue) and that after termination of hyperventilation with humidified air (red) at room (RA; panel A) or high temperature (HA; panels B,C & D) on four different days in a patient with mild asthma.
Fig.11 Fig.10

REPRESENTATIVE RECENT PUBLICATIONS (2008-2013):
Burki, N.K., M. Sheatt, and L.-Y. Lee. Effects of airway anesthesia on dyspnea and ventilatory response to intravenous injection of adenosine in healthy human
subjects. Pulm Pharmacol Ther. 21: 208-13, 2008.
Gu, Q., M.E. Wiggers, G.I. Gleich, and L.-Y. Lee. Sensitization of isolated rat vagal pulmonary sensory neurons by human eosinophil granule-derived cationic
proteins. Am. J. Physiol.: Lung Cell. Mol. Physiol. 294: L544-52, 2008.
Ni, D., and L.-Y. Lee. Effect of hyperthermia on excitability of isolated rat vagal pulmonary sensory neurons: role of TRPV1 receptor. Am. J. Physiol.: Lung Cell.
Mol. Physiol. 294: L563-71, 2008.
Zhang, G. ,R.-L. Lin, M. Wiggers, D.M. Snow, and L.-Y. Lee. Altered expression of TRPV1 and sensitivity to capsaicin in pulmonary myelinated afferents following
chronic airway inflammation in the rat. J. Physiol. (Lond) 586:5771-86, 2008.
Lee, L.-Y. Respiratory Sensations Evoked by Activation of Bronchopulmonary C-fibers. In: Dyspnea (Special Issue), ed. by D.E. O’Connell and J.T. Fisher. Respir.
Physiol. Neurobiol. 167: 26-35, 2009 (Invited review).
Lin, R.-L., D. Hayes, and L.-Y. Lee, Bronchoconstriction induced by hyperventilation with humidified hot air: role of TRPV1-expressing airway afferents. J. Apply.
Physiol. 106:1917-24, 2009.
Lee, L.-Y., and Q. Gu. Nicotine membrane receptors on cough sensors. In: Pharmacology and Therapeutics of Cough, ed by K.F. Chung and J.G. Widdicombe.
Handbook of Experimental Pharmacology 187: 77-98, 2009 (Invited review).
Lee, L.-Y., and Q. Gu. Role of TRPV1 receptor in inflammation-induced airway hypersensitivity. Current Opinion in Pharmacol. 9: 243-49, 2009 (Invited review).
Hu, Y, Q. Gu, R.-L. Lin, R. Kryscio, and L.-Y. Lee. Calcium transient evoked by TRPV1 activators is enhanced by tumor necrosis factor alpha in rat pulmonary
sensory neurons. Am. J. Physiol. Lung Cell. Mol. Physiol. 299: L483-92, 2010.
Gu, Q., and L.-Y. Lee. Regulation of acid signaling in rat pulmonary sensory neurons by protease-activated receptor-2. Am. J. Physiol. Lung Cell. Mol. Physiol.
298: L454-61, 2010.
Burki, N.K., and L.-Y. Lee. Mechanisms of dyspnea. Chest 138: 1196-1201, 2010 (Invited review).
Lee, L.-Y., D. Ni, D. Hayes, and R.-L. Lin. TRPV1 as a cough sensor and its temperature-sensitive properties. Pulm. Pharmacol. Therap. 24: 280-5, 2011 (Invited
review).
Gu, Q. and L.-Y. Lee. Airway irritation and cough evoked by acid: from human to ion channel. Current Opinion in Pharmacol. 11: 238-47, 2011 (Invited review).
Hayes, D., P.B. Collins, M. Khosravi, and L.-Y. Lee. Bronchoconstriction triggered by breathing hot humid air in asthmatics: role of TRPV1 receptor. Am. J. Resp.
Crit Care Med. 185: 1190-6, 2012.
Hsu, C.C., Y.S. Lin, R.-L. Lin and L.-Y. Lee. Bronchoconstriction induced by increasing airway temperature in ovalbumin-sensitized rats: role of tachykinins. J. Appl.
Physiol. 115: 688-96 , 2013.
Hsu, C.C., R.-L. Lin, L.-Y. Lee and Y.S. Lin. Hydrogen sulfide induces hypersensitivity of rat lung vagal neurons: role of TRPA1 receptors. Am. J. Physiol. : Reg. Int.
Comp. Physiol. 305: R769-79, 2013.
Lin, R.-L., Y.J. Lin, M.J. Geer, R. Kryscio and L.-Y. Lee. Pulmonary chemoreflex responses are potentiated by tumor necrosis factor-alpha in mice. J Appl Physiol.
114: 1536-43, 2013.
Lee, L.-Y., Q. Gu, F. Xu, J.L. Hong. Acid-sensing by airway afferent nerves. Pulm Pharmacol Ther. 26: 491-7, 2013.
Lee, L.-Y., J. Yu. Sensory nerves in lung and airways. Comprehensive Physiology (American Physiological Society). 4: 287-324, 2014 (Invited review). doi:
10.1002/cphy.

Airway Sensory Neurobiology Laboratory
Lu-Yuan Lee
You-Shuei (Emy) Lin
Related Documents