226 PEDIATRIC NURSING/September-October 2014/Vol. 40/No. 5 C onsider this scenario com- mon five years ago: Nathan, a second grade student, was sent to the school nurse’s office for a “head check” after his teacher noticed him frequently scrat- ching his head. The nurse finds sever- al tiny white objects on Nathan’s hair, about an inch from the scalp. The nurse does not see any evidence of nits closer to the head, nor does she find any live lice. Per school policy, the nurse immediately calls his par- ents and requests they come to pick him up. His belongings are brought to the nurse’s office. When his parents arrive, the nurse explains there is evi- dence that Nathan might have lice, and that he needs to be treated. She also explains the “no-nit” policy, meaning all nits must be removed from his hair before he returns to school. The nurse describes a treat- ment program that includes washing all the linen in the house, washing all of Nathan’s clothing, putting all items that cannot be washed, such as stuffed animals, in a plastic bag for 10 days, and spraying an aerosol pedi- culicide or vacuuming all hard and soft household surfaces. The nurse also recommends the student and all members of the family be treated with a pediculicide. As an alternative, the nurse suggests a regime that includes either a mayonnaise treatment or a commercial lice removal service. The nurse proceeds to check the heads of all the students in Nathan’s classroom and sends a letter home to notify the parents of Nathan’s classmates of a case of lice in the classroom. Nathan’s Continuing Nursing Education The treatment of Pediculosis capitis, or head lice, is fraught with misinformation, myths, and mismanagement. Common myths include the need to exclude children from school, the need to remove all visible nits (“no-nit” policies), the need for mas- sive environmental cleaning, that head lice live for long periods of time, and that schools are a common location for lice transmission. Head lice are a common childhood nuisance, causing embarrassment and emotional trauma in both chil- dren and families. This article explores and challenges the commonly held beliefs about the identification, management, and treatment of Pediculosis by presenting current recommended evidence-based practice. It also challenges pediatric nurs- es, and school nurses in particular, in alignment with the National Association of School Nurses (NASN) Position Statement on Pediculosis Management in the School Setting, to act as change agents for reasonable and effective school poli- cies and practices. Demystifying Pediculosis: School Nurses Taking the Lead Deborah J. Pontius Objectives and instructions for completing the evaluation and statements of disclosure can be found on page 235. Deborah J. Pontius, MSN, RN, NCSN, is Health Services Coordinator, Pershing County School District, Lovelock, NV, and Past Board Member and Executive Com- mittee Member, National Association of School Nurses, Silver Spring, MD. teacher asks the nurse to check her head and to sanitize headphones in her classroom. The problem with the scenario described above is that not one of the health care provider interventions is evidence-based best practice. Many school nurses across the county have successfully advocated their school boards to update their treatment of Pediculosis to reflect the current state of knowledge. Unfortunately, the sce- nario above is still all too common. This article will evaluate common head lice myths or traditional prac- tices and present current evidence- based Pediculosis practice. For the school community, Pedi- culosis capitis, or head lice, is a time consuming, seemingly never-ending problem. School children (presumed to be) with lice have been estimated to lose an average of four days of school per year in schools where “no-nit” policies are enforced (Gordon, 2009). This represents not only a loss of the opportunity for learning, but a loss of funding for schools and loss of parent work days as well. Nationwide, it has been estimated that schools lose between $280 to $325 million in annual funding, and families lose up to of $2,720 in wages per active infes- tation (Gordon, 2009). Myth #1. Lice Are Easy To Get; They Are Easily Passed via Hats, Helmets, Or Hair Care Items; And Can Jump or Fly From One Person to Another A head louse is a wingless insect with six legs; therefore, it cannot jump, fly, or even crawl long distances (Centers for Disease Control and Preventions [CDC], 2013a). Lice pos- sess pincher-like grasping structures that allow them to hold on to the hair shaft quite tenaciously. Bathing, shampooing, or simple daily hair brushing cannot easily dislodge them (see Figure 1). The pincher actually adapts to hair shafts. In the U.S., the most common form of head lice species has adapted to the round Caucasian hair shaft (Frankowski & Bocchini, 2010). Lice are much less common among the oval-shaped hair shaft of the African-American child. A louse is mostly readily transmitted via head-to-head contact. There is a very small theoretical possibility that hair care items may assist in the transmission of lice, although these insects are likely to be dead or injured. Therefore, it is pru-

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

226 PEDIATRIC NURSING/September-October 2014/Vol. 40/No. 5
Consider this scenario com-mon five years ago: Nathan, asecond grade student, wassent to the school nurse’s
office for a “head check” after histeacher noticed him frequently scrat -ching his head. The nurse finds sever-al tiny white objects on Nathan’s hair,about an inch from the scalp. Thenurse does not see any evidence ofnits closer to the head, nor does shefind any live lice. Per school policy,the nurse immediately calls his par-ents and requests they come to pickhim up. His belongings are brought tothe nurse’s office. When his parentsarrive, the nurse explains there is evi-dence that Nathan might have lice,and that he needs to be treated. Shealso explains the “no-nit” policy,meaning all nits must be removedfrom his hair before he returns toschool. The nurse describes a treat-ment program that includes washingall the linen in the house, washing allof Nathan’s clothing, putting all itemsthat cannot be washed, such asstuffed animals, in a plastic bag for 10days, and spraying an aerosol pedi-culicide or vacuuming all hard andsoft household surfaces. The nursealso recommends the student and allmembers of the family be treated witha pediculicide. As an alternative, thenurse suggests a regime that includeseither a mayonnaise treatment or acommercial lice removal service. Thenurse proceeds to check the heads ofall the students in Nathan’s classroomand sends a letter home to notify theparents of Nathan’s classmates of acase of lice in the classroom. Nathan’s
Continuing Nursing Education
The treatment of Pediculosis capitis, or head lice, is fraught with misinformation,myths, and mismanagement. Common myths include the need to exclude childrenfrom school, the need to remove all visible nits (“no-nit” policies), the need for mas-sive environmental cleaning, that head lice live for long periods of time, and thatschools are a common location for lice transmission. Head lice are a commonchildhood nuisance, causing embarrassment and emotional trauma in both chil-dren and families. This article explores and challenges the commonly held beliefsabout the identification, management, and treatment of Pediculosis by presentingcurrent recommended evidence-based practice. It also challenges pediatric nurs-es, and school nurses in particular, in alignment with the National Association ofSchool Nurses (NASN) Position Statement on Pediculosis Management in theSchool Setting, to act as change agents for reasonable and effective school poli-cies and practices.
Demystifying Pediculosis: School Nurses Taking the Lead
Deborah J. Pontius
Objectives and instructions for completing the evaluation and statements of disclosure can be found on page 235.
Deborah J. Pontius, MSN, RN, NCSN, isHealth Services Coordinator, PershingCounty School District, Lovelock, NV, andPast Board Member and Executive Com -mittee Member, National Association ofSchool Nurses, Silver Spring, MD.
teacher asks the nurse to check herhead and to sanitize headphones inher classroom.
The problem with the scenariodescribed above is that not one of thehealth care provider interventions isevidence-based best practice. Manyschool nurses across the county havesuccessfully advocated their schoolboards to update their treatment ofPediculosis to reflect the current stateof knowledge. Unfortunately, the sce-nario above is still all too common.This article will evaluate commonhead lice myths or traditional prac-tices and present current evidence-based Pediculosis practice.
For the school community, Pedi -culosis capitis, or head lice, is a timeconsuming, seemingly never-endingproblem. School children (presumedto be) with lice have been estimated tolose an average of four days of schoolper year in schools where “no-nit”policies are enforced (Gordon, 2009).This represents not only a loss of theopportunity for learning, but a loss offunding for schools and loss of parentwork days as well. Nationwide, it hasbeen estimated that schools losebetween $280 to $325 million inannual funding, and families lose upto of $2,720 in wages per active infes-tation (Gordon, 2009).
Myth #1. Lice Are Easy To Get; They Are EasilyPassed via Hats, Helmets,Or Hair Care Items; And Can Jump or Fly From One Person toAnother
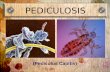
A head louse is a wingless insectwith six legs; therefore, it cannotjump, fly, or even crawl long distances(Centers for Disease Control andPreventions [CDC], 2013a). Lice pos-sess pincher-like grasping structuresthat allow them to hold on to the hairshaft quite tenaciously. Bathing,shampooing, or simple daily hairbrushing cannot easily dislodge them(see Figure 1). The pincher actuallyadapts to hair shafts. In the U.S., themost common form of head licespecies has adapted to the roundCaucasian hair shaft (Frankowski &Bocchini, 2010). Lice are much lesscommon among the oval-shaped hairshaft of the African-American child. Alouse is mostly readily transmitted viahead-to-head contact.
There is a very small theoreticalpossibility that hair care items mayassist in the transmission of lice,although these insects are likely to bedead or injured. Therefore, it is pru-

PEDIATRIC NURSING/September-October 2014/Vol. 40/No. 5 227
dent to recommend not sharing hair-brushes, combs, or hair retainers,such as “scruchies” or ponytail hold-ers. Slick helmets (e.g., bicycle hel-mets, football helmets, or baseballhats) pose no risk of transmission(Burgess, Pollack, & Taplin, 2003;CDC, 2013a; Frankowski & Bocchini,2010; Pontius, 2011). Although bedlinen may be a source of transmission,one study found live head lice ononly 4% of the pillow cases used byan infested person (Speare, Cahill, &Thomas, 2003). Sharing beds is notedto be a significant risk factor for trans-mission. The extended time withheads being close to each other whenbed sharing presents an opportunityfor adult lice to crawl from one headto another (Burgess et al., 2003;Frankowski & Bocchini, 2010;Meinking & Taplin, 2011).
Symptoms of lice include ticklingsensations, difficulty sleeping, soreson the head from scratching, anditching. Pruritus is caused by sensiti-zation to components of the louse’ssaliva. With a first case, itching maynot develop for three to six weeks, butwith repeated cases, the pruritusdevelops much more quickly(Frankowski & Bocchini, 2010).
Myth #2. You Can Get LiceFrom Your Dog, GuineaPig, or Other Animal
Human head lice (Pediculosishumanus capitis) are small parasiticinsects that live on the scalp and neckhairs of human hosts. Although thereare a number of other types of mam-malian lice, they are all species-specif-ic. Only humans can spread humanlice. Humans can only acquire humanlice (CDC, 2013a).
Myth #3. Head Lice BreedIn Furniture, Carpets andOther Household Objects;You Must Treat the HouseTo Eliminate Lice
People are infested with headlice, not things or places. A louse’sentire existence is dependent uponthe human host, and without thishost, lice typically die within 24hours (Meinking & Taplin, 2011).Eggs remain viable a bit longer, but assoon as hatched, they must feed onthe human host, or they will die with-in hours. According to RichardPollack, PhD, noted expert on para-
the world. In the U.S., children in pre-school and primary grades are affect-ed more often, as are their caregiversand housemates. This is due to theopportunity for close, head-to-headcontact (Burgess et al., 2003).
Myth #5. The Presence Of Nits/Eggs Indicates An Active Case of Lice
The three stages of the louse lifecycle are egg/nit, nymph, and adult,and altogether, the life cycle lastsapproximately 45 days (CDC, 2013a)(see Figure 2). The adult female louselays up to 8 to 10 brown to yellowishcolored eggs per day, which arecemented to the base of the hair shaft,most commonly found behind theears or at the nape of the neck (seeFigure 3). The color of the eggs mayvary to match the color of the hair,making them very difficult to discov-er (Frankowski & Bocchini, 2010;Meinking & Taplin, 2011). Because ofthe cement-like attachment, theycannot “fall” off. Nymphs hatch inabout one week, leaving behind awhite-colored shell or nit. The nymphstage is also about one week in length,going through three molts to achieveadulthood (see Figure 4). The adult isthe size of a sesame seed, is brown togray or whitish in color, and will livefor as many as 30 days (CDC, 2013a).Although some authorities refer tothe “nit” as the non-viable shell onlybecause it is difficult to ascertain trueviability of a nit without microscopicexamination, this article will use themore commonly ascribed definitionof nit to include both viable eggs andhatched egg shells.
The presence of a live louse isconsidered the gold standard for anactive infestation, not the mere pres-ence of nits (Pollack et al., 2000;Meinking & Taplin, 2011). A viablenit is one that is closer than six mil-limeters (mm) to the scalp (CDC,
sitology and entomology, “I’ve seennothing of an objective nature to sug-gest that fomites play any significantrole in the transmission of head lice”(Burgess et al., 2003, p. 4).
If a child is determined to have alice infestation, only items that havebeen in contact with the head of theperson with the lice in the previous24 to 48 hours prior to treatmentshould be considered for cleaning(Frankowski & Bocchini, 2010). Thismay include items of clothing wornnear the head and possibly carpetingor rugs if the child was lying on them.Washing, soaking, or drying items attemperatures greater than 130° F willkill stray lice or nits. Cloth or carpeteditems may be vacuumed. Althoughthe risk is low, it is prudent to notshare combs, brushes, or other haircare items. Pediculicide spray in thehome is not necessary and should notbe used. It provides unnecessaryexposure to pediculicides to bothinfested and uninfested persons inthe household, and can be can dan-gerous to infants (CDC, 2013a;Frankowski & Bocchini, 2010). TheAmerican Academy of Pediatrics(AAP) finds no benefit in “herculeancleaning measures” (Frankowski &Bocchini, 2010, p. 398).
Myth #4. Poor HygieneAnd Low Income AreAssociated with Head Lice
Head lice often infest people withgood hygiene and grooming habits(CDC, 2013a). There is some evidencethat more lice will be found on thehead that is shampooed or brushedless often (Frankowski & Bocchini,2010). However, regular hair hygienewill not eliminate nor prevent headlice, but may remove lice that areprobably dead or dying (Pollack,Kiszewski, & Spielman, 2000). Allsocioeconomic groups are affected,and infestations are seen throughout
Figure 1. Gripping “Claw” of the Head Louse
Source: CDC Public Health Image Library, 2014.

228 PEDIATRIC NURSING/September-October 2014/Vol. 40/No. 5
Demystifying Pediculosis: School Nurses Taking the Lead
2013a). Considering that nits do notmove after being laid, that nits hatchin approximately seven days, and thathair grows and average of 13 mm(Caucasian) to 10 mm (AfricanAmerican) per month (Loussouarn,Rawadi, & Genain, 2005), and gener-ously doubling the viability estimate(as it can be longer in warmer cli-mates (Meinking & Taplin, 2011),most experts concur that nits foundfarther than one-fourth to one-halfinches (6 to 12mm) from the scalp arenon-viable (Frankowski & Bocchini,2010; Mumcuoglu et al., 2007;National Association of School Nurses(NASN), 2011; Pollack et al., 2000).Lice are more common among girls,which may be due to longer hair hid-ing the infestation or a greater likeli-hood of playing with heads closertogether (Burgess et al., 2003;Frankowski & Bocchini, 2010). By thetime a case of lice is found, the childhas generally had them for a monthor more (Frankowski & Bocchini).
Myth #6. No-Nit PoliciesReduce the Transmission Of Head Lice in Schools
Over the past decade, there havebeen important recommended changesin the management of head lice inschools: No student should ever missschool time because of head lice, and no-nit policies should be eliminated (CDC,2013a; Frankowski & Bocchini, 2010;Mumcuoglu et al.,2007; NASN, 2011).Many schools have traditionally had“no-nit” policies, which re quire theremoval of all nits, viable or not,before a child returns to school. Toschool personnel unfamiliar with thelife cycle of the louse, school exclu-sion for an infestation or for the evi-
Figure 2.Lifecycle of the Louse
1st nymphEgg
Pediculus humanus capitis
= Infective Stage
= Diagnostic Stage
2nd nymph 3rd nymphAdults
Source: CDC, 2013c.
Figure 3.Viable Nit
Source: CDC Public Health Image Library, 2014.
Figure 4.Comparison of Egg, Nymph,
and Adult
Source: CDC Public Health ImageLibrary, 2014.

PEDIATRIC NURSING/September-October 2014/Vol. 40/No. 5 229
dence of nits seems logical. Theirrationale may be that by excludingthose who have head lice, others willnot catch it. However, there is no evi-dence that these policies reduce thetransmission of head lice in schools.Moreover, there is significant evi-dence they increase absenteeism,shame, stigma, and unnecessary treat-ment.
The Cost of “No-Nit” PoliciesIt has been estimated that school
children with lice lose an average offour days of school per year in schoolswhere “no-nit” policies are enforced(Gordon, 2009). The loss of theopportunity for learning, funding forschools, and parent/guardian workdays result. Our nation’s schools losebetween $280 to $325 million inannual funding, and families lose upto $2,720 in wages per active infesta-tion (Gordon, 2009). One studyfound that while the presence ofmore than five nits closer than one-quarter inch from the scalp was a riskfactor for the development of anactive infestation, most of these chil-dren did not actually become infested(Williams, Reichert, MacKenzie,Hightower, & Blake, 2001). Just thepresence of nits does not indicate thepresence of an active case of lice, espe-cially if the nits are more thanapproximately one half inch (1 cm)from the scalp.
Even viable nits do not transmitlice. Eggs cannot be transmitted fromone head to another, nor can they falloff the hair shaft. Even if hair with aviable nit falls off, it will not hatch attemperatures lower than the humanhead (Meinking & Taplin, 2011).Should environmental temperaturesstay warm enough that the nymphactually hatches off the head, as anobligate ectoparasite and blood feed-er, it must find a human host or rap-idly succumb within 24 to 48 hours(Frankowski & Bocchini, 2010). Thereis no medical need to eliminateempty egg cases, but removal foresthetic reasons may reduce stigma(Burgess et al., 2003; Gordon, 2007).Additionally, the evidence showsboth lay and health care personnel,even school nurses (who generallyspend the most time of any healthcare professional assessing for lice)actually identify hair casts, hair prod-uct debris, dandruff, and other itemsfound in the hair erroneously as liceor nits equally as often as they do socorrectly (Pollack et al., 2000).
Myth #7. Schools Are aCommon Place for LiceTransmission
Surprisingly, schools rarely pro-vide an opportunity for close head-to-head contact, except for very youngchildren, such as preschool andkindergarten students. For that rea-son, schools are rarely a source for licetransmission. Head lice are most oftena community health issue broughtinto the school setting. Speare,Thomas, and Cahill (2002) found thatwhile 14,000 live lice were found onthe heads of 466 children, no licewere found on the carpets of 118classrooms. Hootman (2002) mappedclassrooms of infested students, andfound all students in the same class-room with lice shared time togetheroutside of school with relatives, orhousehold members, or had partici-pated in a recent sleepover. Clothingstored next to each other, classroomheadphones, riding on the bus to -gether, and playing on the play-ground or in sports are also notsources of transmission (Burgess et al.,2003). The evidence indicates 1% to10% of U.S. children (in kindergartento fourth grade) have an infestation ofhead lice at any one time (Pollock etal., 2000). It is estimated that 10% ofthose may actually be transmitted inschool. It does not make sense toexclude children when the likelihoodof transmission in school is only 1%,far less than the common cold.
Schools often see a spike in casesafter a school break, such as thebeginning of the school year, afterChristmas, and again after springbreak. This is often falsely attributedto a return to the school environ-ment, but is actually due to being inthe community for an extended periodof time (Gordon, 2007). These breaktimes are commonly when childrenhave sleepovers, go to camp, or visitrelatives. They then return to school,and the teacher or school nurse whois familiar with the symptoms identi-fies the infestation. The school, ratherthan being the proximate cause ofinfestation, is the location of its iden-tification.
Current recommendations includenotifying parents at the end of theschool day and providing educationon the proper treatment. The childshould be checked again the nextschool day. Should the parents beunable to provide necessary follow
Exclusion for Live LiceIt also is no longer recommended
to exclude children immediately forlive lice or viable nits, but rather, towait to notify parents/guardians atthe end of the day. In most situations,the child has probably had lice for amonth or more and possesses littlerisk to others (CDC, 2013a; Frankowski& Bocchini, 2010; Mumcuoglu et al.,2007). Any exposure to his or herclassmates has already occurred, andimmediate exclusion provides no fur-ther prevention. No exclusion fromany activities is necessary, includingriding the school bus or participatingin sports.
Shame and StigmaWhen a child is called to the
nurse’s office and does not return, andthen a note goes home at the end ofthe day to check children for possiblelice, it only takes a few questions fromparents/guardians to determine whichof their child’s classmates has lice. Forthe child with persistent lice, theshame and stigma can be devastatingnot only to the child, but to the familyas well. Children may be told theycannot play, sit by, or even be friendswith the child who had/has lice. Headlice are not a health threat. Unlikebody lice, head lice cause no knowndisease other than the occasional top-ical infection from persistent scratch-ing, yet can cause a child to be sociallyostracized (Gordon, 2007)
The Call for the DiscontinuanceThe following groups all call for
elimination of “no-nit” policies:• American Pediatrics Association
(AAP) (Frankowski & Bocchini,2010).
• Centers for Disease Control andPrevention (CDC, 2013a).
• International Guidelines for theTreatment of Pediculosis (Mum -cuoglu et al., 2007).
• National Association of SchoolNurses (NASN, 2011).According to D. Taplin, “If no nit
policies were that effective, why dowe still have so many head lice?”(Burgess et al., 2003, p. 11). However,eliminating “no nit” policies does notmean eliminating a need to treat theinfestation. Whether by chemical ormechanical means, treatment to elim-inate the head lice remains a high pri-ority. Although not dangerous, infes-tation may be uncomfortable andshould be managed.

230 PEDIATRIC NURSING/September-October 2014/Vol. 40/No. 5
Demystifying Pediculosis: School Nurses Taking the Lead
through, further follow up, whichmay include financial assistance withpediculicides, additional educationand how to check and comb out liceand viable eggs, referral for prescrip-tion treatment, or as a rare, very lastresort, exclusion for non-compliance,may be appropriate (Frankowski &Bocchini, 2010; Pontius, 2011). Achild should never lose a day atschool because of lice.
Myth #8. ClassroomChecks Can Limit SpreadOf Head Lice in Schools
It is the position of NASN, theCDC, and AAP that school screenings,either routine or after an identifiedclassroom case, are not productive,cost-effective, or merited, and arewasteful of education time (CDC,2013a, Frankowski & Bocchini, 2010;NASN, 2011). School screenings arenot an accurate way of assessing or pre-dicting which children are or willbecome infested, and such screeningshave not been proven to have a signif-icant effect on the incidence of headlice in a school (Frankowski &Bocchini, 2010; Meinking & Taplin,2011). One study found that misdiag-nosis is so common that non-infestedchildren were excluded from schoolmore often than actually infested chil-dren (Pollack et al., 2000). Anec dotally,prior to the elimination of “no-nit”policies and classroom screening in herdistrict, the author had conductedclassroom screens whenever one stu-dent was found to have head lice.During eight years of such screenings,no further cases of lice were ever foundthat could not be attributed to closecontact outside of school.
Screenings also have significantpotential to violate the children’s pri-vacy. In schools, parents or guardianshave a right to control access to theirchild’s body. This could be violated byroutinely screening students withoutparent/guardian permission. TheNational Pediculosis Association, a laypediculosis interest group, continuesto recommend the strict adherence to“no-nit” policies via nit combing androutine screenings as a way to elimi-nate the need any pediculicides.There is no published, reviewed evi-dence to support these claims (R.Pollack, personal communication,May 21, 2014).
It is prudent, however, to checkclose contacts of a child found to have
HIV or other communicable condi-tion in school. However, they do nothave a legal right to such informa-tion. Although no school would sendhome a letter with a specific child’sname in it, families can easily deter-mine which child is suspected to havelice. This right to confidentiality inschools is protected by the FamilyEducational Rights and Privacy Act(FERPA), and by state and nationalethical health care and educationstandards.
The Family Educational Rights and Privacy Act
FERPA requires that medical andeducational records cannot, withoutparental/guardian consent, be releas edto others without a legitimate educa-tional interest. This is regardless ofwhether the information is written,oral, or electronic (ASHA, 2000; Bergren,2001). Even without disclosing theactual name, if another person can eas-ily determine the identity of a child,then student privacy and confidential-ly has been violated. For example, ifthe nurse were discussing an issue atschool about a child in a wheelchairand only one child is in a wheelchairat school, enough information hasbeen provided to identify that childand breech his or her privacy, withoutever mentioning a name. In a pedicu-losis situation, if after parents receive alice alert letter they ask their own childwho went home from school todayand their child knows the answer, asimilar breech has occurred.
National Ethical Standards And State Laws
Both the professions of educationand nursing have developed codes ofethics that stipulate not disclosinginformation about students obtainedwithin the course of professional serv-ice. For example, provision #3 in theAmerican Nurses Association (ANA)Code of Ethics states “the nurse pro-motes, advocates for and strives toprotect the health, safety and rights ofa patient, which includes both priva-cy and confidentiality” (ANA, 2001,p. 6). Failure to uphold national pro-fessional standards can leave thenurse open to charges of malpractice.
Harm vs. Duty to WarnAccording to ASHA (2000), when
contemplating a disclosure of confi-dential health information even if bydefault, two ethical criteria must bemet. The criteria and related consider-
head lice (Frankowski & Bocchini,2010). A close contact includes allmembers of the household; those whohave recently spent the night; familymembers who travel between house-holds in blended families; childrenwho spend large amounts of time out-side of school with each other, such asday care, camp, or at babysitters; andpreschool and kindergarten childrenwho both sit near each other and playoften together.
Myth #9. Letters to ParentsOr Guardians When a CaseIs Identified at School AreA Good Way to ControlThe Spread of Head Lice
There is no evidence to supportthe claim that letters sent home pre-vent head lice transmission, and theymay, in fact, be a violation of privacyand confidentiality (American SchoolHealth Association [ASHA], 2000;Frankowski & Bocchini, 2010). Thereis no known method to prevent lice(other than by shaving the scalp hair).Sending home a letter may, as itshould, cause parents to check theirstudents to see if they are currentlyinfested. However, this may also cre-ate a false sense of security becauseparents may believe their child is lice-free. There may be undetected, un -hatched viable nits or one pregnantlouse in the hair, or the child mayspend the next night with friend whounknowingly has an infestation.Some parents/guardians will treat pro-phylactically, causing unnecessary useof pediculicides or time-consumingcombing and environmental clean-ing. Sending letters home oftenresults in panic and emotional dis-tress among caregivers. Letters homenot only provoke a crisis situationand unjustified panic, but they per-petuate the myth that lice are trans-mitted in schools (Mumcuoglu et.al,2007). However, some schools contin-ue to send alert letters because whilethey may understand head lice arenot a public health risk, they are concerned about a public relationsdilemma and community backlash(Frankowski & Bocchini, 2010).
Confidentiality Violations Parents or guardians often insist
they have a right to know when a caseof head lice is discovered in a class-room. Parents have also insisted theyhave a right to know when a child has

PEDIATRIC NURSING/September-October 2014/Vol. 40/No. 5 231
ations as they pertain to head liceinclude:
Ethical Criteria 1: Do no harm.Consider the following:• Can the truth of the information be
confirmed? The literature revealshow frequently health care pro-fessionals error in the identifica-tion of head lice. True confirma-tion must be made by micro -scopy.
• How much will the individual andhis or her family’s privacy be violat-ed by this disclosure? Will it harmthem? Stigma, embarrassment,and social humiliation are com-mon for those with head lice.
• Will a decision to disclose do MOREharm than good to the individualwith head lice? Head lice areannoying, but they are not lifethreatening. Stigma, however,can change lives forever.
Ethical Criteria 2: Duty to warn. Con -sider the following: • These circumstances are limited
to very few situations when thepotential for harm is high.
• Examples include child abuse,self-injury, or possible life-threat-ening or serious harm to anotherperson. Because head lice are not danger-
ous and do not cause disease, an infes-tation does not rise to the level of“duty to warn.” Further, because dis-closure, however inadvertent, maycause great harm to the family withhead lice through social stigma, theright to privacy and confidentialitymust be upheld for the student andfamily experiencing lice. Parents/guardians are better served ratherthan receiving alert letters, receivingregularly scheduled head lice infor-mation letters several times duringthe year (most appropriately at thetimes when children are returningfrom the community after schoolbreaks). Suggested contents includereminders to regularly check theirchildren’s hair (weekly for elementaryage students) for any evidence of headlice, how to check, and treatmentinstructions (Gordon, 2009).
Myth #10. If One MemberOf the Household Has Lice,Everyone Should BeTreated
Treatment should be initiatedonly when there is clear evidence ofhead lice. When lice are identified in
information. In addition, families willself-treat an average of five timesbefore seeking the help of a healthcare professional (Gordon, 2009). Thecost of seeing a health care provider,plus the additional cost of a prescrip-tion medication and the stigma asso-ciated with head lice, are often thereasons many families will initiallyseek alternative information andtreatments. Experts recommend refer-ral to a health care provider after twotreatment failures (Burgess et al.,2003). According to the treatment pro -tocol recommended by the AmericanAcademy of Pediatrics (2012), “Fortreatment failures not attributable toimproper use of an over-the counterpediculicide, mala thion, benzyl alco-hol lotion, or spinosad suspensionshould be used” (p. 4). Several pre-scription medications exist, withthree new medications receiving FDAapproval in the last five years (seeTable 1). Each of these pediculicidesmust be used according to the direc-tions. Some require a second treat-ment to ensure eradication of newlyhatched nymphs. Others re quire anextended time on the head. Theschool nurse can help assure treat-ment success by making sure explana-tions of options and instructions foruse are clear and understood by thecaregiver. Finally, there is some evi-dence that a device that uses hot air todesiccate the insects may be effective(Frankowski & Bocchini, 2010). How -ever, the device is expensive and notreadily available.
Lice Removal ServicesDelousing/nit picking services
have expanded across the county inthe last decade. These primarily for-profit businesses espouse to providerelief for families who are eitherunable or unwilling to do mechanicallice and egg removal, and/or prefernot to use pediculicides. However,unlike barbers and beauticians whoalso manipulate hair, such businessesare unregulated. Workers are nothealth care professionals and are gen-erally trained by the establishment(Pollack, 2012). Noted lice expertRichard Pollack (personal communi-cation, May 21, 2014) is unconvincedof the need for such services, andbelieves when the nature of the busi-ness is to sell head lice control servicesand proprietary supplies, it is not sur-prising to see these salons aggressivelyarguing in favor of no-nit policies,and perhaps suggesting that “out-
one family member, all householdmembers and close contacts shouldbe examined. Treat only those con-tacts that actually have crawling liceor viable eggs. Prophylactic treatmentis unnecessary and time-consuming,and exposes persons to medicationsunnecessarily. All persons with headlice should be treated at the sametime, otherwise they could re-infesteach other (CDC, 2013a).
Myth #11. Pediculicides Are Dangerous and Should Be Avoided
Treatment choices for lice shouldbe based on any local patterns of re -sistance, ease of use, and cost. Figure 5describes a suggested treatment regi-men. If the hair is fine and untangled,and the caregiver is motivated, usinga fine-toothed comb and methodical-ly combing through all hair on thehead, both to examine the head forlive lice, and to remove the viable nitsand the lice, can be effective. Thisprocess must be repeated every fewdays for at least two weeks, to elimi-nate each new louse as it hatches.Because this is so time-consuming,and most families want the problemsolved immediately, use of FederalDrug Administration (FDA)-approvedpediculicides, which are safe whenused as directed, can be used as anadjunct or to replace combing (Burgesset al., 2003; CDC, 2013a). The safetyand effectiveness of home or “natur-al” remedies, such as olive oil, tea-treeoil, lavender oil, or mayonnaise, arenot regulated by the FDA and havenot been shown to be effective in any known double-blind studies, and are therefore not recommended(Frankowski & Bocchini, 2010)
PediculicidesOver-the-counter (OTC) prepara-
tions or permethrin (e.g., Nix®) andpyrethrins (e.g., RID®, Clear®, Pronto®)remain as the first line choice forpediculicidal treatment. Even in lightof some developing resistance topyrethrins, they remain very effec-tive. They are inexpensive and haveextremely low toxicity. Pyrethrins area natural chrysanthemum extract,and permethrin is a synthetic pyre -throid. Both are neurotoxic to lice(Frankowski & Bocchini, 2010).
Evidence has shown that manyfamilies rely on peers, and increasing-ly, the Internet, for their treatment

232 PEDIATRIC NURSING/September-October 2014/Vol. 40/No. 5
Demystifying Pediculosis: School Nurses Taking the Lead
Source: © 2010 IdentifyUS, LLC. Used with permission. Retrieved from https://identify.us.com/idmybug/head-lice/head-lice-documents/lice-mgmnt-chart-home.pdf
Figure 5.Suggested Scheme for Head Louse Infestations
Managing Presumed Head Louse Infestations at Home
“Nits”discovered
on hair?
Live(crawling)
lice onhair?
Is the hairreadily combed
with a lousecomb?
Do live (crawling)lice persis after the second treatment?
• Inspect hair for live (crawling) lice.• Compare samples to images on our website
or submit a sample for evaluation.• Inspect all other people in the home for live
lice.
• Apply an FDA-registered over-the-counter pediculicideaccording to label directions.
• Change or launder pillowcases,pajamas, and towels that werein direct contact with theinfested person within the pastday.
• If live (crawling) lice persist, asecond application may beneeded about 10 days after thefirst treatment.
• Consult your physician orpharmacist for advice.
• Consult with your physician.• Consider prescription pediculicides that
contain an active ingredient different thanthat of your over-the-top counter product.
• Removal of remaining nuts should be apersonal choice, as these are likely to allbe dead or hatched.
• Change or launder pillowcases, pajamas,and towels exposed to lice within the pastday.
Relax! DoNOT treatfor lice.
Periodicallyreinspect hairfor live lice. Do NOT treat.
Treat
• Comb hair thoroughly with a louse comb.• Use hair conditioner to lubricate and comb.
Many lice and eggs should be removed during the first combing session.
• Repeat every few days. Subsequent combingwill remove another portion of the remaining,as well as any new, lice and eggs.
• Continue periodic combing until no live liceare discovered for an interval of about twoweeks.
• Treatment with pediculicides may supplementor replace combing.
Yes
Yes
No
No
No
Yes Yes

PEDIATRIC NURSING/September-October 2014/Vol. 40/No. 5 233
breaks” or “epidemics” of head lice areoccurring. The cost can be quiteexpensive, with a session costing sev-eral hundred dollars or more. There isno evidence to support recommend-ing these services.
Myth #12. Head Lice AreBecoming IncreasinglyResistant to Pediculicides
Several studies have reportedsome increase in local resistance toOTC pediculicides in the last 20 years,receiving prominent lay press cover-age. However, the prevalence of actualresistance is unknown because clinicaltrials have used different inclusion cri-teria, resulting in different conclu-sions (Frankowski & Bocchini, 2010;Pollack et al., 2000). Most recently,Yoon et al. (2014) found by DNA typ-
ing of lice in several locations in theU.S. and Canada, the rate of T1 muta-tion (the gene mutation most respon-sible for permethrin resistance) variedbetween 84.4% and 99%. While thissuggests increasing resistance to per-methrin and pyre thrins-based pedi-culicides, one must be careful inextrapolating these results becausetheir study examined a small numberof lice from only 12 U.S. states andstudied the potential for resistance,rather than a clinical measurement ofactual resistance. What matters mostis the degree to which head lice havebecome resistant in each community(Burgess et al., 2003). Studies on resist-ance and efficacy are ongoing.
Resistance is often branded as theproximate cause of treatment failurewhen head lice are not eradicated by apediculicide. However, these treat-
Table 1. Medications
Age Notes
Over-the-Counter Medications
Permethrinlotion, 1%
2 monthsand older
• Kills live lice but not unhatched eggs.• A second treatment often is necessary on day 9
to kill any newly hatched lice before they canproduce new eggs.
Pyrethrins 2 years andolder
• Generally should not be used by persons whoare allergic to chrysanthemums or ragweed.
• A second treatment is recommended 9 to 10days after the first treatment to kill any newlyhatched lice before they can produce new eggs.
Prescription Medications
Benzylalcohol lotion(0.5%)
6 monthsand older
• Kills lice but not eggs.• A second treatment is needed 7 days after the
first treatment to kill any newly hatched licebefore they can produce new eggs.
Ivermectinlotion, 0.5%
6 monthsand older
• Kills live lice and appears to prevent nymphs(newly hatched lice) from surviving.
• It is effective in most patients when given as asingle application on dry hair without nit combing.
• It should not be used for retreatment withouttalking to a health care provider.
Malathionlotion, 0.5%
6 years andolder
• Kills live lice and some lice eggs.• A second treatment is recommended if live lice
still are present 7 to 9 days after treatment.
Spinosad0.9% topicalsuspension
4 years andolder
• Kills live lice and unhatched eggs. • Retreatment usually not needed and should be
given only if live (crawling) lice are seen 7 daysafter first treatment.
Source: Adapted from CDC, 2013b.
ment failures are more commonly theresult of: • Misdiagnosis (no active infesta-
tion, or misidentification).• Non-compliance (not following
treatment protocol).• New infestation (lice acquired
after treatment).• Lack of ovicidal (egg-killing) or
residual properties of the product(Burgess et al., 2003; Frankowski& Bocchini, 2010).Pollack et al. (2000) found the
most common reason for a conclusionof “resistance” was actually misdiag-nosis; therefore, it could not be effec-tively treated with a pediculicisde. Ofthe 555 samples sent in and initiallyidentified as head lice, only 57.5%were correctly diagnosed and con-firmed as such by an entomologist.Family identifications were only 47%correct, and physicians had the worstidentification rate at 11% correct. Thehealth care pro vider should considerresistance after assuring oneself theabove factors have not contributed tothe treatment failure.
Nurses as Change AgentsPediatric nurses working both in
and out of schools can lead the chargeto help schools design evidence-basedpolicies that respect the privacy andconfidentially of students yet promotesuccessful treatment of infestations.NASN, in its position statementregarding pediculosis (NASN, 2011),described that school nurses are thekey health care professionals in theprovision of education and anticipato-ry guidance in all aspects of the man-agement of pediculosis in the schoolsetting. Additionally, school nursesplay an important roll in helping localpharmacists, health care providers,and community health districts inupdating their knowledge of currentstate of pediculosis science. Providingeducation to reduce the stigma of lice,clarify myths, and provide accurateinformation about effective treatmentoptions, as well as appropriate referralsto health care providers, is importantnursing care. Table 2 gives an exampleof a parent-teaching tool, designed bythe author using the principles ofhealth literacy to effectively disputethe common myths of lice manage-ment. NASN provides free, profession-ally produced, evidence-based parentand nurse educational tools in theirLice Lessons program (visit http://www.nasn.org for more information).

234 PEDIATRIC NURSING/September-October 2014/Vol. 40/No. 5
Article title goes here on master page for left hand page (LHF)
Even in light of evidence to thecontrary, the lay public, includingteachers and school administrators,often remain unconvinced of the needto remove “no-nit” policies and will beunmotivated to do so on their own.Further, some experts believe the onlyhope for true success is to focus on thechildren. “Teach them to think, toevaluate conflicting bits of informa-tion and to form logical and rationalconclusions, and to be compassionateand caring” (R. Pollack, personal com-munication, May 21, 2014) to helpchildren develop a new reality abouthead lice. Armed with the evidence,
ReferencesAmerican Nurses Association (ANA). (2001).
Code of ethics for nurse. Retrieved fromhttp://www.nursingworld.org/MainMenuCategories/EthicsStandards/CodeofEthicsforNurses/Code-of-Ethics.pdf
American Academy of Pediatrics (AAP).(2012). Red book: 2012 report of theCommittee of Infectious Diseases. ElkGrove Village, IL: Author.
American School Health Association(ASHA). (2000). National Task Force onConfidential Student Health Infor -mation. Guidelines for protecting confi-dential student health information. Kent,OH: ASHA.
Bergren, M. (2001). HIPAA hoopla: Privacyand security of identifiable health infro-
school nurses are the perfect changeagent to promote policy improvementto match what the evidence showsabout the transmission and treatmentof pediculosis. Not only can nursesprovide education with every interper-sonal en counter, they can lobby theirschool board. Following the examplesset by leaders in school districts such asOakland Unified, the author did justthat (see Figure 6). Because manyhealth care professionals are unawareof the realities of lice and newer licetreatments regimes, school nurses, aswell as pediatric nurses in general, arein the ideal position to lead the charge!
Table 2.Lice 101: Myths and Realities about Head Lice
Definitions
Lice: More than one louse. Nit: Eggs, dead or alive, of a louse
Louse: Small insect that lives on the scalp. Parasite: Lives off another, in this case the blood of humans.
Pediculosis: Having an infestation of lice. Infestation: Having an insect present, in this case, in your head.
Myths Truths
Head lice are easy to get. Lice are spread only mainly by head-to-head contact. They are much harderto get than a cold, flu, ear infection, pink eye, strep throat, food poisoning, orimpetigo.
You can get lice from your dog, guinea pig, orother animal.
Lice are species-specific. You can only get human lice from another human.You cannot get another animal’s lice.
You can get head lice from hats and helmets. Rarely, but possible. Hairbrushes, pillows, and sheets are also uncommonmodes of transmission.
School is a common place for lice transmission. School is an unlikely source of transmission. Much more common are familymembers, overnight guests, and playmates who spent a large amount oftime together.
Poor hygiene contributes to lice. Hygiene makes absolutely no difference. You get lice by close personalhead-to-head contact with someone else that has lice, not by being dirty.
Lice can jump or fly from one person to another. Lice can only crawl. They can neither fly nor jump. They must crawl fromone person to another.
Any nits left in the hair can cause lice to comeback.
Any nits farther away than one quarter to one half on the hair shaft areALREADY HATCHED and pose no risk to others.
Eggs or nits can fall out of the hair, hatch, andcause lice in another person.
Nits are cemented to the hair and very hard to remove. They cannot fall off.Newly hatched lice must find a head quickly or will die.
Lice can live a long time. Lice live only 1 to 2 days off the head. Each louse only lives about 30 dayson the head.
All members of a family should be treated if oneperson has lice.
Only the person with lice should be treated. Lice shampoos are INSECTICIDES and can be dangerous if used incorrectly or too frequently.Household members and close contacts should be checked, but only treatthose who actually have lice. The house should NOT be sprayed with insecticide, nor used on clothing or other items.
Checking a classroom when one student has licecan prevent lice from spreading.
Classroom transmission is EXCEEDINGLY RARE and checking students isa waste of valuable teaching time. Checking family members and closeplaymates is much more appropriate.
Avoiding lice is important as they spread disease. Head lice do not spread any known disease. They are annoying and irritating, but not dangerous.

PEDIATRIC NURSING/September-October 2014/Vol. 40/No. 5 235
mation. Journal of School Nursing,17(6), 336-340.
Burgess, I., Pollack, R., & Taplin, D. (2003).Cutting through controversy: Specialreport on the treatment of head lice.Englewood, CO: Postgraduate Institutefor Medicine.
Centers for Disease Control and Prevention(CDC). (2013a). Head lice informationfor schools. Retrieved from http://www.cdc.gov/parasites/lice/head/index.html
Centers for Disease Control and Prevention.(2013b). Head lice treatment. Retrievedfrom http://www.cdc.gov/parasites/lice/head/treatment.html#otc
Centers for Disease Control and Prevention(CDC). (2013c). Head lice biology.Retrieved from www.cdc.gov/parasites/lice/head/biology.html
Centers for Disease Control and Prevention(CDC) Public Health Image Library.(2014). Homepage. Retrieved fromwww.cdc.gov/phil/home.asp
Frankowski, B., & Bocchini, J. (2010). Clinicalreport – Head lice. Pediatrics, 126(2),392-403.
Gordon, S. (2007). Shared vulnerability: Atheory of caring for children with persist-ent head lice. The Journal of SchoolNursing, 23(5), 283-292.
Gordon, S. (2009). Head lice management inschool settings. Orlando, FL: FloridaAssociation of School Nurses.
Hootman, J. (2002). Quality improvementprojects related to pediculosis manage-ment. The Journal of School Nursing,18(2), 80-86.
Loussouarn, G., Rawadi, C., & Genain, G.(2005). Diversity of hair growth profiles.International Journal of Dermatology,44(Suppl. 1), 6-9.
Meinking, T., & Taplin, D. (2011). Infestations.In L. Schachner, & R. Hansen (Eds.),Pediatric dermatology (pp. 1525-1583).Philadelphia: Mosby Elsevier.
Mumcuoglu, K.B., Barker, F.C., Burgess, I.F.,Combescot-Lang, C., Dalgleish, R.C.,Larsen K.S., … Taylan-Ozkan, A.(2007). International guidelines foreffective control of head louse infesta-tions. Journal of Drugs in Dermatology,6(4), 409-414.
National Association of School Nurses (NASN).(2011). Position Statement: Pediculosisin the school settings. Silver Spring,MD: Author. Retrieved from http://www.nasn.org/Portals/0/positions/2011pspediculosis.pdf
Pollack, R. (2012). Louse and nit removingsalons. IDmy Bug. Retrieved fromhttp://idmybug.tumblr.com/post/17920155632/louse-nit-removing-salons
Pollack, R., Kiszewski, A., & Spielman, A.(2000). Overdiagnosis and consequentmismanagement of head louse infesta-tions in North America. Pediatric infec-tious Disease Journal, 19(8), 689-693.
Pontius, D. (2011). Hats off to success:Changing head lice policy. NASNSchool Nurse, 26(6), 356-362.
Speare, R., Cahill, C., & Thomas, G. (2003).Head lice on pillows, and strategies tomake a small risk even less. Inter -national Journal of Dermatology, 42(8),626-629.
Speare, R., Thomas, G., & Cahill, C. (2002).Head lice are not found on floors in pri-mary school classrooms. Australian &New Zealand Journal of Public Health,26(3), 207-208.
Williams, L., Reichert, M., MacKenzie, W.,Hightower, A., & Blake, P. (2001). Lice,nits and school policy. Pediatrics,107(5), 1011-1015.
Yoon, K., Previte, D., Hodgdon, H., Poole, B.,Kwon, D., Abo El-Ghar, G., … Clark, J.(2014). Knockdown resistance allelefrequencies in North American headlouse populations. Journal of MedicalEntomology. 51(2), 450-457. doi:10.1603/ME1313
Instructions For Continuing Nursing Education
Contact HoursDemystifying Pediculosis:
School Nurses Taking the Lead
Deadline for Submission: October 31, 2016
PED 1407 To Obtain CNE Contact Hours1. For those wishing to obtain CNE contact
hours, you must read the article and com-plete the evaluation through PediatricNursing’s Web site at www.pediatricnursing.net/ce
2. Evaluations must be completed onlineby the above deadline. Upon completionof the evaluation, your CNE certificatefor 1.3 contact hour(s) will be mailed toyou.
Fees – Subscriber: Free Regular: $20
Goal
To provide an overview of head lice anddemystify the common misperceptionssurrounding it.
Objectives1. Define Pediculosis capitis.2. List the common myths about head lice
and nits.3. Explain the implications these myths
have on school children and theirfamilies.
4. Discuss ways school nurses mayeducate their community and schoolsabout lice and nits, and thus, discouragethe enforcement of “no-nit” policies.
Statement of Disclosure: The author(s) re port - ed no actual or potential conflict of interest inrelation to this continuing nursing education act -ivity.
The Pediatric Nursing Editorial Board membersreported no actual or potential conflict of interestin relation to this continuing nursing educationactivity.
This independent study activity is providedby Anthony J. Jannetti, Inc. (AJJ).
Anthony J. Jannetti, Inc. is accredited as aprovider of continuing nursing education by theAmerican Nurses Credentialing Center's Com -mission on Accreditation.
Anthony J. Jannetti, Inc. is a providerapproved by the California Board of RegisteredNursing, Provider Number, CEP 5387.
Licenses in the state of California mustretain this certificate for four years after the CNEactivity is completed.
This article was reviewed and formatted forcontact hour credit by Rosemarie Marmion,MSN, RN-BC, NE-BC, Anthony J. Jannetti, Inc.,Education Director; and Judy A. Rollins, PhD,RN, Pediatric Nursing Editor.
Source: Pontius, 2011.
Figure 6.Real Life Application
Using the evidence presented here, the author’s district now allows both nits andlive lice, does not send home specific alert letters, informs and educates parents/guardians at the end of the school day, and most importantly, provides copiousteaching to families and children. In the four years hence, there has been noincrease in infestation incidence, and although there is the occasional upset parent,overall the community has accepted these policies.
Related Documents