-
8/3/2019 Anaemia and Thalassaemia
1/61
Anaemia and
Thalassaemia
Luke Woon Sy-Cherng
-
8/3/2019 Anaemia and Thalassaemia
2/61
Introduction
Haematopoiesis is the production anddevelopment of blood cells
Occurs in 3 stages:
Mesoblastic
Hepatic
myeloid
From pluripotent stem cells to progenitorcells of different cell lines
-
8/3/2019 Anaemia and Thalassaemia
3/61
Introduction
Erythropoiesis: regulated by erythropoietin(EPO)
Haemoglobin (Hb): tetramer (2 pairs ofpolypeptide chains) + heme group
Embyronic Hb: Hb Gower 1, Hb Gower 2,Hb Portland
Fetal Hb: Hb F (22)
Adult Hb: Hb A (22), Hb A2 (22)
-
8/3/2019 Anaemia and Thalassaemia
4/61
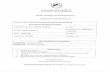
Figure 1. Model of the haemoglobin molecule showing (pink) and (blue) chains. 2,3-BPG(bisphosphoglycerate) binds in the centre of the molecule and stabilizes the deoxygenated form by
cross-linking the chains. M, methyl; P, propionic acid; V, vinyl.
Downloaded from: StudentConsult (on 4 March 2009 10:57 AM)
2005 Elsevier
Introduction
-
8/3/2019 Anaemia and Thalassaemia
5/61
Introduction
Fetal Hb has higher affinity than adult Hb
Fetal Hb is gradually replaced by adult Hb duringthe 1st yr of life
Proportion of Hb:
BirthHbF 70 80%, HbA 25
30%, HbA2
1 3%
Adults HbA 97%, HbA2 2%
-
8/3/2019 Anaemia and Thalassaemia
6/61
Introduction
Lifespan of neonatal RBC is 60 90 d
Hb is high at birth (14 21.5 g/dl), becomethe lowest at 2 mo (10 g/dl)
Average blood volume 80 ml/kg
-
8/3/2019 Anaemia and Thalassaemia
7/61
Anaemia
Anaemia: Hb level below the normal range
Common features of anaemia:
Pallor Weakness, palpitations
Tachypnoea, tachycardia
Congestive heart failure
Neonate < 14 g/dl
1 12 mo < 10 g/dl
1 12 yr < 11 g/dl
-
8/3/2019 Anaemia and Thalassaemia
8/61
Anaemia
Anaemia results from:
Impaired production:
Ineffective erythropoiesis
Red cell aplasia
Haemolysis
Blood loss
-
8/3/2019 Anaemia and Thalassaemia
9/61
Anaemia
Ineffective erythropoiesis:
Deficiency:
iron deficiency
folic acid deficiency
vitamin B12 deficiency
Anaemia of chronic disease (ACD)
Anaemia of renal disease
-
8/3/2019 Anaemia and Thalassaemia
10/61
Iron Deficiency Anaemia
Caused by: Inadequate intake (> 6 mo, excessive cow
milk intake)
Malabsorption Blood loss (e.g. hookworm infestation)
Manifestations :
Hb < 6 7 g/dl Pallor, tiredness
Pica
Intellectual impairment
-
8/3/2019 Anaemia and Thalassaemia
11/61
Iron Deficiency Anaemia
Investigations:
Hypochromic, microcytic anaemia
Poikylocytosis, anisocytosis Low serum ferritin & high total iron binding
capacity (TIBC)
Elevated transferrin receptor (TfR) DD: - & -Thalassaemia trait, ACD
-
8/3/2019 Anaemia and Thalassaemia
12/61
Figure 2. Hypochromic microcytic cells (arrow) on a blood film. Poikilocytosis and anisocytosisare seen.
Downloaded from: StudentConsult (on 4 March 2009 10:57 AM)
2005 Elsevier
Iron Deficiency Anaemia
-
8/3/2019 Anaemia and Thalassaemia
13/61
Iron Deficiency Anaemia
Treatment:
Oral ferrous salts:
E.g. FeSO4
(20% elemental iron)
4 6 mg/kg/d elemental iron
Hb 1 g/dl per wk, continue for 3 mo
Underlying cause: dietary advice, stopblood loss etc
Packed cell transfusion: very severeanaemia only
-
8/3/2019 Anaemia and Thalassaemia
14/61
Folic Acid Deficiency
Caused by:
Inadequate intake (e.g. haemolysis)
Decreased absorption (e.g. chronic diarrhoea) Metabolic abnormalities
Manifestations:
Anaemia, irritability Associated features (e.g. malnutrition)
-
8/3/2019 Anaemia and Thalassaemia
15/61
Folic Acid Deficiency
Investigation: Macrocytic anaemia
Low reticulocyte count
Neutrophil: hypersegmented nuclei Low serum folic acid
Bone marrow: megaloblast
DD: vitamin B12 deficiency Treatment:
Folic acid 0.5 1 mg/d
Transfusion: very severe case
-
8/3/2019 Anaemia and Thalassaemia
16/61
Figure 3. Macrocytes and a hypersegmented neutrophil (arrowed) on a peripheral blood film.
Downloaded from: StudentConsult (on 4 March 2009 11:05 AM)
2005 Elsevier
Folic Acid Deficiency
-
8/3/2019 Anaemia and Thalassaemia
17/61
Vitamin B12 Deficiency
Caused by: Inadequate intake (rare)
Lack of intrinsic factor (IF): pernicious
anaemia Impaired absorption (e.g. regional enteritis)
Transcobalamin II deficiency (rare)
Manifestations: Anaemia, glossitis Neurologic symptoms: parasthesiae, seizures,
developmental delay
-
8/3/2019 Anaemia and Thalassaemia
18/61
Vitamin B12 Deficiency
Investigations: Macrocytic anaemia
Hypersegmented neutrophil
Bilirubin may be raised Low serum vitamin B12
Bone marrow: megaloblast
Schilling test: radioactive vitamin B12 IF Treatment:
Parenteral vitamin B12
-
8/3/2019 Anaemia and Thalassaemia
19/61
Anaemia of Chronic Disease
Associated with infection, inflammation ortissue breakdown (e.g. bronchiectasis, SLE)
Blunted response to EPO and decreasediron availability
Manisfestations: anaemia with underlyingdisease
Investigations:
Normocytic normochromic anaemia
Low serum iron, normal TIBC
-
8/3/2019 Anaemia and Thalassaemia
20/61
Anaemia of Chronic Disease
Elevated serum ferritin
Normal TfR
Treatment:
Underlying disease
Recombinant human EPO
-
8/3/2019 Anaemia and Thalassaemia
21/61
Anaemia of Renal Disease
Due to: Reduced EPO production
Bone marrow suppression
Reduced lifespan of RBC Haematinic deficiency
Increased blood loss
Normocytic normochromic anaemia Laboratory evidence of renal failure
Treatment: recombinant human EPO
-
8/3/2019 Anaemia and Thalassaemia
22/61
Red Cell Aplasia
Pure red cell aplasia
Diamond-Blackfan anaemia (DBA)
Transient erythroblastopenia of childhood
(TEC)
Red cell aplasia associated with chronichaemolysis
Aplastic anaemia (pancytopenia) Inherited aplastic anaemia
Acquired aplastic anaemia
-
8/3/2019 Anaemia and Thalassaemia
23/61
Diamond-Blackfan Anaemia
Congenital hypoplastic anaemia
Gene mutation increased apoptosis
Majority are sporadic cases Usually presented with profound anaemia
at 2 6 mo
Congenital anomalies e.g. short stature,abnormal thumbs
Treatment: oral steroids or transfusions
-
8/3/2019 Anaemia and Thalassaemia
24/61
Transient Erythroblastopenia of
Childhood
Triggered by viral infections
Recover within 1 2 mo
Severe anaemia may need transfusionsRed Cell Aplasia associated with
Chronic Haemolysis
Caused by parvovirus B19 infection
Aplastic crisis in patients with haemolysis
Transfusion may be needed
-
8/3/2019 Anaemia and Thalassaemia
25/61
Aplastic Anaemia
Pancytopenia with hypocellularity of thebone marrow
Presented with anaemia, infection and
bleeding Divided into:
Inherited: Fanconi anaemia, Schwachman-
Diamond syndrome, etc Acquired: viral infections (e.g. hepatitis),drugs (e.g. chloramphenicol), chemicals (e.g.benzene), radiation, infiltration
-
8/3/2019 Anaemia and Thalassaemia
26/61
Figure 4. Bone marrow trephine biopsies in low-power view. Hypocellularity in aplastic anaemia.
Downloaded from: StudentConsult (on 4 March 2009 11:05 AM)
2005 Elsevier
Aplastic Anaemia
-
8/3/2019 Anaemia and Thalassaemia
27/61
Haemolytic Anaemia
Reduced red cell lifespan due to increaseddestruction
Presented with anaemia, jaundice andhepatosplenomegaly
Investigation:
reticulocyte count/polychromasia
unconjugated bilirubin and urobilinogen
Abnormal red cells on blood film
-
8/3/2019 Anaemia and Thalassaemia
28/61
Haemolytic Anaemia
Inherited Membrane defects: hereditary spherocytosis,
hereditary elliptocytosis Metabolic defects: G6PD deficiency, pyruvate
kinase deficiency Haemoglobinopathies: thalassaemia, sickle
cell diseaseAcquired
Immune: haemolytic disease of the newborn,autoimmune haemolytic anaemia
Non-immune: malaria, DIC, hypersplenism
-
8/3/2019 Anaemia and Thalassaemia
29/61
Hereditary Spherocytosis
Autosomal dominant, 25% sporadic
Abnormalities of structural proteins (e.g.spectrin, ankyrin) spheroidal shape
destruction in spleen Presented with:
Neonatal jaundice
Anaemia Splenomegaly
Aplastic crisis
gallstones
-
8/3/2019 Anaemia and Thalassaemia
30/61
Hereditary Spherocytosis
Investigations:
Blood film: spherocytes
Osmotic fragility test: positive
Coombs test: negative
Treatment:
Folic acid supplementation
Splenectomy
-
8/3/2019 Anaemia and Thalassaemia
31/61
Figure 5. Spherocytes (arrowed). This blood film also shows reticulocytes, polychromasias and anucleated erythroblast.
Downloaded from: StudentConsult (on 4 March 2009 11:05 AM)
2005 Elsevier
Hereditary Spherocytosis
-
8/3/2019 Anaemia and Thalassaemia
32/61
G6PD Deficiency
The commonest red cell enzymopathy Prevalent in Southeast Asia
X-linked recessive enzyme deficiency
Glucose-6-phosphate dehydrogenase(G6PD) is an enzyme in the pentosephosphate pathway
Needed for the reduction of oxidizedglutathione, which is responsible for theprotection against oxidative stress
Deficiency intravascular haemolysis
-
8/3/2019 Anaemia and Thalassaemia
33/61
G6PD Deficiency
Presented with:
Neonatal jaundice
Acute haemolysis, precipitated by: Infections
Drugs (e.g. antimalarials, sulphonamides)
Naphthalene
Fava beans
Anaemia, jaundice, haemoglobinuria
-
8/3/2019 Anaemia and Thalassaemia
34/61
G6PD Deficiency
Investigation: Blood film: blister cells, Heinz bodies
Reduced G6PD activity
Treatment: Underlying cause (e.g. withdraw offending
drug)
Blood transfusions
Adequate hydration
Prevention of haemolysis: avoidprecipitating factors
-
8/3/2019 Anaemia and Thalassaemia
35/61
Figure 6. 'Blister' cells (arrowed) in G6PD deficiency.
Downloaded from: StudentConsult (on 4 March 2009 11:05 AM)
2005 Elsevier
G6PD Deficiency
-
8/3/2019 Anaemia and Thalassaemia
36/61
Thalassaemia
Genetic disorder of globin chain ( or )production, leading to ineffectiveerythropoiesis and haemolysis
Common along the Thalassaemia Belt,including Southeast Asia
Divided into:
-Thalassaemia
-Thalassaemia
-
8/3/2019 Anaemia and Thalassaemia
37/61
Figure 7. Major haemoglobin abnormalities: geographical distribution.Downloaded from: StudentConsult (on 4 March 2009 11:05 AM) 2005 Elsevier
Thalassaemia
-
8/3/2019 Anaemia and Thalassaemia
38/61
-Thalassaemia
chain production: reduced (+) or none(0)
Increased HbA2 and HbF
Excessive chains precipitation ineffective erythropoiesis and haemolysis
Clinically divided into:
Thalassaemia major (Cooleys anaemia) Thalassaemia intermedia
Thalassaemia minor/trait
-
8/3/2019 Anaemia and Thalassaemia
39/61
Thalassaemia Major
Homozygous -thalassaemia (0/0, +/+)
Presented with:
Failure to thrive, recurrent infections
Severe anaemia from 3 6 mo
Extramedullary erythropoiesis:hepatosplenomegaly, thalassaemic facies (
frontal bossing, flat nasal bridge, maxillaryhyperplasia)
-
8/3/2019 Anaemia and Thalassaemia
40/61
Figure 8. A child with thalassaemia, showing the typical facial features.
Downloaded from: StudentConsult (on 4 March 2009 11:05 AM)
2005 Elsevier
Thalassaemia Major
-
8/3/2019 Anaemia and Thalassaemia
41/61
Thalassaemia Major
Investigation: Severe microcytic hypochromic anaemia
Blood film: deformed red cells
Skull X-ray: bone marrow hyperplasia
Diagnosis confirmed by Hb electrophoresis
Treatment: Monthly transfusion (keep Hb 10 g/dl)
Folic acid supplementation Splenectomy
Bone marrow transplantation
Genetic counseling
-
8/3/2019 Anaemia and Thalassaemia
42/61
Figure 9. Skull x-ray of a child with thalassaemia, showing the hair on end appearance.
Downloaded from: StudentConsult (on 4 March 2009 11:05 AM)
2005 Elsevier
Thalassaemia Major
-
8/3/2019 Anaemia and Thalassaemia
43/61
Figure 10. Patterns of haemoglobin electrophoresis.
Downloaded from: StudentConsult (on 4 March 2009 11:05 AM)
2005 Elsevier
Thalassaemia Major
-
8/3/2019 Anaemia and Thalassaemia
44/61
Thalassaemia Major
Transfusion haemosiderosis
Iron overload cause by repeatedtransfusions
Cardiomyopathy, hepatic cirrhosis,diabetes mellitus, delayed growth & sexualmaturation, bronze pigmentation of skin
Iron status monitoring: serum ferritin,hepatic iron
-
8/3/2019 Anaemia and Thalassaemia
45/61
Thalassaemia Major
Transfusion haemosiderosis
Prevention:
Iron-chelating agents
Desferrioxamine (Desferal), SC over 8 12hr, 5 7 d per week (SE: nerve deafness,cataracts, retinal damage)
Ascorbic acid 100 250 mg/d Low iron diet, tea drinking
-
8/3/2019 Anaemia and Thalassaemia
46/61
Thalassaemia Minor
Heterozygous -thalassaemia/carrier state(0/, +/)
No or mild anaemia
Microcytic hypochromic red cells,increased red cell count
DD: iron deficiency anaemia
Normal iron stores
Diagnosis: Hb electrophoresis
-
8/3/2019 Anaemia and Thalassaemia
47/61
Thalassaemia Intermedia
Moderate anaemia (Hb 7 10 g/dl)
Do not require regular transfusions
Combinations of -thalassaemia mutations(0/+, 0/variant, etc), -thalassaemia & -thalassaemia, -thalassaemia & hereditarypersistence of fetal haemoglobin
Extramedullary erythropoiesis may occur
-
8/3/2019 Anaemia and Thalassaemia
48/61
Haemoglobin E
Hb E (2226glulys) is the most common Hb
variant in Southeast Asia
Heterozygous Hb E: asymptomatic,
microcytic red cells
Homozygous Hb E: mild microcyticanaemia
Hb E/-thalassaemia thalassaemiamajor
-
8/3/2019 Anaemia and Thalassaemia
49/61
-Thalassaemia
4 genes for -chains Caused by gene deletions:
4-gene deletion: no -chain, only Hb Barts
(4) hydrops fetalis 3-gene deletion: Moderate anaemia and
splenomegaly, Hb Barts and Hb H (4)present Hb H disease
2-gene deletion: -thalassaemia trait,microcytosis mild anaemia, Hb H present
1-gene deletion: silent trait, normal bloodpicture
-
8/3/2019 Anaemia and Thalassaemia
50/61
Mostly found in Southeast Asia
Diagnosis confirmed by DNA analysis: -globin gene deletion
Treatment: Folic supplementation
Splenectomy
Hb H disease: intermittent transfusion Hydrops fetalis: chronic transfusion/bone
marrow transplant
-Thalassaemia
-
8/3/2019 Anaemia and Thalassaemia
51/61
Sickle Cell Disease
Sickle cell Hb (Hb S): point mutation(22
6gluval)
Homozygous (Hb SS): sickle cell anaemia
Heterozygous (Hb AS): sickle cell trait Combined heterozygocity (Hb SC):
intermediate symptoms
Mainly among Africans Deoxygenated Hb S polymerization
sickling haemolysis and vascularobstruction
-
8/3/2019 Anaemia and Thalassaemia
52/61
Figure 11. Sickle cells (arrowed) and target cells.
Downloaded from: StudentConsult (on 4 March 2009 11:05 AM)
2005 Elsevier
Sickle Cell Disease
-
8/3/2019 Anaemia and Thalassaemia
53/61
Sickle Cell Anaemia
Vaso-occlusive crisis Precipitated by infections, hypoxia, cold, dehydration,
acidosis
Dactylitis (hand-foot syndrome), stroke
Acute anaemia
Splenic sequestration
Aplastic crisis
haemolysis Splenomegaly, priapism, infections
Long-term problems: retarded growth, leg ulcers,cardiomegaly, etc
-
8/3/2019 Anaemia and Thalassaemia
54/61
Sickle Cell Anaemia
Prophylaxis: immunizations, penicillin,avoidance of vaso-occlusive crisis
Treatment:
Acute crisis: analgesics, hydration,oxygen, antibiotics, exchange transfusion
Chronic problems: hydroxyurea, bonemarrow transplant
Haemol tic Disease of the
-
8/3/2019 Anaemia and Thalassaemia
55/61
Haemolytic Disease of the
Newborn
Due to feto-maternal incompatibility of redcell antigens:
ABO incompatibility
RhD incompatibility
Sensitization antibody production
Haemolytic anaemia of the newborn
Coombs test: positive
Management: neonatal jaundice
Autoimmune Haemolytic
-
8/3/2019 Anaemia and Thalassaemia
56/61
Autoimmune Haemolytic
Anaemia
Increased red cell destruction due to redcell autoantibodies
Idiopathic or secondary (autoimmune
disorders, malignancies, infections) Divided into:
Warm AIHA (37C, IgG)
Cold AIHA (
-
8/3/2019 Anaemia and Thalassaemia
57/61
Anaemia due to Blood Loss
In newborn:
Feto-maternal bleeding
Twin-twin transfusion
Perinatal blood loss e.g. placental abruption
Gastrointestinal bleeding
E.g. Meckels diverticulum
Inherited bleeding disorders
E.g. von Willebrands disease
-
8/3/2019 Anaemia and Thalassaemia
58/61
Thank You
-
8/3/2019 Anaemia and Thalassaemia
59/61
Classification of anaemia. MCV, mean corpuscular volume.
Downloaded from: StudentConsult (on 4 March 2009 11:05 AM)
2005 Elsevier
-
8/3/2019 Anaemia and Thalassaemia
60/61
Downloaded from: StudentConsult (on 4 March 2009 11:05 AM)
2005 Elsevier
-
8/3/2019 Anaemia and Thalassaemia
61/61
Antiglobulin (Coombs') tests. The anti-human globulin forms bridges between the sensitized cellscausing visible agglutination. The direct test detects patients' cells sensitized in vivo. The indirect