Assessment, pricing, and reimbursement of new health technologies: Innovative reimbursement models: Examples from health insurance systems in Asia Abdulkadir Keskinaslan, MD, MBA, MPH International Conference for Improving Use of Medicines – ICIUM 2011 Antalya,Turkey, November 17, 2011

Abdulkadir Keskinaslan , MD, MBA, MPH
Feb 01, 2016
Assessment, pricing, and reimbursement of new health technologies: Innovative reimbursement models: Examples from health insurance systems in Asia. Abdulkadir Keskinaslan , MD, MBA, MPH International Conference for Improving Use of Medicines – ICIUM 2011 Antalya,Turkey , November 17, 2011. - PowerPoint PPT Presentation
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

Assessment, pricing, and reimbursement of new health technologies: Innovative reimbursement models: Examples from health insurance systems in Asia
Abdulkadir Keskinaslan, MD, MBA, MPHInternational Conference for Improving Use of Medicines – ICIUM 2011Antalya,Turkey, November 17, 2011

Striking a Challenging Balance
Continued innovation
Household & system affordability
Appropriate use
Access to new medicines
2 | Innovative Reimbursement Models | Keskinaslan | 17 Nov 2011

In an increasingly cost-sensitive environment, it is becoming more difficult for highly-priced innovative drugs to gain reimbursement
Pharma is now moving towards a value-based pricing system, opting for risk-sharing in an effort to improve equitable access to effective care
Innovative pricing and patient access schemes are arrangements which may be used on an exceptional basis for the acquisition of medicines
The schemes are intended to improve the cost-effectiveness of a medicine and therefore allow HTA bodies to recommend treatments which they would otherwise have deemed not cost-effective
Source: Akehurst,Taiwan HTA Workshop 2010; de Pouvourville, EJHE, 2006
The underlying concept of innovative pricing and patient access schemes is value-based pricing
Risk-Sharing Agreement:
“A contract between two parties who agree to engage in a transaction in which there are uncertainties regardless concerning its final value. Nevertheless, one party, the company,
has sufficient confidence in its claims of either effectiveness or efficiency that it is ready to accept a reward or a penalty depending on the observed performance.”
3 | Innovative Reimbursement Models | Keskinaslan | 17 Nov 2011

From “Price Volume” and “Money Back” to Value Based Reimbursement: Non-linear pricing
Size of Patient segment or indication
Weighted Average Price
low
high Price-Volume Agreement assumes that “reimbursement buckets” are filled from left to right
Money-back Guarantee assumes binary outcome: full response or failure
Is it possible to devise a scheme, where all “buckets”! Are filled simultaneously, depending on patient characteristics (e.g. unmet need, risk, benefit)?
S1 S2 S3
P1
P2
P3
Average Price
4 | Innovative Reimbursement Models | Keskinaslan | 17 Nov 2011

Pricing models to improve access and affordability
Financial Utilization Models
Outcomes Based Pricing Models
Risk Based Pricing Models
Price volume agreement: e.g. full reimbursement for first 10% of patients, reduced reimbursement for next 20% of patients, no reimburse-ment for all others
Initial 10% of patients
Next 20% of patients
All others
Full response
Partial response
No response
Money back guarantee, e.g. full reimbursement for responders, reduced reimbursement for partial responders, no reimburse-ment for non-responders
High Risk
Moderate risk
Low risk
Reimbursement linked to value and level of risk factors (e.g. based on diagnostic test)
Patient segments Patient segments Patient segments
5 | Innovative Reimbursement Models | Keskinaslan | 17 Nov 2011

In 2008 NICE found Lucentis to be cost-effective for wet Age-Related Macular Degeneration (AMD) if a course of treatment did not exceed 14 injections
To ensure full patient access, Novartis agreed to pay for any injections of Lucentis that exceeded the 14 recommended by NICE
• Company covers the costs of additional injections
Results
Patients received effective innovative treatment
Improved cost effectiveness for the NHS
Lucentis became established as effective treatment in the market
Lucentis (ranibizumab) for AMD – UKPer patient, response-assumed, if longer treatment required, drug free of charge
Source: National Institute for Health and Clinical Excellence. Final Guidance: Ranibizumab and pegaptanib for age-related macular degeneration. http://guidance.nice.org.uk/TA155
Financial Utilization Models
6 | Innovative Reimbursement Models | Keskinaslan | 17 Nov 2011

Velcade (bortezomib) for multiple myeloma - UKPer patient, response dependent, cash refund
In 2006, Velcade treatment was considered ‘not cost-effective’• costs approx. £3,000 per treatment cycle (£38,000 per QALY).
Johnson & Johnson scheme proposed that treatment would be reimbursed only when effective• Full or partial response - remain on therapy and funded by NHS• minimal or no response - cease treatment and costs refunded to NHS by the
company
ICER with rebate, stopping rule after 4 cycles with partial and full responders continuing therapy: £20,700/QALY• Response assessed after max of 4 treatment cycles and response was measured
by tumor shrinkage - reduction in serum M-protein levels of 50% or more
• 60 day claim period
Outcomes Based Pricing Models
Source: A Keskinaslan, ISPOR Asia, Thailand September 5-7th, 2010
7 | Innovative Reimbursement Models | Keskinaslan | 17 Nov 2011

Actonel (risedronate) for osteoporosis – USPer patient, response dependent, pay for consequence
In 2009 Procter & Gamble and Sanofi-Aventis agreed the scheme with Health Alliance Medical Plans
A risk-sharing agreement where preventative treatment is assessed against unwanted disease outcomes• To pay for bone fractures occurring while the patient is taking Actonel.
• For these patients, any health costs associated with a non-spinal fracture to be covered by the manufacturing companies (estimated to cost between $6,000 and $30,000 per fracture, depending on the fracture location).
Patients qualify if they have no-comorbidity, no prior fractures etc; and have taken Actonel for six out of the nine most recent months
Intention of the scheme:• To reduce potential treatment costs for fracture treatment for patients on Actonel
• To provide an incentive to keep qualified patients on Actonel instead of switching to less-expensive generic alternatives
• To keep Actonel on a lower formulary tier than competition
Outcomes Based Pricing Models
Source: A Keskinaslan, ISPOR Asia, Thailand September 5-7th, 20108 | Innovative Reimbursement Models | Keskinaslan | 17 Nov 2011

Telbuvidine for chronic hepatitis B treatment - Australiaacceptable ICER across patient segments
Telbuvidine is indicated for the treatment of HBeAg-positive and HBeAg-negative chronic hepatitis B patients who have compensated liver disease, evidence of viral replication and active liver inflammation and who are nucleoside analogue naïve.
Telbuvidine priced at weighted average price across patient subgroups
• priced at a high but acceptable incremental cost effectiveness ratio compared to lamivudine for HBeAg-positive (e-pos) patients
• priced higher than lamivudine for HBeAg-negative patients based on cost-offsets due to reduced resistance rates and thus lower use of more expensive 2nd-line adefovir
Risk Based Pricing Models
Source: http://www.health.gov.au/internet/main/publishing.nsf/Content/pbac-psd-telbivudine-mar08; www.novartis.com.au/DownloadFile.aspx?t=p&f=seb.pdf&dateid
9 | Innovative Reimbursement Models | Keskinaslan | 17 Nov 2011

The underlying concept of patient access schemes is no different from innovative pricing schemes: value-based pricing
Willingness to Pay BasedPricing Models
Affordability BasedPricing Models
Loyalty Card: e.g. progressive discounted price for members, additional reward for compliant patients (4+1), value added services (free routine tests) for long term compliant patients
Discount for members
Price or free goods reward for compliance
Value added servicesfor compliant patients
Patient Assistance Program, e.g. Patients pay what they can afford, governments or private insurance companies may contribute
Patient segments Patient segments
Full price
Partial price
No price
10 | Innovative Reimbursement Models | Keskinaslan | 17 Nov 2011

NOA providing Glivec (imatinib) for CML - Indonesia Affordability based model, shared contribution
Novartis Oncology Access (NOA) designed to bridge the affordability gap in Indonesia
NOA offers patients to pay what they can afford, based on a financial evaluation – to bridge the affordability gap.• Co Pay Model Based on the “Cost of Living Wages” (CoL)
• Patient’s financial resources do not fall under 2 X CoL after purchasing Glivec
• 7 tier scheme determined through assessment made by financial agency; in December, 2010: 305 patients
Multiple Stakeholders involved in setting up the program• Ministry of Health Indonesia
• Indonesian Society of Hematology and Blood Transfusion
• Indonesian Hematology and Internal Medicine Medical Oncology National Working Group
• Indonesian Cancer Foundation, Jakarta Branch
• Financial assessment by PT Survindo Putra Pratama
• Novartis Indonesia
Patient segments
Full price
Partial price
No price
Affordability BasedPricing Models
11 | Innovative Reimbursement Models | Keskinaslan | 17 Nov 2011

Novartis introducing MUSANDA Program, a patient access & affordability program which enables ophthalmologist to treat a segment of patients that was left with no treatment
Program helps patients with funding gap and creates a financing option for self-pay patients
It helps restoring sight and prevent blinds & visual impairment for AMD/DME patients
Program also offers discounted fees for patients at affiliated clinics and hospitals
3rd party conducts financial assessment to identify eligibility for different level of support
Lucentis (ranibizumab) for AMD – UAE Affordability based model with shared contribution
Patient segments
Patient Purchase
Partial price for all segments
Affordability BasedPricing Models
12 | Innovative Reimbursement Models | Keskinaslan | 17 Nov 2011

Musanada program designed to help patients with no access
Affordability barrierNo Access
Patients wAMD & DME for MUSANADA program :
13 | Innovative Reimbursement Models | Keskinaslan | 17 Nov 2011

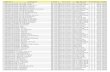
Examples of Estimated ICER Thresholds
Unit Lower boundary Upper boundary
USA QALY US$50,000 US$100,000
Canada QALY US$17,600 US$87,800
Australia LYG US$28,200 US$51,000
UK QALY US$32,000 US$48,000
Thailand QALY ~US$2,000 ~US$8,000
Unit Lower boundary Upper boundary
WHO GDP/capita/DALY averted <3
Australia PBAC
GDP/capita/life-year gained
1.26 2.29
UK NICE GDP/capita/QALY 1.4 2.1
ICER = incremental cost-effectiveness ratio; QALY = quality-adjusted life-year; LYG = life-years gained;GDP = gross domestic product; WHO = World Health Organization; DALY = disability adjusted life-years; NICE = National Institute for Clinical Excellence (UK); PBAC = Pharmaceutical Benefits Advisory Committee Value in Health 2004;7:518
If the ICER is within a defined acceptable range (threshold) by the payer/ provider of healthcare, then there is a high likelihood that the treatment could be accepted
15 | Innovative Reimbursement Models | Keskinaslan | 17 Nov 2011
Related Documents